To understand the perspectives of infectious disease residents and their preceptors on teaching radiology in medical residency programmes in this speciality. The aim is to support the creation of a strategy to facilitate teaching and promote learning within the competency matrix, given the expanding role of diagnostic imaging methods in medicine. Thus, knowledge of radiology is an increasingly useful tool for professional practice in the area of infectious diseases.
Material and methodsThis is a qualitative, exploratory investigation in which semi-structured interviews were conducted with resident physicians and preceptors of a medical residency programme in infectious diseases according to the paradigmatic approach of Foucault’s discourse analysis.
ResultsBased on analysis of the interviews, the following central points are considered in developing a strategy to teach radiology in the medical residency programme in infectious diseases: understanding of the vocabulary used in radiology, development of good communication skills with radiologists, optimising the time dedicated to learning radiology, the correlation between aspects of radiology and anatomical pathology, as well as the systematisation of a teaching process.
ConclusionThe appreciation for peer education and case discussions, particularly with a radiologist integrated into the medical residency team, indicate that these are the measures with the greatest potential to facilitate teaching and promote learning.
Comprender las perspectivas de los residentes de enfermedades infecciosas y sus preceptores sobre la enseñanza de la radiología en los programas de residencia médica en esta especialidad. El objetivo es apoyar la creación de una estrategia para facilitar la enseñanza y promover el aprendizaje dentro de la matriz de competencias, dado el papel cada vez mayor de los métodos de diagnóstico por imagen en la medicina. Por lo tanto, el conocimiento de la radiología es una herramienta cada vez más útil para la práctica profesional en el área de las enfermedades infecciosas.
Material y métodoSe trata de una investigación cualitativa y exploratoria en la que se realizaron entrevistas semiestructuradas a médicos residentes y preceptores de un programa de residencia médica en enfermedades infecciosas según el enfoque paradigmático del análisis del discurso de Foucault.
ResultadosA partir del análisis de las entrevistas, se consideran los siguientes puntos centrales en el desarrollo de una estrategia para enseñar radiología en el programa de residencia médica en enfermedades infecciosas: comprensión del vocabulario utilizado en radiología, desarrollo de buenas habilidades de comunicación con radiólogos, optimización del tiempo dedicado al aprendizaje de radiología, correlación entre aspectos de radiología y anatomía patológica, así como la sistematización de un proceso de enseñanza.
ConclusiónEl aprecio por la educación entre pares y las discusiones de casos, particularmente con un radiólogo integrado en el equipo de residencia médica, indican que estas son las medidas con mayor potencial para facilitar la enseñanza y promover el aprendizaje.
Knowledge on radiology is essential to the practice of modern medicine in various clinical and surgical specialties. It is therefore a relevant subject in the competency matrix of medical residency programmes as medical devices for diagnosis by complementary imaging methods are increasingly developed and incorporate technological advances, especially those of computer science, to medicine.1
Teaching radiology in medical residencies in infectious diseases has certain peculiarities since working in this area requires an understanding of diagnostic imaging strategies in pathologies of various human organs and systems, unlike several medical specialities where the area of interest is restricted to a particular organ or system.2–4
Learning such diverse concepts, techniques, and imaging patterns requires a coherent, well-planned, and well-structured approach so that it does not occupy time that is incompatible with the duration of the training programme. Accordingly, it is important to expand learning in radiology in medical residency programmes in infectious diseases by adopting a strategy that facilitates its integration into the competency matrix, to boost cognition and promote more consistent teaching in both theory and practice.5–7
In Brazil, there is no uniformity in terms of the academic role attributed to learning complementary diagnostic imaging methods in medical residency programmes in infectious diseases. However, as there is no established normative standard, the discussion over developing a strategy to teach radiology in specialised training programmes in infectious diseases remains open.4
Central points to learning radiology throughout medical residency programmes in various specialties include patient safety, training to appropriately choice of complementary exams and understanding the different terms used in radiologists' reports.8,9
The resident physician also needs to understand how medical images are interpreted by radiologists in the field of infectious diseases as it depends on the time of disease progression, varies with the patient’s immunological status, and is subject to pattern modifications resulting from the introduction of therapeutics. Thus, this information needs to be reported accurately by the requesting physician so as not to compromise the examination report. Additionally, the infectious disease physician must be aware of the importance of interpreting radiological findings as markers for the emergence of new diseases or forms of progression of infectious diseases that have never been described, as observed with COVID-19.10
Since it involves broad cognitive, ethical, and economic aspects, teaching radiology to infectious disease residents is no simple task. Nevertheless, due to the incorporation of the concepts of interdisciplinarity and transdisciplinarity in medical education, knowledge on imaging methods in medicine is more easily acquired when it relates to understanding the pathophysiology of diseases. As a result, proposals for teaching radiology have included the joint study of clinical, laboratory, anatomopathological, and radiological approaches for resident physicians.11–17
Another factor contributing to successfully teaching radiology in medical residencies is respect for how adults learn. Under the perspective of andragogy, the participation of resident physicians and preceptors in creating a teaching strategy with specific, measurable, achievable, relevant learning objectives that are compatible with the schedule needs to take the particularities of the residency programme and its participants into account.13
As teaching and learning strategies tend to fail significantly when they disregard the perspective of those involved, it is necessary to conduct research that sets out to clarify the viewpoint of resident physicians and preceptors.10,13–17
In the area of infectious diseases, there are no publications discussing the residents’ and preceptors’ views on the learning process in radiology or the development of a specific strategy focused on teaching radiodiagnosis in this field. Other specialties have developed concrete initiatives in this respect for decades, namely pulmonology.2,3,6,18,19
The idea of aligning medical residency programmes in infectious diseases with teaching strategies that have been successfully tested in the training of radiologists is potentially valuable for improving the way radiology is handled by residents and preceptors. Other medical specialties that have promoted the introduction of teaching radiology in a structured manner have reported positive experiences.2,16
Based on the results of qualitative research, the current study presents a strategic model to incorporate radiology in medical residency programmes in infectious diseases considering the perspectives of preceptors and resident physicians on the teaching and learning process.
Material and methodsThis qualitative study was developed at the teaching hospital of a Brazilian Federal University, with a medical residency programme in infectious diseases.
Data collection occurred between October 2019 and January 2020. Semi-structured interviews were conducted in person and lasted approximately 30 minutes. They consisted of three open-ended questions that the interviewee could answer freely.
The questions inquired about the role of radiology in the practice of the infectious disease specialty, how this knowledge is constructed within the scope of medical residency, and the space that radiology should occupy within the resident’s competency matrix.
The interviewer was the principal investigator, an instructor, radiologist, and full member of the Brazilian College of Radiology. A second investigator, a professor and pathologist also affiliated with the Tropical Medicine Center of the Federal University of Pará in the area of medical education, analysed the data separately. The analysis of the Second Investigator's reliability from the other point of view guarantees the diversity of meanings expressed by the interlocutors.
All the interviews occurred in a reserved room at the facilities of the medical residency programme in infectious diseases, recorded in audio and later transcribed in full by the principal investigator, kept in a safe place, in anonymity.
The paradigmatic approach of Foucault’s discourse analysis was adopted as it does not propose to investigate ‘what lies behind’ or ‘what is meant’ by texts and documents. It reveals the conditions of existence for a particular discourse and the central idea in the answers to the open-ended questions.20
Participants included all resident physicians and preceptors of the hospital’s medical residency programme in infectious diseases, 11 preceptors and 9 resident physicians of both sexes between the ages of 25 and 50 years who had completed their undergraduate studies in medicine between 1 and 26 years ago.
A characterisation of the research subjects is necessary because, in the paradigm of Foucault’s discourse analysis, the idea expressed in the response is tied to hierarchy and culture. Discourse is not a kind of metaphysical entity constructed a priori to other elements of society.20
All the researchers codified the material extracted from the interviews individually and then analysed it together until they agreed on the definitive names for the themes extracted from the interviews, based on the criteria for best practices in qualitative research.21
A summary of the procedural steps of the methodology is presented in Table 1,22 and the characterisation of the research subjects are outlined in Table 2. The themes extracted from each interview are listed in Table 3.
Procedural Steps22
| Steps | Description |
|---|---|
| 1. Obtain ‘raw’ data | Complete records of audio and transcripts |
| 2. ‘Dip’ into each record | Listening and reading records individually to identify core meanings in the subjects’ answers |
| 3. Categorisation | Each researcher institutes the categories based on their own analysis |
| 4. Gather the themes or types reported for each category | After the researchers analysed each interview, exemplary statements were highlighted according to the central idea identified |
| 5. Codify or name the data | Name the themes reported for each category |
| 6. Allocate (in a table) the themes and types of statements | The table demonstrates the results and facilitates interpretation |
Characterisation of the research subjects
| Interviews | Sex | Age | Time elapsed since completion of undergraduate studies in Medicine | Position |
|---|---|---|---|---|
| Interview 1 | Male | 33 years | 7 years | R1 |
| Interview 2 | Female | 28 years | 1 year | R1 |
| Interview 3 | Female | 25 years | 2 years | R1 |
| Interview 4 | Male | 27 years | 2 years | R2 |
| Interview 5 | Female | 27 years | 2 years | R2 |
| Interview 6 | Female | 27 years | 2 years | R2 |
| Interview 7 | Female | 29 years | 3 years | R3 |
| Interview 8 | Female | 28 years | 3 years | R3 |
| Interview 9 | Female | 29 years | 4 years | R3 |
| Interview 10 | Female | 30 years | 8 years | PRECEPTOR |
| Interview 11 | Male | 40 years | 16 years | PRECEPTOR |
| Interview 12 | Female | 50 years | 25 years | PRECEPTOR |
| Interview 13 | Female | 44 years | 20 years | PRECEPTOR |
| Interview 14 | Female | 46 years | 21 years | PRECEPTOR |
| Interview 15 | Male | 30 years | 7 years | PRECEPTOR |
| Interview 16 | Female | 50 years | 26 years | PRECEPTOR |
| Interview 17 | Female | 44 years | 19 years | PRECEPTOR |
| Interview 18 | Female | 33 years | 7 years | PRECEPTOR |
| Interview 19 | Female | 32 years | 6 years | PRECEPTOR |
| Interview 20 | Female | 31 years | 6 years | PRECEPTOR |
Stated themes
| Issues | E1 | E2 | E3 | E4 | E5 | E6 | E7 | E8 | E9 | E10 | E11 | E12 | E13 | E14 | E15 | E16 | E17 | E18 | E19 | E20 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Learning barriers and facilitators | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Teaching methodology | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Assessment for learning | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | ||
| Additional themes | ||||||||||||||||||||
| Use of digital tools and social networks | X | X | X | X | X | X | X | X | X | X | X | X | X | |||||||
| Scientific research in the area of infectious diseases and radiology | X | X | X | X | X | X | X | X | X | X | X | X |
The qualitative study identified four main themes in the interviewees’ statements (see Table 3): barriers and facilitators to learning radiology in the medical residency programme in infectious diseases, issues related to teaching methodologies, assessment for learning, and two additional themes, the use of digital tools and social networks as learning tools and the role of scientific research in the area of infectious diseases and radiology as a promoter of knowledge.
The participants asserted that poor assimilation of vocabulary utilised in each method (radiology, magnetic resonance imaging, ultrasonography, etc.) and difficulties in correlating radiology, clinical aspects, pathology, and other exams.
Another relevant aspect is time management. The space reserved for teaching radiology is easily invaded, particularly when there are complications in both outpatient and inpatient care, and there is no specific plan to avoid compromising the regularity of teaching and learning activities.
The residents reported that they also seek to learn radiology in a ‘simpler’, ‘more accessible’ way. A broad, in-depth study of diagnostic imaging is not common. For this reason, the residents value teaching and learning among themselves (peer education), quick consultations on the internet, and good communication with radiologists.
As for teaching methodologies, the adoption of several tools, such as case studies structured in the correlation between clinical practice and radiology, discussions over scientific papers, or even thematic conferences, was recognised as beneficial in the statements.
The interviewees mentioned informal peer education and case discussions with radiologists as fundamental elements of promoting consistent learning; however, they perceived the lack of a systematised approach as a problem.
Discussing the exams of both the outpatients and inpatients associated with the medical residency programme in infectious diseases brings ongoing cases to the agenda. They are often repetitive and focus on resolving the patient’s problem. The approach is rarely expanded to issues such as which investigation methods to choose, differential diagnoses, or radiological semiology, thus compromising the development of adequate clinical-morphological reasoning and interpretative abilities before unusual medical situations.
The assessment for learning emerged as a theme from the perspective of both the need for assessment and well-defined assessment criteria relative to the residents’ progress over the course of the programme.
Both the preceptors and residents recognise the value of learning from mistakes and critical reflection, which means that thorough feedback is indispensable.
As for the assessment criteria used to evaluate the residents’ progress, all interviewees noted that the assessment process considers how residents utilise complementary diagnostic imaging tests in different aspects: from the way they prepare examination requests to their capability of having a dialogue with the radiologist about imaging findings. They also presented the idea that learning radiology means being capable of proposing a feasible diagnostic hypothesis before a radiological finding in a given clinical context and that this competency is subject to evaluation.
Some additional themes emerged from the interviews and are noteworthy for their relevance as subjects of significant educational transversality: the use of digital tools and social networks as learning tools and the role of scientific research in infectious diseases and radiology.
The search for content with medical images on Instagram has also gained prominence, but the use of video lessons on YouTube is indicated as a quick and accessible tool.
Scientific research in the area of infectious diseases and radiology is perceived as a potential source of learning by preceptors who have encouraged residents to engage in scientific production.
Themes, sub-themes and exemplary statements are exposed in Table 4.
Results: themes, sub-themes and exemplary statements
| Themes | Sub-themes and Additional themes | Exemplary statements |
|---|---|---|
| Learning barriers and facilitators | Learning specific vocabulary and technical terms | E2: ‘I find it difficult to read texts on radiology because of the specific vocabulary used, those hypoechoic, hyperdense, hypodense terms. I stumble with that sometimes. The names of the radiological signs are also hard for me. We saw little radiology in college’. |
| Available, dedicated time | E4: ‘I understand radiology papers about infectious diseases well now, before I did not. It took me a long time to familiarise myself with the terms’. | |
| E7: ‘Time is short. I save time by asking my colleagues when I don't know something, or I look it up on the internet’. | ||
| Rapport with the team of radiologists | ||
| E9: ‘When there are many intercurrences in the section, it is easy to cancel the radiology meeting’. | ||
| E9: ‘Sometimes the radiologist does not offer us more help, because we do not provide a good clinical history. When I go and talk to them, I get better results. I also know that there are things that they do not want to state in the report, but they will in an informal conversation’. | ||
| E14: ‘It would be difficult without discussions with the radiologist. Even to decide which exam is more appropriate, it is always good to talk to them’. | ||
| Teaching methodology | Peer education | E2: ‘R2 and R3 help a lot by sparking the discussion over topics in radiology, but they are few. There is only one R1 working in one ward, while R2 is working in another. So, sometimes we have little contact’. |
| Formal radiological session | E3: ‘I think that one learns more by discussing cases with fellow residents, preceptors, and radiologists on a daily basis’. | |
| E1: ‘The case discussions are great in the residency programme, but nothing is systematised, because you discuss routine cases randomly. There is a lack of continuity’. | ||
| E10: ‘In radiology meetings, we address inpatients, and the cases are very repetitive in the routine. We end up seeing only a narrow range of diseases. The main point is to refer the patient’s case to find a solution to a certain diagnostic problem’. | ||
| Assessment for learning | Need for assessment | E11: ‘I believe that if educational efforts are made to teach radiology, it will require an assessment for learning’. |
| Assessment criteria | E13: ‘Feedback has to be given to the resident’. | |
| E6: ‘I think that the best criterion for assessing learning is verifying the appropriate development of diagnostic hypotheses’. | ||
| E17: ‘It is reductionist to evaluate the resident only by the correct interpretation of an image. More things need to be considered: deciding which modality of complementary exams to choose and the ability to defend a diagnostic hypothesis’. | ||
| Additional themes | Use of digital tools and social networksScientific research in the | E1: ‘We have a WhatsApp group, and people help each other when questions arise’. |
| area of infectious diseases and radiology | ||
| E5: ‘I look it up on YouTube. It’s fast’. | ||
| E11: ‘I learned a lot about radiology by publishing scientific papers’. | ||
| E12: ‘Since most of the scientific papers we produce here at the hospital end up presenting radiological images, I think that research could arouse interest in radiology in infectious diseases’. |
The rapid technological development of radiology and the growing relevance of imaging exams for a fast, accurate diagnosis, which offer safe decision-making in clinical and surgical procedures, pose a new challenge to medical educators. Learning radiology demands support among infectious disease specialists in training through the application of strategies based on the pedagogical tools available.1,16,23–26
Given the results of this study, the main barriers to rapidly learning radiology for infectious diseases resident physicians include difficulties in understanding the technical terms utilised in books and scientific papers about diagnostic imaging and examination reports. Thus, the importance of aligning undergraduate and postgraduate education by strengthening the discipline of radiology in the medical programme, as a diagnostic method and tool for learning about normal anatomy and anatomical pathology. Nevertheless, it is convenient to implement a strong review of the basic concepts of anatomy, pathology, and radiology in the medical residency programme in infectious diseases in its first year.5–8,11,23
Good communication with the radiologists affiliated with the hospital hosting the residency programme in infectious diseases was indicated as a facilitator for learning. In this sense, the collaborative relationships among professionals across different areas and the ability to work in teams were seen as positive by the interviewees, especially concerning radiology services.2,3,5,6,15
As for the methodological aspects, a considerable amount of teaching in a medical residency programme occurs in the workplace. The growing complexity of health problems has required innovative teaching methods that promote medical specialisation technically and in its social, cultural, and academic/scientific roles and is in dialogue with undergraduate education. To then, align the methods applied, develop innovative ideas, and evaluate their results.10,11,13–17,23–25
As reported in the interviews, peer education and informality are prevalent, especially among the residents. Medical residents have a growing responsibility to educate their peers and serve as the primary instructors for medical students in the undergraduate internship programme, but this requires close, dedicated supervision.25,26
Regarding the existence of formal meetings between radiology and infectious diseases with an educational emphasis, experiences in the teaching of radiology in undergraduate programmes in medicine and residency programmes in radiology and other specialities indicate that these sessions must promote meaningful learning in which the constructed knowledge by the interaction of the participants in person, offer an experience different from that obtained through electronic means. It also requires discipline with attendance and a set time to begin and end, a good selection of the subjects or clinical cases studied, and productive discussion over questions conducted by a professional with expertise in the subject, who understands which educational objectives must be met.17,27–30
Although residents prefer educational activities in which they may freely engage in dialogue, conference series shouldn't be downgraded in medical residency programmes. A lecture series oriented by radiologists in a paediatric residency programme contributed to the residents’ understanding of proper classification practices for choosing exams and radiation risk. The radiologist’s participation in the paediatric residents’ training was positive, thus demonstrating its applicability to the residency programme in infectious diseases.3 We can also consider that virtual activities have been successful in enabling distance education and being able to revisit the content several times.27,28
The interviewees, both preceptors and residents, admitted to the need for an assessment for learning in radiology for the infectious disease resident physicians.
As reported in the literature, those in training use the feedback from their preceptor to reflect on their learning. This is why preceptors and residents interviewed considered feedback to be essential.5,24,25
Additional themes such as the use of digital tools and social networks as learning instruments and the role of scientific research in infectious diseases and radiology were recurrent in several interviews.
In addition to producing new knowledge, scientific research generates consistent collateral learning of various subjects for those who conduct it, as research and publication require reading, reflection, and elaborating integrative syntheses.
The use of digital tools and social networks as learning instruments is a widely studied phenomenon in the literature. The use of social networks in medical education has reshaped teaching and learning. The most relevant tool mentioned is the video-sharing site YouTube, but other networks and messaging applications are also used, especially WhatsApp.28
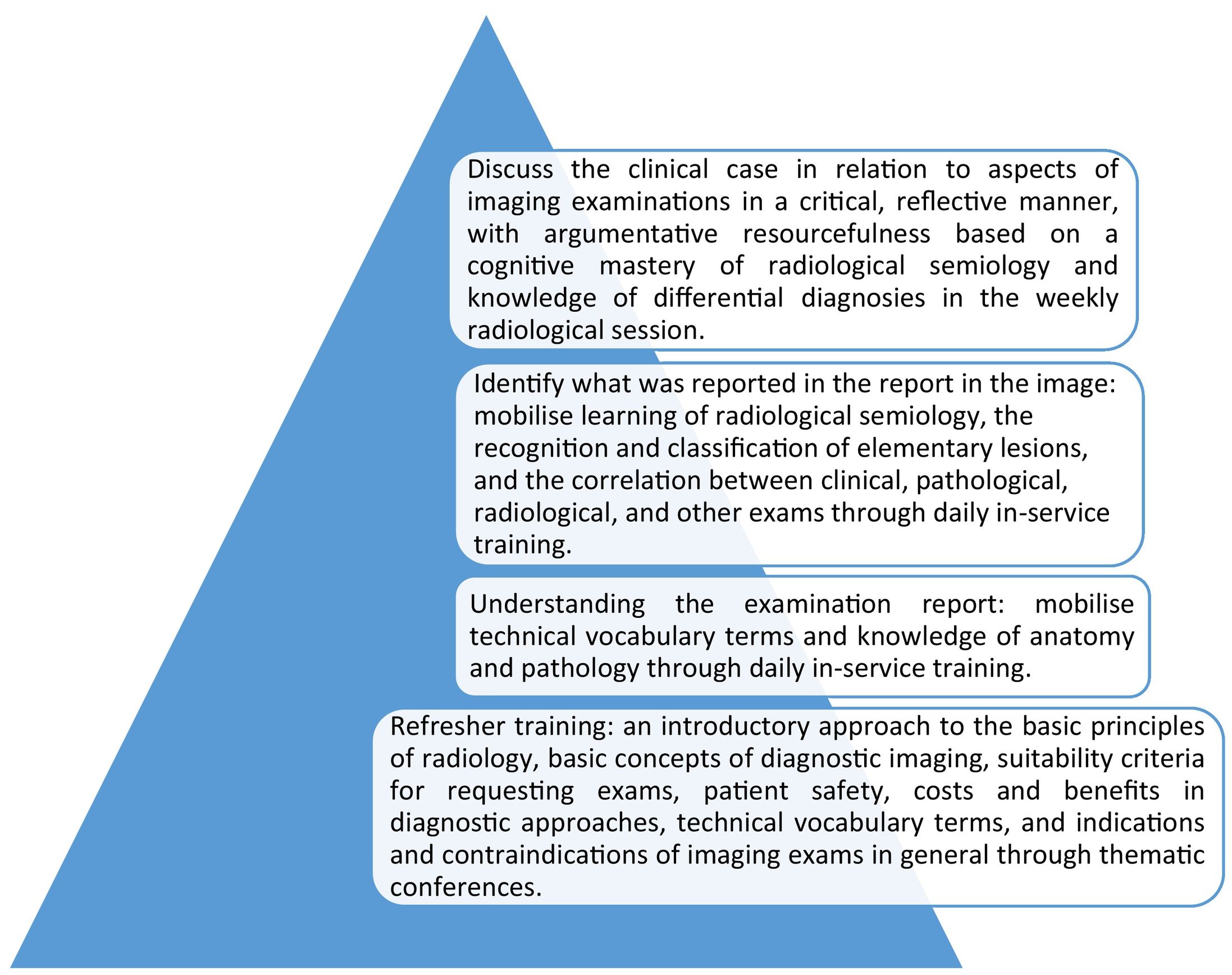
From the results under discussion we propose that in the first semester of medical residency, radiology in infectious diseases would then be introduced with three educational objectives: understanding the examination report, identifying what was reported regarding the image, and the ability to discuss a case in a critical, reflective manner by raising questions and correlating the reports and images with clinical aspects and results from other exams.
To achieve the competencies, the strategy requires a strong collaborative relationship with the radiology department and its physicians in two modalities: a daily visit to discuss the exams of outpatients and inpatients seen by the medical residency team and a formal, weekly radiological session with a standard duration of 50 minutes on a pre-established day and time.
The objective of this meeting will be to resolve questions regarding current patients and provide an educational approach that may involve dialogue lectures, team-based learning, the discussion of structured cases from the service’s own archive, and the study of papers on infectious disease radiology.
The educational aspects discussed can be approached in three ways: i) beginning from the radiological aspect or imaging finding to a differential diagnosis of the diseases responsible for this pattern, whether they are infectious or not, ii) beginning from the disease and contemplating the distinct involvement in various organs and systems, iii) or beginning from the clinical condition and exploring a diagnostic strategy for that particular situation.8
The number of cases discussed should be as large as possible since research suggests that residents who analyse more cases are likely to demonstrate greater knowledge, thus highlighting the utility of case volumes as a prognostic marker of the residents’ success. Consequently, building an image archive with good documentation of the exams is necessary for a medical residency programme in infectious diseases.29,30
Learning must be assessed daily by preceptors and the radiologists involved in the medical residency programme through the residents’ exercise of the competencies listed in the learning objectives.15,16
Since the study was conducted in a medical residency service in infectious diseases, potential generalisations should be viewed with caution.
The subjectivity in qualitative research is part of a complex debate on the nature of the knowledge produced by this type of research. Nonetheless, it is possible to affirm that incorporating the perspective of resident physicians and preceptors, as exposed in the interviews and within the paradigm of Foucault’s discourse analysis, supports the development of a strategic vision for the teaching and learning process in radiology in the aforementioned medical residency programme. Their viewpoint exposes the barriers, facilitating aspects, and questions related to teaching methodologies and the assessment for learning.
Fig. 1 synthetically outlines a strategic proposal for successfully teaching and learning radiology in medical residency programmes in infectious diseases. It relates the learning objectives to the measures proposed to achieve them.
ConclusionThe core of the objectives of a proposed strategy for the inclusion of radiology in the competency matrix of the medical residency programme in infectious diseases should constitute the following abilities: to understand the examination report, to identify what was reported in the report in the image, and to discuss the case in a critical, reflective manner by correlating clinical aspects and the examination results.
Based on the results of this study, the appreciation for peer education and case discussions, especially when the radiologist is integrated into the medical residency team, indicates that these measures demonstrate the greatest potential to promote learning.
Ethical responsibilitiesThis research was approved by the Research Ethics of the UEPA - Universidade do Estado do Pará - Centre for Biological and Health Sciences. Certificate of Presentation of Ethical Appreciation number 14748819.9.0000.5174.