This review aims at identifying research trends in medical education focused on clinical reasoning and argumentation for the resolution of specific problems in the area of medicine. A systematic literature review was performed comprising articles from 2015 to 2019 with the keywords; Clinical Reasoning and Medical Education. A total of 191 articles were initially found, of which 52 were analyzed as they were in accordance with the criteria designed for the study. Most studies had a qualitative design and, although they were focused on the teaching process, there was a fundamental recognition of the student in the design of strategies and methods. The theoretical and thematic categories most addressed were new trends in teaching strategies, resolution of medical practice problems, and the decrease in diagnostic error. This type of study allows the delimitation of fields of research, and clarifies the state of progress, approaches, and interests of researchers dedicated to this particular area. It is concluded that the investigation of teaching practices that lead to the promotion of argumentation in students has become a field of exploration, and introduces new perspectives in relation to the training process. This supports the need to integrate the method into teaching and learning processes of health sciences, as well as in the theoretical and methodological developments resulting from research on specific didactics.
En vista del creciente interés por la aplicación de las teorías educativas, y más específicamente de las didácticas de dominio específico a los procesos de enseñanza y aprendizaje de la medicina, se hace necesario delimitar los campos de intervención que den pie a nuevas propuestas metodológicas, donde se privilegie la promoción del pensamiento crítico y el razonamiento científico, enfocados en la resolución de problemas en salud. Esta revisión pretende identificar las tendencias de investigación en educación médica con respecto al razonamiento clínico y a la argumentación para la resolución de problemas específicos del área de la medicina. Se llevó a cabo una revisión sistemática de la literatura, incluyendo artículos desde el 2015 hasta el 2020, con las palabras clinical reasoning y medical education. Inicialmente, se encontraron 191 trabajos, de los cuales se terminaron analizando 52, según los criterios diseñados para la investigación. La mayoría de los estudios tienen un diseño cualitativo y están centrados en el proceso de enseñanza, aunque enfocados en los estudiantes. Las categorías teóricas y temáticas más abordadas son las nuevas tendencias en estrategias de enseñanza, la resolución de problemas de la práctica médica y la disminución del error diagnóstico.
Este tipo de estudios permite delimitar los campos de investigación y dejar claro el estado de avance, los enfoques y los intereses de los especialistas dedicados a estas áreas particulares. La investigación de las prácticas docentes que conllevan a la promoción de la argumentación en los estudiantes se ha convertido en un campo de exploración y de planteamiento de nuevas perspectivas en relación con el proceso de enseñanza y aprendizaje, lo cual apoya la necesidad de incorporar a este último concerniente a las ciencias de la salud, los desarrollos teóricos y metodológicos productos de la investigación de las didácticas específicas.
Medical activity is based on the care of a patient with whom a relationship of symptoms and signs exploration is established, that could also be called data, to which health professionals apply knowledge and thinking skills to reach a tentative conclusion called a diagnosis; this, in turn, is the origin of a deeper analysis that determines the management, application of protocols, request for diagnostic aids or referral to centers of greater complexity.1 However, such mental exercises of exploration, analysis, and use of data for the resolution of a clinical problem through argued decisions are not always successful2; adverse consequences have even been described by patients due to erroneous prescription of medication, inadequate choice of diagnostic methods, or erroneous advice on therapeutic indications.3–5
In addition to the aforementioned, it is important to note that, for medical associations, the acquisition of knowledge and development of cognitive skills are the fundamental basis that underpin the creation of human talent training programs in health that are focused on the prevention, diagnosis, treatment, and recovery of an individual or a community.6
However, despite the great relevance that is given to the development of higher order cognitive skills such as argumentation as part of their training, studies focused on the evaluation of the argumentative processes of health professionals involved in applying their reasoning abilities to solve challenges encountered in their professional life are incipient—especially when taking into account that they not only do it in specific situations, such as in moments of crisis in emergencies, but also in daily practice when facing situations of an ethical or legal nature, or where factors such as emotions and particular beliefs are involved.7
In addition, the importance of argumentation in the construction of scientific knowledge is recognized, to the extent that students are encouraged to use clinical concepts and procedures that allow them to understand the dynamics of health sciences.8–10
This exploratory review seeks to identify research trends in medical education focused on clinical reasoning and argumentation for the resolution of problems specific to the area of medicine, and therefore achieve the construction of valid and updated records, identifying the integration of teaching practice in medicine and new trends in specific didactics.11
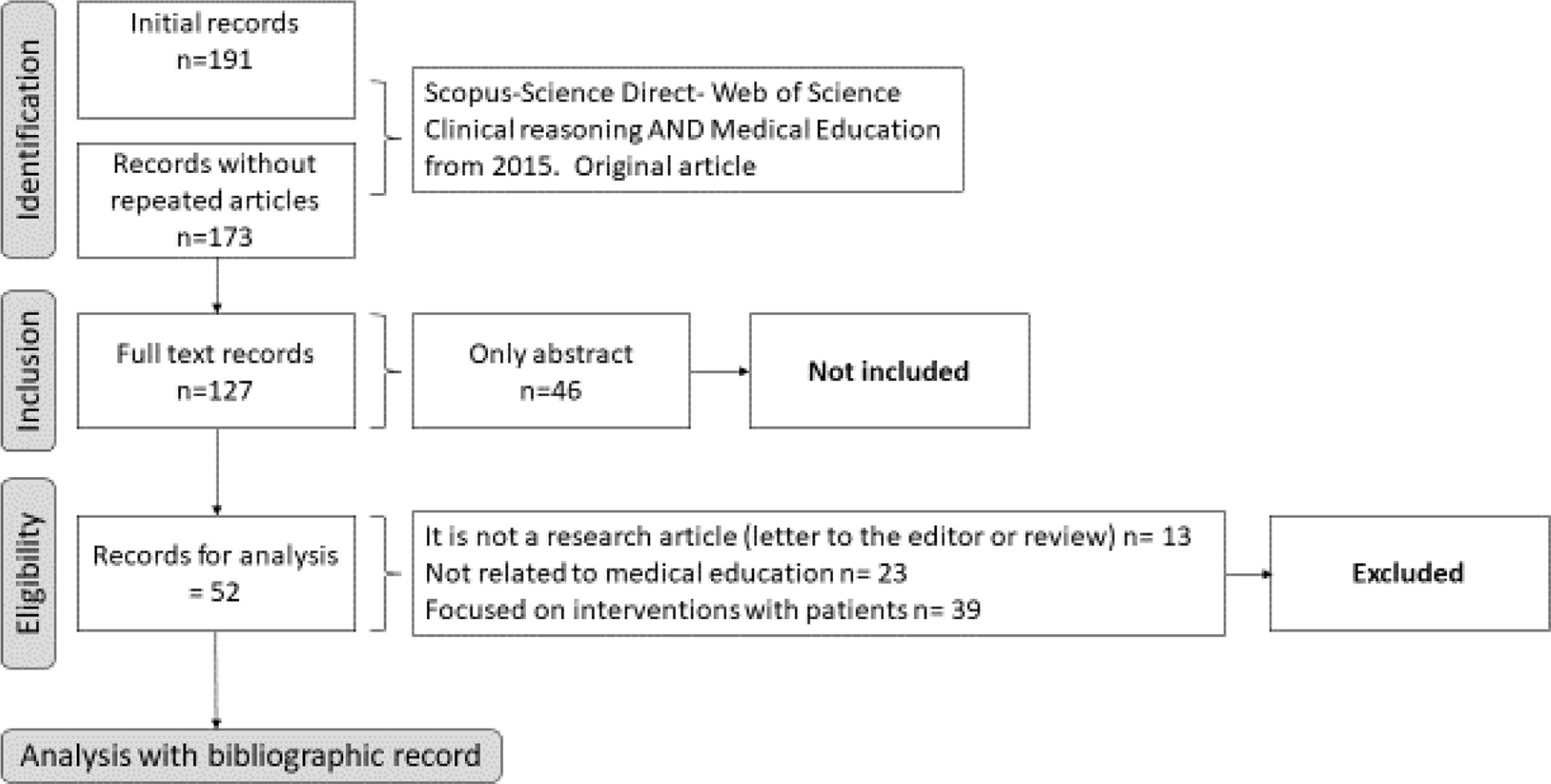
MethodologyIn order to initiate the review, a guiding question was required to define a clear and timely objective of the search. Careful consideration was given to terms that are common to many areas of study and research such as argumentation, reasoning, and medical education, and moreover, that they can even refer to different concepts according to the approach. Therefore, the following question was raised: What are the theoretical and methodological research trends on the development of argumentation and clinical reasoning in the context of medical education?
To select appropriate search terms, a pilot search was performed in MEDLINE defining the words MESH and the initial equation that best described the purpose of the review. Clinical reasoning AND Medical education were chosen; the word Argumentation was excluded in view of its polysemy, and also because it is often associated with formal logic rather than training or development of cognitive reasoning skills in the educational context.
Subsequently, the articles inclusion criteria were defined: Primary research articles focused on clinical reasoning processes in medical education, dated between 2015 and 2019 inclusive, using the Scopus, Web of Science and Science Direct databases, which were available as full text and not just as summaries. An additional filter was carried out to remove, from one of the lists, articles that were repeated in two or more databases.
The exclusion criteria comprised: Non-primary research articles such as reviews, letters to the editor, case reports or comments, documents related to another area of health or not related to medical education, articles related to the direct practice of medicine or focused on the performance of a health professional in particular cases with patients (for instance, reasoning tests used by psychiatrists or neurologists with their patients), or decision making about career choice.
Then, a bibliographic record was created defining specific categories with which to conduct an analysis of current trends comprised in domain specific didactics such as: Type of study (Quantitative, Qualitative, or Mixed), countries of origin, individuals analyzed (teachers or students), research focus (teaching or learning), theoretical perspective, categories of analysis, results, and relevant conclusions (Fig. 1).
ResultsInitially, 191 articles were found, of which 52 were included for the analysis. Most articles stemmed from North America (USA and Canada), followed by Europe, Australia, and Latin America, although the works had the participation of researchers from multiple backgrounds.
The journals from where the articles came were classified into categories according to the area of knowledge they discussed, and included scientific disciplines of education, education in health sciences, and medicine research, among others.
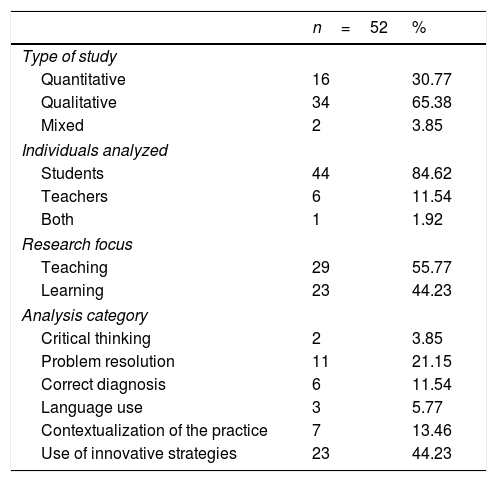
The studies were based on comprehensive analysis of practices, with most (65.38%) being of the qualitative type that investigated the educational process as a social phenomenon—one that is increasingly influenced by the context and factors such as student and teacher motivation, and information management mediated by self-regulation.
Although research on clinical reasoning should be centered on students, it is the teaching aspect that is mostly analyzed (55.77%), rather than classroom learning (Table 1).
Characteristics of the research articles related to clinical reasoning and medical education 2015–2020.
| n=52 | % | |
|---|---|---|
| Type of study | ||
| Quantitative | 16 | 30.77 |
| Qualitative | 34 | 65.38 |
| Mixed | 2 | 3.85 |
| Individuals analyzed | ||
| Students | 44 | 84.62 |
| Teachers | 6 | 11.54 |
| Both | 1 | 1.92 |
| Research focus | ||
| Teaching | 29 | 55.77 |
| Learning | 23 | 44.23 |
| Analysis category | ||
| Critical thinking | 2 | 3.85 |
| Problem resolution | 11 | 21.15 |
| Correct diagnosis | 6 | 11.54 |
| Language use | 3 | 5.77 |
| Contextualization of the practice | 7 | 13.46 |
| Use of innovative strategies | 23 | 44.23 |
In the case of health sciences, efforts have been directed to the development of domain specific thinking skills, mostly focused on the promotion of clinical argumentation for the resolution of specific problems12,13 and the development of critical thinking for application in professional life.14,15 In this manner, argumentation is considered a fundamental cognitive “competence” in health professionals, and more specifically, in health professional training.16,17 However, most research has focused on the study of strategies for medical practice problem resolution and on the intervention of patients in the social context.18,19 Therefore, the literature largely addresses topics such as clinical simulation, telemedicine, the use of technology in the curriculum, problem-based learning, and gamification,20,21 which are seen as strategies for the promotion of professional performance, usually aimed at solving challenges related to diagnosis and correct management.
ConclusionsThe systematic review of scientific information remains a method of information analysis that allows the reconstruction of the current state of a specific topic; in this case, a series of documents are analyzed to identify current trends regarding clinical reasoning, viewed from the approach of argumentation in medicine and considered from a functional perspective. That is, considering it as a thinking skill that encourages the creation of scientific concepts, and should be included in the planning of the higher education curriculum.22
Studies have also shown that research in the field of specific didactic of health sciences has been neglected, where in addition to the promotion of problem-solving and decision-making, aspects such as metacognition and self-regulation, emotions and motivations of the actors in the process, as well as the use of language through scientific argumentation, should be taken into consideration.11,23–25
A literature review of this type makes it possible to delimit the fields of research and clarify the state of progress, approaches, and interests of researchers dedicated to these particular areas. It is possible to glimpse a tendency to try to improve the work of the health professional, which is directly related to their performance and social role, that is, they are more focused on professional competence, rather than achieving integral cognitive skills that promote critical thinking and metacognition of the student.
Implications for future researchResearch on teaching practices that lead to the promotion of argumentation in students has become a field of exploration and introduces new perspectives in relation to teaching and learning processes,22,26 where the understanding of student/teacher dynamics, aimed at the creation of a learning community based on the training of professionals in particular areas, is fundamental for the consolidation of a didactics of health sciences.27,28
This supports the need to incorporate theoretical and methodological developments, which are products of specific didactics research, into health sciences training processes.29,30,31,32 This also implies systematic and rigorous reflection on the scope, intentionality, and awareness that teachers manifest when designing strategies that promote argumentation in health education contexts.33
Conflict of interestThe authors of this article declare no conflict of interest.