Family-Planning services should ideally be offered to any person who is of reproductive age, but when health personnel are not properly trained, the counselling can become suboptimal especially to patients at higher reproductive risk. The use of simulators of human patients and the use of simulation with standardised patients has shown to be useful in improving learning and communication attitudes, as well as reinforcing theoretical learning of medical students. To our knowledge, its use in producing skills in Family Planning and the counselling of contraceptive methods has not yet been sufficiently explored.
ObjectiveTo evaluate a simulation-based contraceptive counselling learning strategy for medical students to improve the skills involved in counselling of Family-Planning methods.
MethodsExploratory, mixed-method study consisting of three groups of medical students.
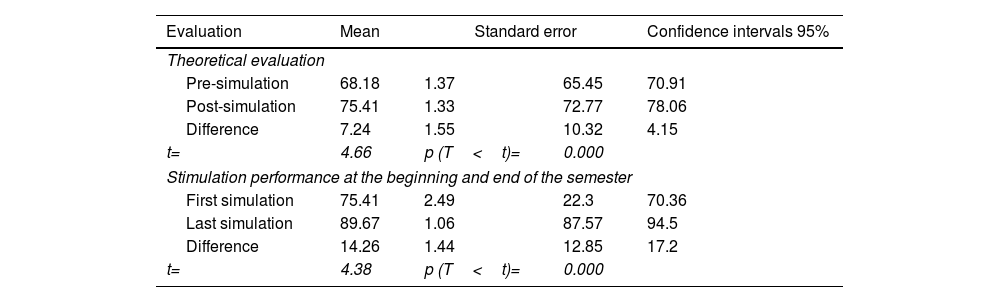
ResultsThe theoretical knowledge of the students increased by 7.24 points, while in the analysis of the performance in the simulation performed at the beginning and end of the semester, a significant increase of 14.26 points was observed.
DiscussionThe use of a simulation centre and standardised patients in a carefully represented environment favoured a meaningful learning. It also improved personalised counselling and strengthened the communications skills of medical students.
Los servicios de planificación familiar deben ofrecerse a cualquier persona en edad reproductiva, pero si el personal de salud no está debidamente capacitado, su asesoramiento puede ser subóptimo, especialmente para las pacientes con mayor riesgo reproductivo. El uso de simuladores humanos, y el uso de simulación con pacientes estandarizados, ha demostrado ser útil en la generación de aprendizaje actitudinal y comunicativo de estudiantes de medicina, pero a nuestro entender, su utilidad en la generación de competencias para métodos anticonceptivos y consejería de planificación familiar aún no ha sido implementada.
ObjetivoEvaluar una estrategia de aprendizaje de consejería anticonceptiva para estudiantes de medicina basada en simulación para mejorar las competencias involucradas en la orientación sobre los métodos de planificación familiar.
MétodosEstudio exploratorio con enfoque metodológico mixto, conformado por 3 grupos de estudiantes universitarios de medicina.
ResultadosEl conocimiento teórico de los estudiantes aumentó 7,24 puntos, mientras que en el análisis del desempeño en la simulación realizada al inicio y al final del semestre se observó un aumento significativo de 14,26 puntos.
DiscusiónEl empleo de un centro de simulación, pacientes estandarizados en un entorno cuidadosamente representado favoreció un aprendizaje significativo y facilitó el asesoramiento personalizado y fortaleció las habilidades de comunicación de los estudiantes de medicina de pregrado.
Family-Planning involves a process of free and conscious decision making regarding whether to reproduce and have children, the size of a family and the birth spacing thru the informed and responsible use of contraceptive methods.1–3 Family-Planning contributes to social development and linked to improve gender equity and economic independence.2–4 Decision making is influenced by the known and available options to meet the reproductive needs. Family-Planning relies in part on the communication skills and attitudes of the healthcare providers who are involved in counselling.
Mexico experienced a reduction in birth-rates over the last ten years, but Family-Planning programmes still have targets to reach. In 2016, 17.8% of all births were from adolescent mothers2,5 and over 20% of all adolescent pregnancies were subsequent.6 The proportion of women who used emergency contraception had a ten-fold increase,7 this phenomenon could be related to a suboptimal Family-Planning. The freedom to choose a specific contraceptive method may be limited by patients’ comprehension of the right use and risks that may derive from employing it, particularly by patients with chronic underlying diseases, anatomic anomalies or under particular conditions related to their lifestyle, reproductive antecedents and even psychological or social risk in certain cultural or religious contexts.3,8 National regulations stipulate that medical doctors should implement Family-Planning counselling thus; it is pertinent to implement educational strategies aiming medical students.9
Patient simulators and standardised patients constitute an efficient learning strategy in health education10,11 and medical training,12,13 but to our knowledge, simulation-based strategies have not been implemented in Family-Planning counselling. The objective of the present study was the evaluation of a simulation-based learning activity to improve theoretical learning of Family-Planning, especially centred on the development of medical students.
Materials and methodsLearning activities- 1.
Theoretical content of contraceptive use and Family-Planning medical counselling was explained during three-hour sessions.
- 2.
Clinical cases were analysed in learning sessions, considering the indications, recommendations and contraindications.
- 3.
The simulation-based learning activities included three different situations:
- i.
Patient admitted for delivery or caesarean section.
- ii.
Patient pre-/post-obstetric event.
- iii.
Non-pregnant patient in ambulatory medical consultation.
Methodological description. Situations i and ii were assigned to a hospital bed scenario with a simulator (manikin), an evaluator and a standardised family-member. Situation iii involved the use of a simulated ambulatory clinic, with a standardised patient and a family member in addition to an evaluator. Scenarios were set at the Montagne Medical Simulation Centre.
Each student participated in six different cases throughout the six-month course. Cases were randomly assigned. For every case, patients’ clinical history, sociodemographic characteristics and timing of counselling varied.
Instructors chose for every case, firstly, the hospital bed or clinic scenario and the situation to represent, and secondly, specifications from three different lists: (a) a list of patients’ features and clinical conditions, (b) a list of different sociodemographic variants and lastly, (c) a list of sexual, reproductive and gynaeco-obstetrical antecedents. Standardised-family-members changed roles as desired; defining, according to each case, whether to be spouses, parents, sexual partners or not to play a role in that case.
Thus, each case represented a combination of situations and patients, these combinations added randomisation and singularity to each case. Students were asked to provide a patient-based Family-Planning counselling considering the patient's specific characteristics and antecedents. In each simulations practice, students were evaluated by instructors using a 30-item previously validated checklist.
Perceived performance, theoretical and cognitive learning were evaluated after the first and last simulations. Perceived performance questionnaire included (a) usefulness, (b) fondness, (c) self-perceived performance, (d) clinical implication of the simulation in a 1–5 scale. Theoretical and cognitive learning included definitions, concepts, contraceptive indications and contraceptive pharmacological aspects along with risk assessment and case-based questions. Students’ qualitative opinions were retrieved and analysed at the end of the course.
Research design. Exploratory quasi-experimental study, in which intervention was based on situated cognition and problem-based-learning educational paradigms. A concurrent mixed method was used whilst qualitative and quantitative information was collected simultaneously.14
Qualitative analysisA conceptual tree was generated to identify related concepts15 expressed by students in their discourses and presented verbatim.
Quantitative analysis. The descriptive statistics of the sociodemographic variables were obtained from questionnaires, evaluations prior to and following the first and last simulations and from the performance during the simulation-based learning activity scores were obtained. Comparison tests were applied with statistical significance of p<0.05 to evaluate competence and learning changes. A linear regression model was constructed associating the scores obtained with characteristics of the participating students. The model selection was based on the maximum likelihood and variance.
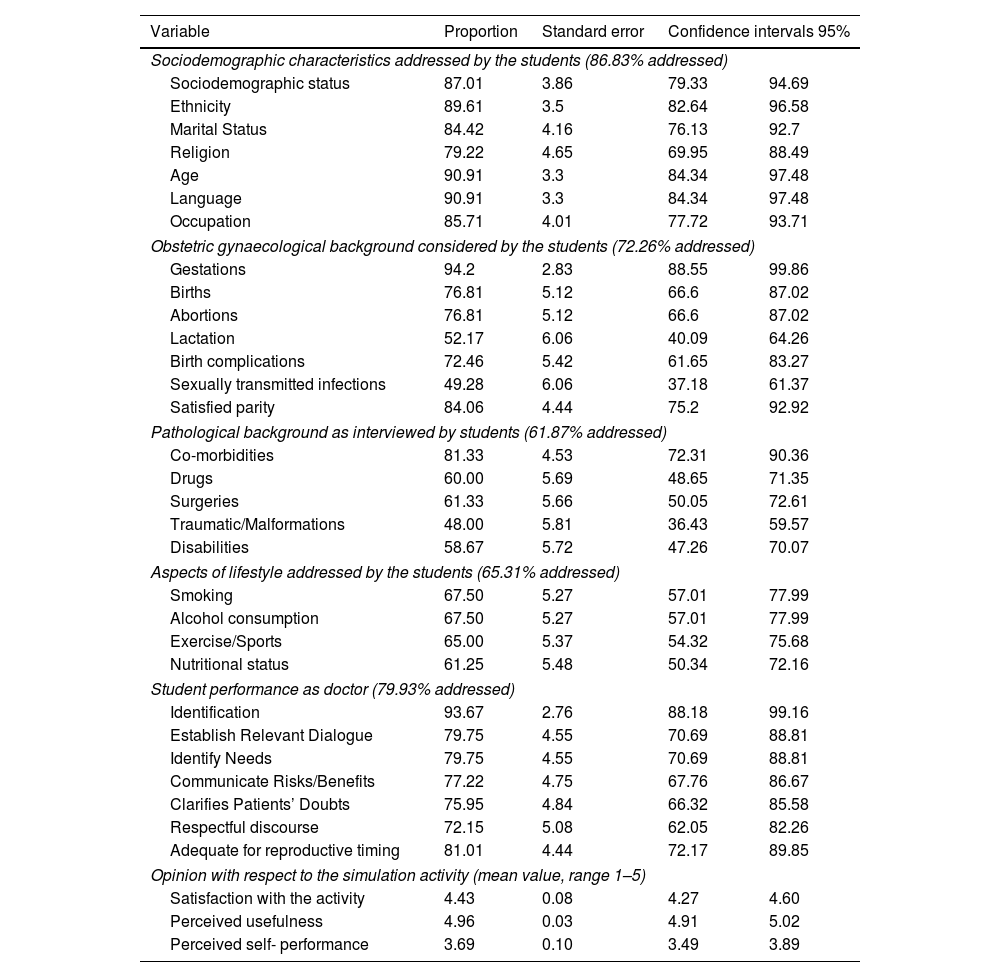
Results83 third-year students (average age 20.8 years) participated in the study, their performance their average performance in Family-Planning counselling simulation is presented in Table 1. Although their self-perceived performance was lower than hetero-evaluations, students acknowledged the usefulness and the scope for the clinical practice derived from the simulation (Table 2).
Student performance and the aspects addressed by the students with respect to the simulated patients for counselling (N=83).
| Variable | Proportion | Standard error | Confidence intervals 95% | |
|---|---|---|---|---|
| Sociodemographic characteristics addressed by the students (86.83% addressed) | ||||
| Sociodemographic status | 87.01 | 3.86 | 79.33 | 94.69 |
| Ethnicity | 89.61 | 3.5 | 82.64 | 96.58 |
| Marital Status | 84.42 | 4.16 | 76.13 | 92.7 |
| Religion | 79.22 | 4.65 | 69.95 | 88.49 |
| Age | 90.91 | 3.3 | 84.34 | 97.48 |
| Language | 90.91 | 3.3 | 84.34 | 97.48 |
| Occupation | 85.71 | 4.01 | 77.72 | 93.71 |
| Obstetric gynaecological background considered by the students (72.26% addressed) | ||||
| Gestations | 94.2 | 2.83 | 88.55 | 99.86 |
| Births | 76.81 | 5.12 | 66.6 | 87.02 |
| Abortions | 76.81 | 5.12 | 66.6 | 87.02 |
| Lactation | 52.17 | 6.06 | 40.09 | 64.26 |
| Birth complications | 72.46 | 5.42 | 61.65 | 83.27 |
| Sexually transmitted infections | 49.28 | 6.06 | 37.18 | 61.37 |
| Satisfied parity | 84.06 | 4.44 | 75.2 | 92.92 |
| Pathological background as interviewed by students (61.87% addressed) | ||||
| Co-morbidities | 81.33 | 4.53 | 72.31 | 90.36 |
| Drugs | 60.00 | 5.69 | 48.65 | 71.35 |
| Surgeries | 61.33 | 5.66 | 50.05 | 72.61 |
| Traumatic/Malformations | 48.00 | 5.81 | 36.43 | 59.57 |
| Disabilities | 58.67 | 5.72 | 47.26 | 70.07 |
| Aspects of lifestyle addressed by the students (65.31% addressed) | ||||
| Smoking | 67.50 | 5.27 | 57.01 | 77.99 |
| Alcohol consumption | 67.50 | 5.27 | 57.01 | 77.99 |
| Exercise/Sports | 65.00 | 5.37 | 54.32 | 75.68 |
| Nutritional status | 61.25 | 5.48 | 50.34 | 72.16 |
| Student performance as doctor (79.93% addressed) | ||||
| Identification | 93.67 | 2.76 | 88.18 | 99.16 |
| Establish Relevant Dialogue | 79.75 | 4.55 | 70.69 | 88.81 |
| Identify Needs | 79.75 | 4.55 | 70.69 | 88.81 |
| Communicate Risks/Benefits | 77.22 | 4.75 | 67.76 | 86.67 |
| Clarifies Patients’ Doubts | 75.95 | 4.84 | 66.32 | 85.58 |
| Respectful discourse | 72.15 | 5.08 | 62.05 | 82.26 |
| Adequate for reproductive timing | 81.01 | 4.44 | 72.17 | 89.85 |
| Opinion with respect to the simulation activity (mean value, range 1–5) | ||||
| Satisfaction with the activity | 4.43 | 0.08 | 4.27 | 4.60 |
| Perceived usefulness | 4.96 | 0.03 | 4.91 | 5.02 |
| Perceived self- performance | 3.69 | 0.10 | 3.49 | 3.89 |
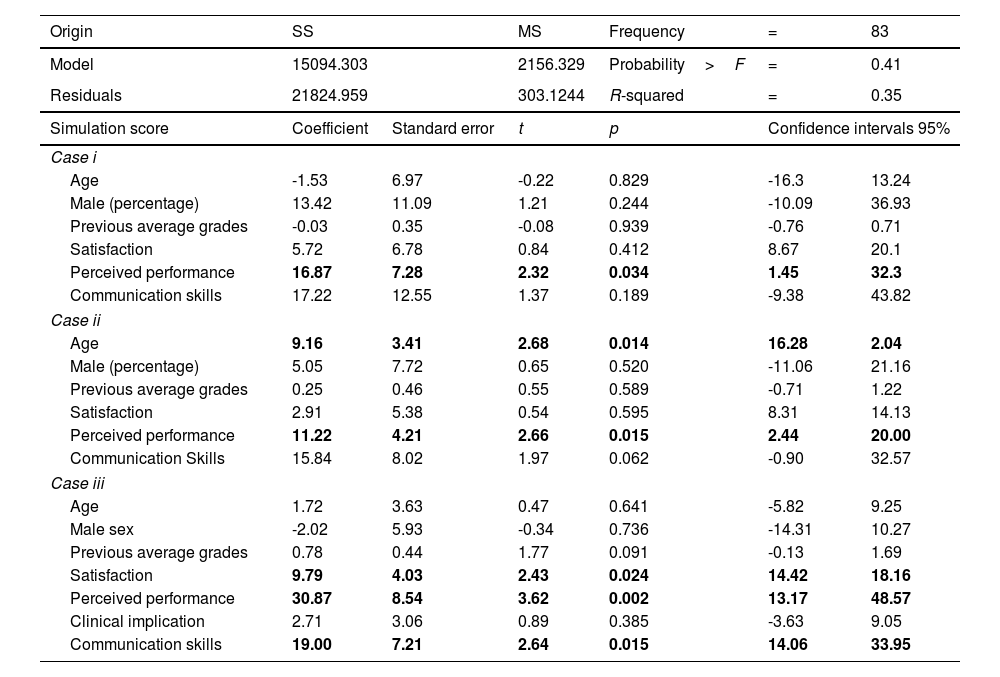
Linear regression model between the grades obtained in the simulation activity and the students’ perceived performance in each case, each student completed two randomly assigned cases.
| Origin | SS | MS | Frequency | = | 83 | |
|---|---|---|---|---|---|---|
| Model | 15094.303 | 2156.329 | Probability>F | = | 0.41 | |
| Residuals | 21824.959 | 303.1244 | R-squared | = | 0.35 | |
| Simulation score | Coefficient | Standard error | t | p | Confidence intervals 95% | |
| Case i | ||||||
| Age | -1.53 | 6.97 | -0.22 | 0.829 | -16.3 | 13.24 |
| Male (percentage) | 13.42 | 11.09 | 1.21 | 0.244 | -10.09 | 36.93 |
| Previous average grades | -0.03 | 0.35 | -0.08 | 0.939 | -0.76 | 0.71 |
| Satisfaction | 5.72 | 6.78 | 0.84 | 0.412 | 8.67 | 20.1 |
| Perceived performance | 16.87 | 7.28 | 2.32 | 0.034 | 1.45 | 32.3 |
| Communication skills | 17.22 | 12.55 | 1.37 | 0.189 | -9.38 | 43.82 |
| Case ii | ||||||
| Age | 9.16 | 3.41 | 2.68 | 0.014 | 16.28 | 2.04 |
| Male (percentage) | 5.05 | 7.72 | 0.65 | 0.520 | -11.06 | 21.16 |
| Previous average grades | 0.25 | 0.46 | 0.55 | 0.589 | -0.71 | 1.22 |
| Satisfaction | 2.91 | 5.38 | 0.54 | 0.595 | 8.31 | 14.13 |
| Perceived performance | 11.22 | 4.21 | 2.66 | 0.015 | 2.44 | 20.00 |
| Communication Skills | 15.84 | 8.02 | 1.97 | 0.062 | -0.90 | 32.57 |
| Case iii | ||||||
| Age | 1.72 | 3.63 | 0.47 | 0.641 | -5.82 | 9.25 |
| Male sex | -2.02 | 5.93 | -0.34 | 0.736 | -14.31 | 10.27 |
| Previous average grades | 0.78 | 0.44 | 1.77 | 0.091 | -0.13 | 1.69 |
| Satisfaction | 9.79 | 4.03 | 2.43 | 0.024 | 14.42 | 18.16 |
| Perceived performance | 30.87 | 8.54 | 3.62 | 0.002 | 13.17 | 48.57 |
| Clinical implication | 2.71 | 3.06 | 0.89 | 0.385 | -3.63 | 9.05 |
| Communication skills | 19.00 | 7.21 | 2.64 | 0.015 | 14.06 | 33.95 |
Theoretical and cognitive learning evaluated with written pre and post tests were compared, observing that the students increased their knowledge by 7.23 points through simulated activity. A significant increase between the first and last simulation activity of the semester was observed, which can be observed in Table 3.
Student performance by group and evaluation type.
| Evaluation | Mean | Standard error | Confidence intervals 95% | |
|---|---|---|---|---|
| Theoretical evaluation | ||||
| Pre-simulation | 68.18 | 1.37 | 65.45 | 70.91 |
| Post-simulation | 75.41 | 1.33 | 72.77 | 78.06 |
| Difference | 7.24 | 1.55 | 10.32 | 4.15 |
| t= | 4.66 | p (T<t)= | 0.000 | |
| Stimulation performance at the beginning and end of the semester | ||||
| First simulation | 75.41 | 2.49 | 22.3 | 70.36 |
| Last simulation | 89.67 | 1.06 | 87.57 | 94.5 |
| Difference | 14.26 | 1.44 | 12.85 | 17.2 |
| t= | 4.38 | p (T<t)= | 0.000 | |
Thru linear regression analysis, direct and significant association was found between the students’ test points, satisfaction and self-perceived performance. Since a mixed methodology has been applied, the following results are presented in two groups according to their methodology and analysis plan.
Qualitative resultsFew students perceived their knowledge as insufficient, as most of them indicated their knowledge was a substantial strength:
“I had a complete knowledge of all the available methods and…it helped me to present the contraceptive options, their benefits and risks in a colloquial way to the patient, taking into account what they wanted and needed”.
Other perceived strengths such as the ability to establish effective communication “I was able to do a complete anamnesis (almost) and deliver the most adequate contraceptive method for the specific patient” and a positive attitude to establish a sympathetic communication, “…it helped me…but I believe that I still canimprove”.
Students liked the singularity and spontaneity of simulated cases, while others valued the possibility of practicing with standardised patients “The fact of being able to participate in this activity and be able to make a mistake here and notoutside”. All the students appreciated the evaluation method, but most of all, the constructive feedback from instructors.
DiscussionWe presented the results of an exploratory, simulation-based learning activity aimed to improve knowledge and competences for Family-Planning counselling, finding that in complement to theoretical bases and case-based analysis, simulations based activities improve communication skills of students and reinforce the students’ ability to adequately respond to real life, unprecedented simulated situations and comprehending the patients as a whole, not merely in response to their reproductive features.
Previous studies reported that communication issues were perceived by patients as a common barrier to contraceptive use.12 Openness to dialogue facilitates patients’ adherence, understanding and commitment to a given contraceptive method.13 In the present study, medical students identified the importance of communicating, generating confidence in the users of the simulated health services.
Holt and colleagues stressed the importance of considering patients’ clinical history when providing Family-Planning counselling, and emphasised the importance good communication in individualised, sensitive counselling.14 In the present study, students acknowledged the importance of these two aspects.
While we observed that a lack of self-perceived communication skills affected the simulated counselling, lack of knowledge also had a negative impact on simulated performance. Previous training in reproductive, obstetric and gynaecological have been oriented to procedural and organisational aspects,15 but our study also provides evidence on the importance of also developing skills to adequately communicating with patients in health-related decision making.
ConclusionsSimulation-based Family-Planning educations is a promising strategy for the medical students to develop competences, reinforce knowledge and gain confidence to correctly inform and effectively counsel their patients.
Previous presentationNone.
FundingNone declared.
Authors’ contribution- •
MID and AAB: coordination of data collection activities/drafting of the original proposal/work design, gathering/obtaining results, drafting of the final manuscript.
- •
YACC: work design, qualitative collection/obtaining results and writing.
- •
JSML: work design, gathering/obtaining results, writing the final manuscript.
- •
CSG and EAV: work design, gathering/obtaining results, writing the final manuscript.
- •
NMD: original idea, methodological planning/work design, gathering/obtaining results, writing the final manuscript.
The authors of this article declare no conflict of interest.
To the students who participated in the project and to the biomedical engineer Joeana Cambranis Romero for the technical and logistical support.