Students experience difficulties defining a sequential order and analyzing variables when solving a clinical problem on real-time. Learning in a virtual environment using PBL and e-learning promotes hypothesis-generating research and case study through clinical reasoning.
MethodsTwenty-two physical therapy students enrolled in a Clinical Reasoning course were asked to solve virtual clinical cases that included three different fields: orthopedic, cardiovascular/pulmonary and neurological. To evaluate the intervention, students’ perception as well as their lecture/lab academic performance, were considered.
ResultsAn increase in academic performance in both lecture and lab average grades in comparison to previous years (ANOVA test, *p<0.05). Fifty-eight percent of students reported prior study, critical thinking and technical language were aspects improved by this resource. Half of the enquired subjects also reported not having enough time to solve cases and suggested be given more adequate feedback.
ConclusionsAfter this experience, teacher's role as a facilitator in the teaching learning process, putting the student in a leading role by using metacognitive strategies in tune with technology. Case-solving presents an advantage by improving the process of hypothesis-generation based on the information gathered from a case study problem. Early introduction of teaching strategies promote a systematic practice such as critical thinking through case study, and debate about the feedback needed for its achievement.
Los estudiantes experimentan dificultades para definir un orden secuencial y el análisis de variables de razonamiento clínico en presencia de un problema en tiempo real. El entorno virtual de aprendizaje mediante el ABP y el e-learning favorece la investigación, la generación de hipótesis y la aplicación-resolución de casos mediante razonamiento clínico.
MétodoSe implementó la resolución de casos clínicos virtual en tres áreas disciplinares: rehabilitación traumatológica, cardiorrespiratorio y neurorrehabilitación para 22 estudiantes de kinesiología en la asignatura de razonamiento clínico. Se evaluó el recurso incorporado mediante una encuesta de percepción y el rendimiento teórico-práctico.
ResultadosEl análisis reveló un incremento en el rendimiento académico en evaluaciones de cátedra y prácticas en comparación a los años previos (test ANOVA, p<0,05). El 58% de los estudiantes reconocen que el estudio previo, el análisis y el lenguaje técnico son variables desarrolladas mediante la herramienta. El 50% reconocieron falta de tiempo para resolver los casos, sugieren mayor retroalimentación y evitar volver al inicio en presencia de errores.
ConclusiónResultó relevante modificar el rol del docente en pregrado con la intención de facilitar y conducir el proceso de aprendizaje del estudiante, lo que favorece la formulación y la articulación de hipótesis según la información obtenida a partir del caso problema. Se propone la incorporación temprana de estrategias didácticas que promuevan la reflexión mediante problemas clínicos.
In Health Sciences, the most important challenges students confront when studying clinical courses resides on their ability to achieve a proper analysis while simultaneously doing pattern recognition, when facing a clinical scenario.1 Moreover, students experience confusion and difficulty when having to define a sequential order to reason while considering clinical variables available in a brief amount of time.2 Conventional teaching strategies tend to be mainly expository and unidirectional, where the teacher provides only the key elements about a case study, which delays and lessens the students’ ability to develop critical thinking skills related to experience.3 Currently, new policies in clinical teaching safeguard key elements, such as review and mental structuring of contents to fabricate a diagnostic impression of common health problems.4,5 Based on these new elements, students then propose a treatment and prognosis that are coherent with the diagnosis. Wingelaar6 states the importance of developing early clinical reasoning skills in medical education, and the incorporation of the students’ perception about different methologies used during the teaching-learning process. Among other factors, the author emphasizes textbook limitations when delivering clinical contents in a comprehensive way, students’ difficulty in organizing information, and poor adherence to studying habits that include solving clinical cases on daily basis.6–8 Therefore, a digital learning environment, and the use of scripts validated by experts and designed for clinical training, show certain advantages: (1) improves the students’ expertise to formulate differential diagnoses, proposing clinical treatments or investigative tactics, and (2) set a physical and symbolic assessment between the student and his object of knowledge, with other players within the educational context such as peers and teachers, which are key elements for the application of the hypothetical-deductive reasoning model.9,10
MethodologyExperimental cross-section study. Sample consisted of twenty-two physical therapy students (n=22) who enrolled for the course “Clinical Reasoning” during the first semester of 2019 at Santo Tomas University in the city of Viña del Mar, Chile.
A case-solving digital resource was designed and implemented, considering three different fields of physical rehabilitation (orthopedic, cardiovascular/pulmonary and neurological) and was then loaded into the course's virtual classroom. Each clinical case scenario included topics, such as, anamnesis, physical assessment, imaging interpretation, diagnosis and treatment objectives, which had to be solved within a maximum of 20min. The resource was evaluated using a perception survey and by comparing the students’ average performances with those of previous years between 2015 and 2018 (control groups, n=151), when students were only given case-solving exercises in the last pre-assessment class. The perception survey included 15 questions grouped into 3 domains: meaningful learning, declarative-procedural learning, and teaching strategy.
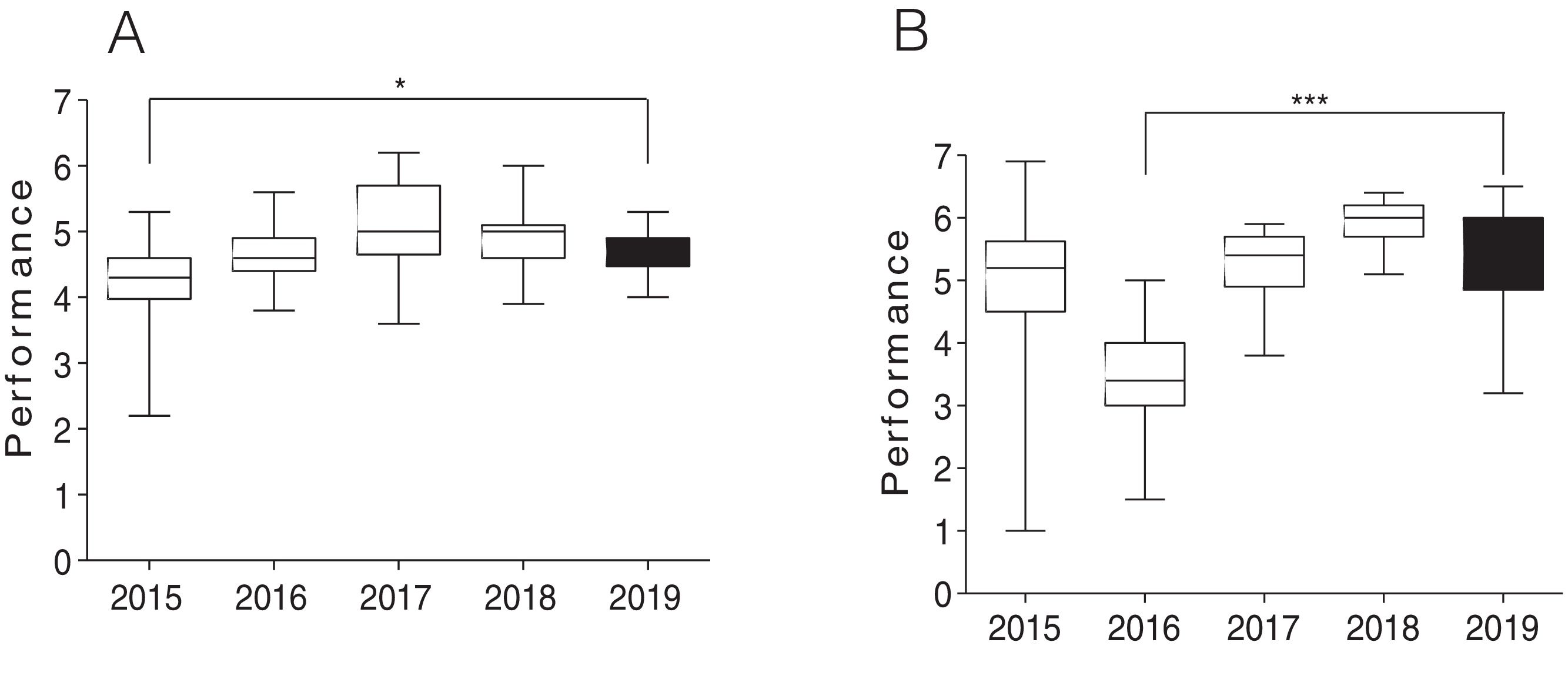
Open questions were added at the end the perception survey to collect free feedback from students. Quality criteria were established for each domain and considered the following categories: Strongly Agree, Agree, Neutral, Disagree and Strongly Disagree (Appendix 1). Performance was assessed using the students’ average grades on a scale of 1 to 7, considering as minimal passing grade a score greater than or equal to 4.0 (or 4.0), and reprobation a score equal to or less than 3.9 (≤3.9) (Fig. 1).
Experimental methodology design. Students who enrolled in a Clinical Reasoning course during the years 2015–2018 were part of the control group and were subjects of three evaluations; while students who participated in 2019 received this e-learning methodology prior each course/unit evaluation.
The authors declare that they have followed the protocols of their institution regarding the publication and protection of student data.
ResultsThe use of an e-learning methodology during 2019 increased the students’ average performance in lecture (Fig. 2A) with a mean score of 4.68±0.05 when compared with the mean score of 4.29±0.08 obtained in 2015. When comparing the results with the years 2016 (4.63±0.05), 2017 (5.19±0.12) and 2018 (4.94±0.09) there is no significant improvement.
Students’ performance in clinical reasoning course: (A) Performance in the course's lecture evaluations between the years 2015 and 2019, highlighting 2019's intervention using the new case-solving digital resource. Academic performance in 2019 is significantly higher than in 2015 (ANOVA/Bonferroni post hoc test, *p<0.05). (B) Performance in the course's lab evaluations. The academic performance recorded during 2019 intervention is significantly higher than in 2016 (ANOVA/Bonferroni post hoc test, *p<0.05). The data is presented as mean scores±SEM.
Performance in laboratory (Fig. 2B) showed a significant increase with a mean of (5.31±0.19) during 2019 in comparison with average scores obtain in 2016 (3.49±0.10). This intervention showed no significant difference when compared with the years 2015 (5.0±0.14) and 2017 (5.1±0.12), although 2018's mean score (5.94±0.06) was higher (Fig. 2).
The data collected from the perception survey that dealt with the domain “meaningful learning” revealed that 53% of students recognized that case solving requires the integration of clinical information; and that the incorporated resource allowed them to learn by trial and error. In addition, 58% of participants found that case study in a virtual environment it's a better approach to address a content or topic. Declarative-procedural learning, at least 53% of students considered that the contents and topics included in these clinical cases were reviewed in previous courses. Over 50% of participants agreed or strongly agreed that the digital resource encouraged the use of technical language. Meanwhile, the same percentage reported difficulties sorting, managing and remembering the contents and information delivered on a clinical case. Regarding the intervention as a teaching strategy, about 50% of students reported that practice through virtual training has increased motivation allowing for a better performance in clinical reasoning. 90% of participants showed in favor of including this methodology in other courses (Fig. 3).
Student's perception survey about quality criteria for each topic. graphic shows the students’ opinion presented as quality criteria for domains each question related to the meaningful learning, declarative-procedural learning and teaching strategy. (A) Meaningful Learning. 1. Case solving requires content integration. 2. Prior study is required to recognize relevant clinical patterns present in these cases. 3. Solving virtual clinical cases allow for content analysis. 4. The resource promotes curiosity to study and solve these cases. 5. The resource allows for learning by trial and error. (B) Declarative-Procedural Learning. 1. The contents and topics included in the clinical cases have been reviewed on previous courses. 2. The cases are extremely difficult to solve for a fourth-year physical therapy student. 3. Do you think you have the skills and training to properly solve the case? 4. Student had difficulties in sorting, managing and remembering the contents and information that a clinical case delivers. 5. The resource promotes the use of technical language. (C) Learning Strategy. 1. Practice through this virtual training allows for a better performance in clinical reasoning. The teacher encouraged the use of this resource and solved questions. 3. The virtual clinical case allows you to simulate your performance in a controlled scenario. 4. Solving these cases increased your motivation to learn how to deal with clinical problems in different disciplinary areas of physical rehabilitation. 5. Would you like to include this methodology in other courses and disciplinary areas to improve learning?
Open-questions response revealed that 50% of students claimed not having enough time to solve the presented cases. 40% of participants gave suggestions to improve the resource which included: giving better feedback and eliminating the step of going back to the start when failing an answer (not shown).
DiscussionThe results of this investigation validate the teacher's current role as a facilitator of knowledge, guiding the student's learning process. In this modern paradigm, the student has the leading role in the generation of metacognitive strategies to self-manage his understanding of contents, his analysis and critical thinking skills.11,12
This strategy encourages teachers to approach the complexity of clinical reasoning by working pattern recognition with their students, in order to promote contrast of information and discussion. The method of collaborative knowledge building to solve a given clinical problem is favored by the use of technology, which emulates the act of solving clinical problems in its whole multidimensionality as a complement to clinic practice.13
The main teaching-student consensus was that clinical reasoning needs the correct interpretation of technical language, prior study and critical thinking skills, elements that are time dependent, which in turn encourages students to increase their autonomy and improve their management of time devoted in deepening the topics.14 E-learning with case study methologies, improves progressive levels of independence, autonomy and motivation during the last stage of student training in health sciences.15 Similar studies have shown advantages in promoting skills related to the generation of hypotheses according to the information obtained from a case problem, as well as the students’ personal research to accomplish this process.16
It was considered as limitations of this study the number of students who participated in the sample as well as the non-application of assessment tools that would allow to quantify and determine specific aspects of reasoning that were best achieved by these students, as well as if these aspects correspond to meaningful learning.17,18
In conclusion, this study proposes the early incorporation teaching strategies that encourage systematic training to improve critical thinking skills through clinical problem solving and feedback discuss. In addition, it is recommended the use of this type of intervention no just as teaching-learning tool but also as a useful assessment format.
Presentation of the workCongress of academic innovation Santo Tomas University (Santiago, Chile).
FundingAcademic innovation project funded by internal fund Santo Tomás University.
Conflict of interestThe authors declare no conflicts of interest.