Interstitial lung disease (ILD) is one of the leading causes of mortality in autoimmune diseases. The extent of the disease is a determining factor in the prognosis and treatment initiation and monitoring. Quantification using the Goh method is the most commonly used method; however, it is subjective. So far, no studies have evaluated the level of agreement among various readers.
ObjectiveThe study's objective is to determine the interobserver and intra-observer variability in using ILD quantification among physicians from various specialties and levels of experience.
MethodsImages from chest computed tomography of patients with rheumatoid arthritis (RA) or systemic sclerosis (SSc) and ILD were collected. The five necessary cuts described by Goh were extracted to be evaluated by pulmonologists, rheumatologists, radiologists, fellows, and a thoracic radiologist (gold standard). The interobserver and intra-observer variability values were calculated using the intraclass correlation coefficient test or Cohen's Kappa test, depending on the nature of the variable, between each group of medical specialties and in comparison with the gold standard.
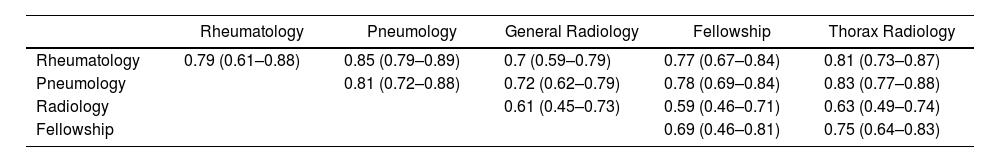
ResultsSeventy-nine patients were selected, primarily women, 56% having SSc. A total of 1098 CT scans were performed. The intraclass correlation coefficient was .75 (95% CI: .67–.81), including all nine readers. The best correlation with the gold standard was found among pulmonologists (CCI .83) and rheumatologists (CCI .81). According to severity (more significant or less than 20% extension), the Kappa coefficient was .64 among the nine readers. The intraclass correlation coefficient for the average intra-observer correlation of all readers was .89 (95% CI: .81–.93), and the Kappa coefficient was .82.
ConclusionThe Goh method is valuable and highly correlated among a diverse group of specialties that manage ILD, making it a practical tool for assessing the extent of the disease.
La enfermedad pulmonar intersticial (EPI) es una de las principales causas de mortalidad en las enfermedades autoinmunes. Su extensión es un factor determinante en el pronóstico, el inicio o el monitoreo del tratamiento. El método de Goh es el más utilizado para su cuantificación; sin embargo, es subjetivo. Hasta el momento no hay estudios que evalúen el grado de acuerdo entre varios lectores.
ObjetivoEl objetivo del estudio es determinar la variabilidad interobservador e intraobservador en el uso de la cuantificación de la EPI en un grupo de médicos de diversas especialidades y tiempo de experiencia.
MétodosSe recopilaron imágenes de tomografía computarizada de tórax de pacientes con artritis reumatoide (AR) o esclerosis sistémica (ES) y EPI. Se extrajeron los cinco cortes necesarios descritos por Goh para ser evaluados por neumólogos, reumatólogos, radiólogos, residentes y un radiólogo de tórax (estándar de oro). Los valores de variabilidad interobservador e intraobservador se calcularon utilizando la prueba estadística del coeficiente de correlación intraclase o la prueba Kappa de Cohen, según la naturaleza de la variable, entre cada grupo de especialidades médicas y en comparación con el estándar de oro.
ResultadosSe seleccionaron 79 pacientes, en su mayoría mujeres, un 56% con ES. Se realizaron un total de 1.098 lecturas de TC. El coeficiente de correlación intraclase fue de 0,75 (IC95%: 0,6-0,81), incluyendo a los 9 lectores. La mejor correlación con el estándar de oro fue de los neumólogos (CCI: 0,83) y reumatólogos (CCI: 0,81). Según la gravedad (mayor o menor al 20% de extensión), el coeficiente Kappa fue de 0,64 entre los 9 lectores. El coeficiente de correlación intraclase para la correlación intraobservador promedio de todos los lectores fue de 0,89 (IC95%: 0,81-0,93), y el coeficiente Kappa fue de 0,82.
ConclusiónEl método de Goh es útil y tiene una alta correlación entre un grupo diverso de especialidades que manejan la EPI, lo que lo convierte en una herramienta práctica para calcular la extensión de la enfermedad.