Community pharmacy settings are considered the front line to provide effective patient care and safe use of medicines. A pharmacy internship program imposes considerable responsibility on pharmacy students to prioritize their education and training to become patient-centered healthcare providers and to support their further professional development. The aim of this study was to explore the perceptions and the experience of undergraduate pharmacy students who had their training practices in community pharmacies and to identify the related barriers during the internship training program in Türkiye.
Materials and methodsA cross-sectional study was conducted among pharmacy students who had received their training in community pharmacy settings in Istanbul, Türkiye. The study was conducted using validated online questionnaires consisting of five sections during the period from March to October 2024.
ResultsA total of 231 pharmacy students responded to the questionnaires with a mean age of 22 ± 2.66 years. The majority of the students reported that the community pharmacy offered a practical setting that facilitates students' communication with patients (82.7%, mean 4 ± 0.86, p < 0.0001), the community pharmacy had the necessary resources for drug information (92.2%, mean 4 ± 0.75, p < 0.0001), their internship experience had increased their involvement in the pharmacy profession (92.2%, mean 4 ± 0.71, p < 0.0001), and 87.4% (mean 4 ± 0.77, p < 0.0001) showed that the pharmacy internship program alleviates the stress of direct patient contact. However, most of the trainees reported that there were difficulties in finding a pharmacy for internship training (53.7%, mean 4 ± 1.4, p < 0.0001).
ConclusionThe current study revealed that the pharmacy students acquired experience and knowledge during their internship and were equipped with the skills they needed to practice their future pharmacy profession effectively and efficiently. The learning outcomes related to these skills should be addressed during pharmacy degree courses and to implement structured preparation programs before the start of the internship or systematic training for preceptors in community pharmacies that could develop their skills required for the internship process.
Las farmacias comunitarias se consideran la primera línea para brindar una atención eficaz al paciente y un uso seguro de los medicamentos. Un programa de prácticas en farmacia impone una responsabilidad considerable a los estudiantes de farmacia, quienes deben priorizar su formación para convertirse en profesionales de la salud centrados en el paciente y apoyar su desarrollo profesional. El objetivo de este estudio fue explorar las percepciones y la experiencia de estudiantes de farmacia de pregrado que realizaron sus prácticas en farmacias comunitarias e identificar las barreras asociadas durante el programa de prácticas en Turquía.
Materiales y métodosSe realizó un estudio transversal con estudiantes de farmacia que recibieron su formación en farmacias comunitarias en Estambul, Turquía. El estudio se realizó mediante cuestionarios en línea validados, compuestos por cinco secciones, durante el período de marzo a octubre de 2024.
ResultadosUn total de 231 estudiantes de farmacia respondieron a los cuestionarios con una edad media de 22 ± 2,66 años. La mayoría de los estudiantes informaron que la farmacia comunitaria ofrecía un entorno práctico que facilitaba la comunicación con los pacientes (82,7%, media 4 ± 0,86, p < 0,0001), que contaba con los recursos necesarios para la información sobre medicamentos (92,2%, media 4 ± 0,75, p < 0,0001), que sus prácticas habían aumentado su implicación en la profesión farmacéutica (92,2%, media 4 ± 0,71, p < 0,0001) y que el 87,4% (media 4 ± 0,77, p < 0,0001) demostró que el programa de prácticas aliviaba el estrés del contacto directo con los pacientes. Sin embargo, la mayoría de los practicantes informaron que hubo dificultades para encontrar una farmacia para realizar la pasantía (53,7%, media 4 ± 1,4, p < 0,0001).
ConclusiónEl presente estudio reveló que los estudiantes de farmacia adquirieron experiencia y conocimientos durante sus prácticas y adquirieron las habilidades necesarias para ejercer su futura profesión farmacéutica de forma eficaz y eficiente. Los resultados de aprendizaje relacionados con estas habilidades deberían abordarse durante los estudios de grado en farmacia e implementar programas de preparación estructurados antes del inicio de las prácticas o una formación sistemática para tutores en farmacias comunitarias que puedan desarrollar las habilidades necesarias para el proceso de prácticas.
Pharmacists today have additional responsibilities and commitments to enhance their practice, highlighting the fact that the pharmacy profession is evolving into a more patient-focused and outcome-oriented role as opposed to the prior dispensing function.1,2 On the one hand, pharmacies are perceived as local health care centers, serving as the public's initial point of contact with the health care system, while pharmacists are regarded as the most easily available health care experts. In this view, the pharmacy sector benefits public health and assures patient safety.3 Pharmacists need to be well-trained and knowledgeable on how to obtain the most up-to-date and trustworthy information in order to be trusted information sources for patients and other healthcare professionals. In the meantime, pharmacy students are regarded as the cornerstone of healthcare professionals' futures.4–6 Pharmacy schools have improved their training programs to meet these learning objectives in order to fulfill this mission. The development of pharmacy interns' positive attitudes toward offering patient counseling in pharmacies appears to be influenced by education. This is a result of the integration of academic pharmacy education and real-world pharmacy work experience gained through internship assignments.7,8
Experiential training is an essential component of pharmacy curricula globally. Training under the guidance of the preceptor allows students to emphasize, shape, and develop the relevant knowledge and abilities while providing direct patient care.9 The goal of internship is to help students make the transition from academic to professional life by exposing them to the pharmacy field in a controlled learning setting.10 Professionally designed, an internship program helps pharmacy students apply what they have acquired in school to real-world pharmacy settings.11 The majority of developed countries design their pharmacy internship programs to introduce students to pharmacy practice during their first three years of study, typically in community pharmacy settings. In their final year of pharmacy study, they gain advanced practical pharmacy experience, typically in both community pharmacy and hospital settings.4–6,12 This structure usually assists students in applying the skills, attitudes, and knowledge they acquired in the classroom and laboratory settings. Additionally, it is believed that students will be able to use variations in pharmacy practice, such as managing drug therapy in direct patient care settings and assuming responsibility for achieving optimal patient outcomes with this type of training.4–6,13,14 Previous studies has emphasized the acquisition of knowledge and the development of abilities through direct involvement in community pharmacy settings.15,16
For the pharmacy curriculum to be of higher quality, evaluation of the internship programs and outcomes attained from this professional training is crucial. The evaluation of internship programs is specifically important for pharmacy students, who must complete their training as a prerequisite for graduation. In order to elevate these experiences, feedback from students regarding the form and utility of the internship program should be considered for any future implementation in order to suit the evolving needs of the pharmacy profession. Student input is especially is crucial to guarantee that the training enhances knowledge and abilities that will subsequently result in better pharmaceutical decision-making. Earlier data showed that feedback is most effective when it comes from a trustworthy source and is based on specific observations and an action plan.17 Students' learning and future counseling behavior may be influenced by their attitudes and beliefs regarding experiential training. For any new program, including experiential training, to be implemented successfully, it is crucial to gather the opinions and attitudes of the students17.
The legal basis of internship practice in pharmacy education in Türkiye was enacted by the Council of Higher Education on May 25, 2018, in accordance with the European Union Directive 2005/36/EC and the Regulation on Minimum Education Conditions for Medicine, Nursing, Midwifery, Dentistry, Veterinary Medicine, Pharmacy and Architecture. In addition, the standards of internship programs were determined by the Deans' Council of the Faculty of Pharmacy and added to the existing Pharmacy Education Program Core Program. Pharmacy students are required to complete a 6-month professional training program in order to equip pharmacy students with the necessary skills, such as dispensing services, compounding extemporaneous preparations, offering medication counseling, implementing medication management and review services. This can be approached in community pharmacies, hospital pharmacies and, with an additional decision taken in 2018, in the pharmaceutical industry. Pharmacy internship practices of 30 universities in Türkiye were examined, and it was reported that 85% of pharmacy faculties implemented internship programs in accordance with standards.18 However, it did not evaluate in depth students’ perception of learning through quantitative and qualitative methods. Currently, no prior study has assessed students' perceptions of their community pharmacy training experience in Türkiye. Therefore, the aim of this study was to explore the perceptions and the experience of undergraduate pharmacy students who had their training practices in community pharmacies and to identify the related barriers during the internship training program in Türkiye.
Materials and methodsStudy design and settingThis was a cross-sectional study conducted from March to October 2024 by undergraduate students of the Faculty of Pharmacy, Istinye University, Istanbul, Türkiye. The study was approved by the Ethics Committee of Istinye University (No. 24-44), in accordance with the World Medical Association Declaration of Helsinki guidance.
Study participants and sample sizeThe study was recruited by undergraduate students who are currently studying for a bachelor's degree in pharmacy at the Faculty of Pharmacy, Istinye University. The sample size was determined using Cochran's sample size calculation, with a 95% confidence level and a 5% margin of error. Based on the calculated results, an appropriate sample of 430 students was selected to assess the questionnaire responses. Pharmacy interns from the third academic year or above who registered and completed the current internship and pharmacy training practices in urban, independent pharmacies were deemed qualified to participate in the study. Students who refused to participate or provided insufficient responses to questionnaire items were excluded.
Study questionnaireA structured questionnaire was designed and developed for the purpose of this study. The structured items of the questionnaire were reviewed and adapted from the previous literature and amended substantially.4,8,12,14–16,18–20 The amended questionnaire was assessed in terms of content validation, restructuring and appropriateness through peer review by two independent academic experts in medical research. In addition, the questionnaire was pilot tested on 12 pharmacy students to comment on the clarity and simplicity of the items and to eliminate any ambiguity in the survey questions and to determine whether the data will provide reliable information The final version of the questionnaire was improved by taking into account and implementing all of the expert and student feedbacks based on the pilot study. The pre-test data were excluded from the study's final statistical analysis.
The questionnaire was uploaded to Google Drive, and the link was distributed and shared online on the pharmacy students' groups using social platforms via WhatsApp. No financial incentives were offered, and reminder emails were sent out two weeks after the initial email. The questionnaire form was set up to allow for a single completion. Meanwhile, the general information was provided outlining the purpose of the questionnaire and stating that it will take around 10 min to complete. Furthermore, all participants signed an electronic informed consent form prior to participating in the study, stating that their identities and any information they provided would be kept confidential and used solely for research purposes.
The questionnaire consists of five structured sections. The first section collected the pharmacy students' demographic data (gender, year of study, completed days of training) and geographic location (city of internship practice). The second section aims to assess the perception of pharmacy students toward training sites of community pharmacies during the internship training program and consists of 9 items. The third section aims to assess the pharmaceutical care training provided by pharmacy preceptors and students during the internship program and consists of 22 items. The fourth section aims to assess the perception of pharmacy students about the outcomes of the internship program and consists of 15 items. The last section aims to assess the perception of the pharmacy students toward the barriers and challenges during the internship training program and consists of 15 items. The questionnaires within sections two to five will be assessed using the 5-point Likert scale (strongly agree, agree, neutral, disagree, and strongly disagree).
Statistical analysisData were analyzed using the Statistical Package for the Social Science (SPSS) version 23.0 and Microsoft Office Excel 2013. Descriptive analyses were conducted to describe the study population, and the results were expressed in numbers, percentages, means, and standard deviations. The score and the results depend on the 5-point Likert scale rating. The chi-square test was used to assess the significant differences among proportions. Responses to the questionnaire based on Likert scale rating were also presented as percentages, medians and standard deviations. P-value was considered significant at <0.05.
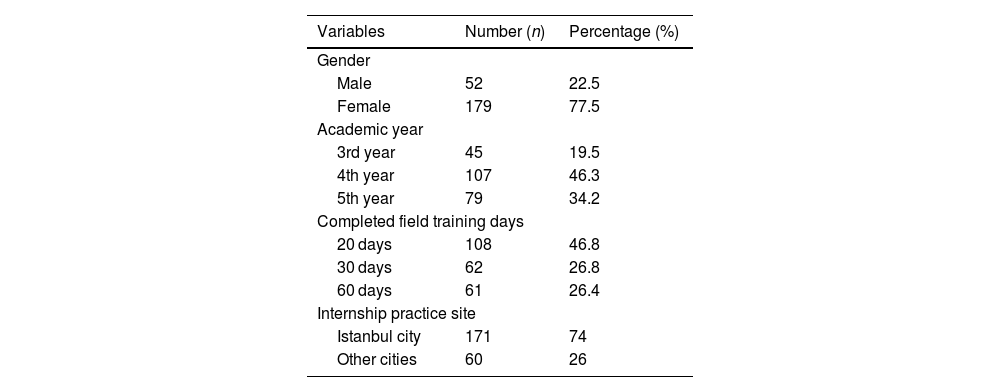
ResultsDemographic characteristics of the participantsA total of 231 pharmacy students responded to the questionnaires with a mean age of 22 ± 2.66 years. The majority of respondents were female (77.5%, n = 179). Most of the interns (46.3%, n = 107) were from the 3rd year students, followed by 5th class students (34.2%, n = 79). Results are summarized in Table 1.
Demographic characteristics of the study participants (N = 231).
| Variables | Number (n) | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 52 | 22.5 |
| Female | 179 | 77.5 |
| Academic year | ||
| 3rd year | 45 | 19.5 |
| 4th year | 107 | 46.3 |
| 5th year | 79 | 34.2 |
| Completed field training days | ||
| 20 days | 108 | 46.8 |
| 30 days | 62 | 26.8 |
| 60 days | 61 | 26.4 |
| Internship practice site | ||
| Istanbul city | 171 | 74 |
| Other cities | 60 | 26 |
Data presented as number (n) and percentage (%).
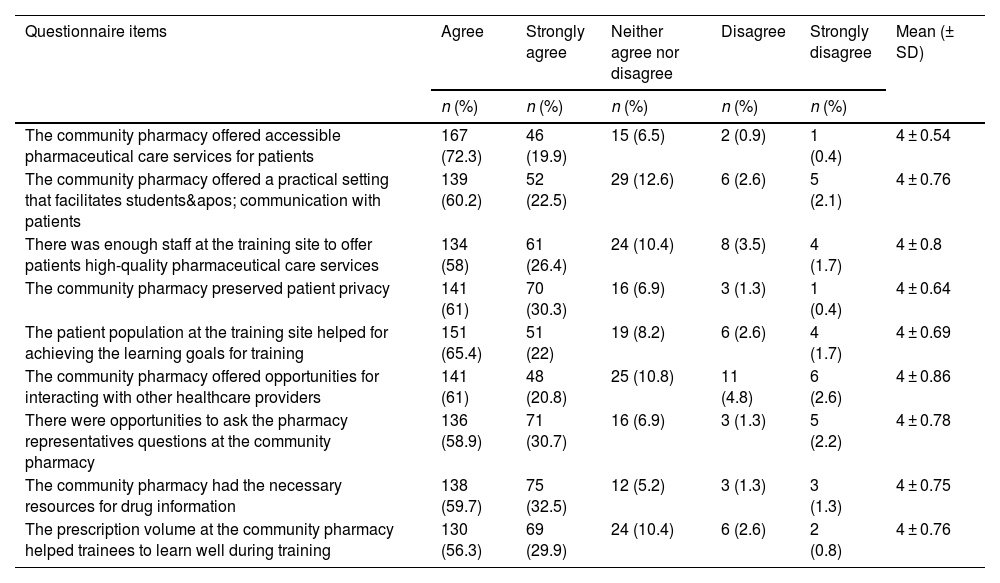
Around three-quarters (74%) of the responding students carried out their internship in Istanbul city. The majority of the interns showed significant positive perceptions and responses toward training sites of community pharmacies and to the way that their preceptors had to be involved in some pharmacy tasks. Furthermore, most of the interns believed that the community pharmacy offered accessible pharmaceutical care services for patients (92.2%, mean 4 ± 0.54, p < 0.0001), and the community pharmacy preserved patient privacy (91.3%, mean 4 ± 0.64, p < 0.0001). In addition, the respondents agreed that the community pharmacy offered a practical setting that facilitates students' communication with patients (82.7%, mean 4 ± 0.86, p < 0.0001) and the community pharmacy had the necessary resources for drug information (92.2%, mean 4 ± 0.75, p < 0.0001). Other results are also summarized in Table 2.
Perception of students toward training sites of community pharmacies during the internship program.
| Questionnaire items | Agree | Strongly agree | Neither agree nor disagree | Disagree | Strongly disagree | Mean (± SD) |
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | ||
| The community pharmacy offered accessible pharmaceutical care services for patients | 167 (72.3) | 46 (19.9) | 15 (6.5) | 2 (0.9) | 1 (0.4) | 4 ± 0.54 |
| The community pharmacy offered a practical setting that facilitates students' communication with patients | 139 (60.2) | 52 (22.5) | 29 (12.6) | 6 (2.6) | 5 (2.1) | 4 ± 0.76 |
| There was enough staff at the training site to offer patients high-quality pharmaceutical care services | 134 (58) | 61 (26.4) | 24 (10.4) | 8 (3.5) | 4 (1.7) | 4 ± 0.8 |
| The community pharmacy preserved patient privacy | 141 (61) | 70 (30.3) | 16 (6.9) | 3 (1.3) | 1 (0.4) | 4 ± 0.64 |
| The patient population at the training site helped for achieving the learning goals for training | 151 (65.4) | 51 (22) | 19 (8.2) | 6 (2.6) | 4 (1.7) | 4 ± 0.69 |
| The community pharmacy offered opportunities for interacting with other healthcare providers | 141 (61) | 48 (20.8) | 25 (10.8) | 11 (4.8) | 6 (2.6) | 4 ± 0.86 |
| There were opportunities to ask the pharmacy representatives questions at the community pharmacy | 136 (58.9) | 71 (30.7) | 16 (6.9) | 3 (1.3) | 5 (2.2) | 4 ± 0.78 |
| The community pharmacy had the necessary resources for drug information | 138 (59.7) | 75 (32.5) | 12 (5.2) | 3 (1.3) | 3 (1.3) | 4 ± 0.75 |
| The prescription volume at the community pharmacy helped trainees to learn well during training | 130 (56.3) | 69 (29.9) | 24 (10.4) | 6 (2.6) | 2 (0.8) | 4 ± 0.76 |
Data presented as number (n) and percentage (%); SD: Standard deviation.
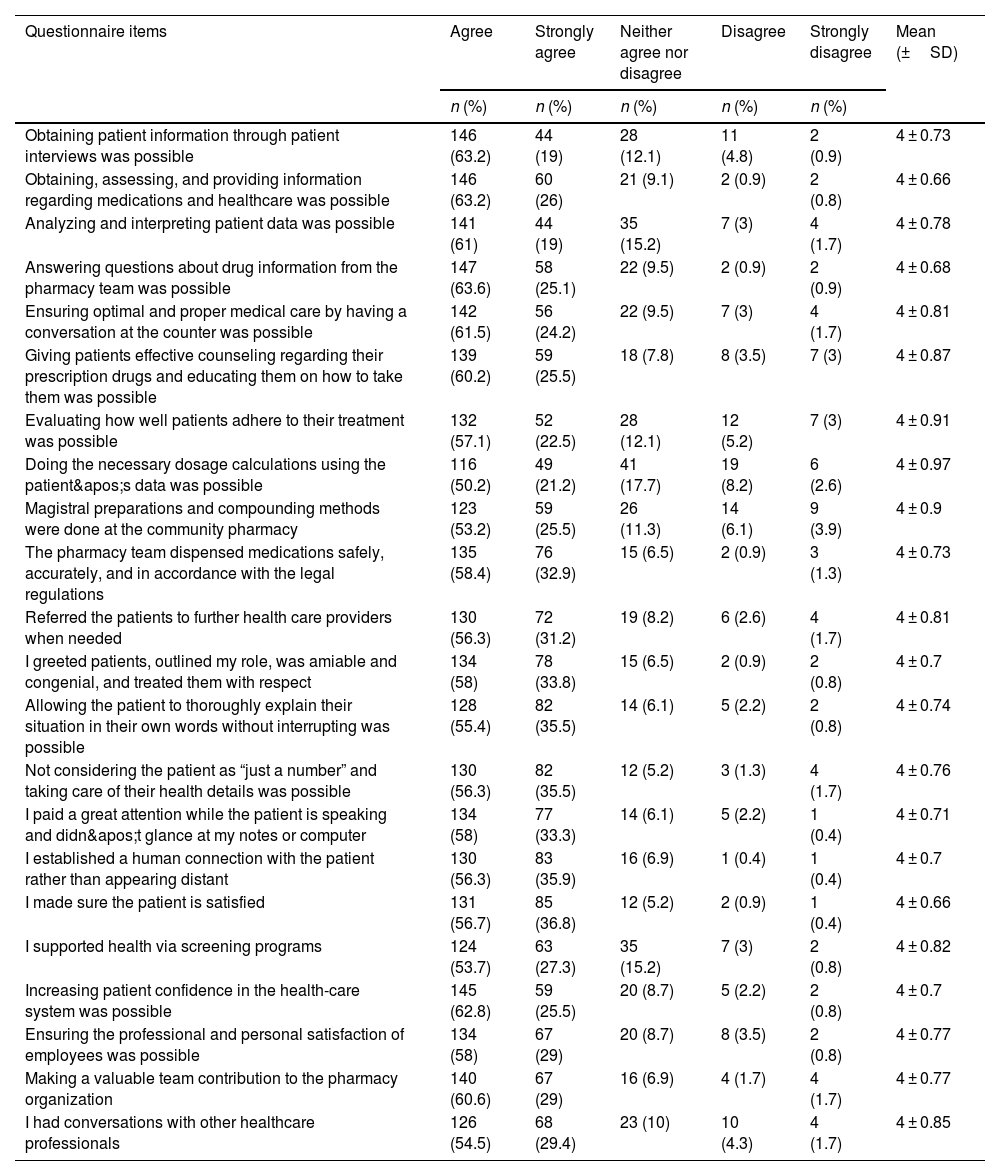
Most of the interns provided strong positive responses and were satisfied with their pharmacy preceptors regarding pharmaceutical training tasks, a patient-oriented manner obtained during the internship, gaining more pharmaceutical knowledge and the chance to interact with other members of the healthcare team. This includes obtaining patient information through patient interviews (82.2%); (mean 4 ± 0.73, p < 0.0001), obtaining, assessing, and providing information regarding medications (89.2%); (mean 4 ± 0.66, p < 0.0001), answering questions about drug information from the pharmacy team (88.7%); (mean 4 ± 0.68, p < 0.0001), ensuring optimal and proper medical care by having a conversation at the counter (85.7%); (mean 4 ± 0.81, p < 0.0001), and giving patients effective counseling regarding their prescription drugs and educating them on how to take (85.7%); (mean 4 ± 0.87, p < 0.0001). Other findings are presented in Table 3.
Pharmaceutical care training and tasks provided by pharmacy preceptors and students during the internship program.
| Questionnaire items | Agree | Strongly agree | Neither agree nor disagree | Disagree | Strongly disagree | Mean (±SD) |
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | ||
| Obtaining patient information through patient interviews was possible | 146 (63.2) | 44 (19) | 28 (12.1) | 11 (4.8) | 2 (0.9) | 4 ± 0.73 |
| Obtaining, assessing, and providing information regarding medications and healthcare was possible | 146 (63.2) | 60 (26) | 21 (9.1) | 2 (0.9) | 2 (0.8) | 4 ± 0.66 |
| Analyzing and interpreting patient data was possible | 141 (61) | 44 (19) | 35 (15.2) | 7 (3) | 4 (1.7) | 4 ± 0.78 |
| Answering questions about drug information from the pharmacy team was possible | 147 (63.6) | 58 (25.1) | 22 (9.5) | 2 (0.9) | 2 (0.9) | 4 ± 0.68 |
| Ensuring optimal and proper medical care by having a conversation at the counter was possible | 142 (61.5) | 56 (24.2) | 22 (9.5) | 7 (3) | 4 (1.7) | 4 ± 0.81 |
| Giving patients effective counseling regarding their prescription drugs and educating them on how to take them was possible | 139 (60.2) | 59 (25.5) | 18 (7.8) | 8 (3.5) | 7 (3) | 4 ± 0.87 |
| Evaluating how well patients adhere to their treatment was possible | 132 (57.1) | 52 (22.5) | 28 (12.1) | 12 (5.2) | 7 (3) | 4 ± 0.91 |
| Doing the necessary dosage calculations using the patient's data was possible | 116 (50.2) | 49 (21.2) | 41 (17.7) | 19 (8.2) | 6 (2.6) | 4 ± 0.97 |
| Magistral preparations and compounding methods were done at the community pharmacy | 123 (53.2) | 59 (25.5) | 26 (11.3) | 14 (6.1) | 9 (3.9) | 4 ± 0.9 |
| The pharmacy team dispensed medications safely, accurately, and in accordance with the legal regulations | 135 (58.4) | 76 (32.9) | 15 (6.5) | 2 (0.9) | 3 (1.3) | 4 ± 0.73 |
| Referred the patients to further health care providers when needed | 130 (56.3) | 72 (31.2) | 19 (8.2) | 6 (2.6) | 4 (1.7) | 4 ± 0.81 |
| I greeted patients, outlined my role, was amiable and congenial, and treated them with respect | 134 (58) | 78 (33.8) | 15 (6.5) | 2 (0.9) | 2 (0.8) | 4 ± 0.7 |
| Allowing the patient to thoroughly explain their situation in their own words without interrupting was possible | 128 (55.4) | 82 (35.5) | 14 (6.1) | 5 (2.2) | 2 (0.8) | 4 ± 0.74 |
| Not considering the patient as “just a number” and taking care of their health details was possible | 130 (56.3) | 82 (35.5) | 12 (5.2) | 3 (1.3) | 4 (1.7) | 4 ± 0.76 |
| I paid a great attention while the patient is speaking and didn't glance at my notes or computer | 134 (58) | 77 (33.3) | 14 (6.1) | 5 (2.2) | 1 (0.4) | 4 ± 0.71 |
| I established a human connection with the patient rather than appearing distant | 130 (56.3) | 83 (35.9) | 16 (6.9) | 1 (0.4) | 1 (0.4) | 4 ± 0.7 |
| I made sure the patient is satisfied | 131 (56.7) | 85 (36.8) | 12 (5.2) | 2 (0.9) | 1 (0.4) | 4 ± 0.66 |
| I supported health via screening programs | 124 (53.7) | 63 (27.3) | 35 (15.2) | 7 (3) | 2 (0.8) | 4 ± 0.82 |
| Increasing patient confidence in the health-care system was possible | 145 (62.8) | 59 (25.5) | 20 (8.7) | 5 (2.2) | 2 (0.8) | 4 ± 0.7 |
| Ensuring the professional and personal satisfaction of employees was possible | 134 (58) | 67 (29) | 20 (8.7) | 8 (3.5) | 2 (0.8) | 4 ± 0.77 |
| Making a valuable team contribution to the pharmacy organization | 140 (60.6) | 67 (29) | 16 (6.9) | 4 (1.7) | 4 (1.7) | 4 ± 0.77 |
| I had conversations with other healthcare professionals | 126 (54.5) | 68 (29.4) | 23 (10) | 10 (4.3) | 4 (1.7) | 4 ± 0.85 |
Data presented as number (n) and percentage (%); SD: Standard deviation.
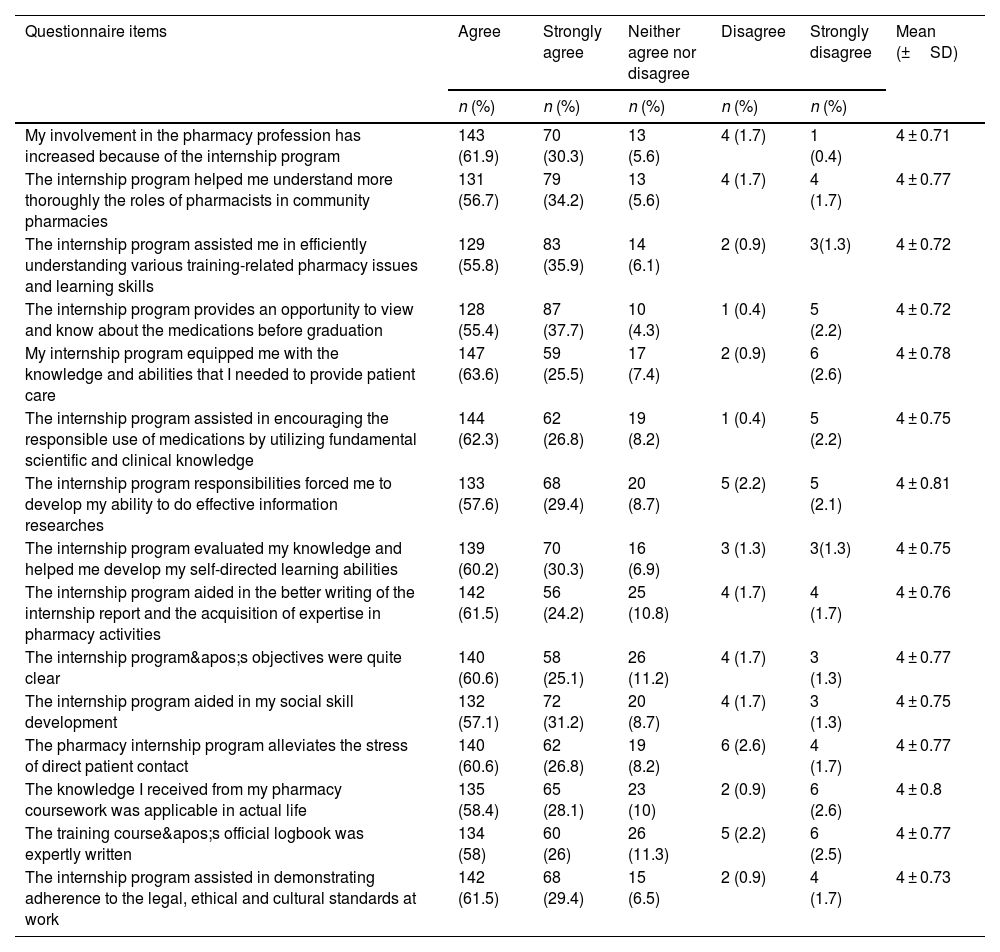
Table 4 shows that the majority of the trainees indicated agreement or strong agreement that their internship experience had increased their involvement in the pharmacy profession (92.2%); (mean 4 ± 0.71, p < 0.0001). This was also reported by 89.1% of the respondents that the internship program equipped them with the knowledge and abilities to provide patient care (mean 4 ± 0.78, p < 0.0001). About 89.1% (mean 4 ± 0.75, p < 0.0001) mentioned that the internship program assisted in encouraging the responsible use of medications, 90.5% (mean 4 ± 0.75, p < 0.0001) reported that the internship program evaluated knowledge and helped to develop self-directed learning abilities, and 87.4% (mean 4 ± 0.77, p < 0.0001) showed that the pharmacy internship program alleviates the stress of direct patient contact. Other results are also summarized in Table 4.
Perception of pharmacy students about the outcomes of the internship program.
| Questionnaire items | Agree | Strongly agree | Neither agree nor disagree | Disagree | Strongly disagree | Mean (±SD) |
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | ||
| My involvement in the pharmacy profession has increased because of the internship program | 143 (61.9) | 70 (30.3) | 13 (5.6) | 4 (1.7) | 1 (0.4) | 4 ± 0.71 |
| The internship program helped me understand more thoroughly the roles of pharmacists in community pharmacies | 131 (56.7) | 79 (34.2) | 13 (5.6) | 4 (1.7) | 4 (1.7) | 4 ± 0.77 |
| The internship program assisted me in efficiently understanding various training-related pharmacy issues and learning skills | 129 (55.8) | 83 (35.9) | 14 (6.1) | 2 (0.9) | 3(1.3) | 4 ± 0.72 |
| The internship program provides an opportunity to view and know about the medications before graduation | 128 (55.4) | 87 (37.7) | 10 (4.3) | 1 (0.4) | 5 (2.2) | 4 ± 0.72 |
| My internship program equipped me with the knowledge and abilities that I needed to provide patient care | 147 (63.6) | 59 (25.5) | 17 (7.4) | 2 (0.9) | 6 (2.6) | 4 ± 0.78 |
| The internship program assisted in encouraging the responsible use of medications by utilizing fundamental scientific and clinical knowledge | 144 (62.3) | 62 (26.8) | 19 (8.2) | 1 (0.4) | 5 (2.2) | 4 ± 0.75 |
| The internship program responsibilities forced me to develop my ability to do effective information researches | 133 (57.6) | 68 (29.4) | 20 (8.7) | 5 (2.2) | 5 (2.1) | 4 ± 0.81 |
| The internship program evaluated my knowledge and helped me develop my self-directed learning abilities | 139 (60.2) | 70 (30.3) | 16 (6.9) | 3 (1.3) | 3(1.3) | 4 ± 0.75 |
| The internship program aided in the better writing of the internship report and the acquisition of expertise in pharmacy activities | 142 (61.5) | 56 (24.2) | 25 (10.8) | 4 (1.7) | 4 (1.7) | 4 ± 0.76 |
| The internship program's objectives were quite clear | 140 (60.6) | 58 (25.1) | 26 (11.2) | 4 (1.7) | 3 (1.3) | 4 ± 0.77 |
| The internship program aided in my social skill development | 132 (57.1) | 72 (31.2) | 20 (8.7) | 4 (1.7) | 3 (1.3) | 4 ± 0.75 |
| The pharmacy internship program alleviates the stress of direct patient contact | 140 (60.6) | 62 (26.8) | 19 (8.2) | 6 (2.6) | 4 (1.7) | 4 ± 0.77 |
| The knowledge I received from my pharmacy coursework was applicable in actual life | 135 (58.4) | 65 (28.1) | 23 (10) | 2 (0.9) | 6 (2.6) | 4 ± 0.8 |
| The training course's official logbook was expertly written | 134 (58) | 60 (26) | 26 (11.3) | 5 (2.2) | 6 (2.5) | 4 ± 0.77 |
| The internship program assisted in demonstrating adherence to the legal, ethical and cultural standards at work | 142 (61.5) | 68 (29.4) | 15 (6.5) | 2 (0.9) | 4 (1.7) | 4 ± 0.73 |
Data presented as number (n) and percentage (%); SD: Standard deviation.
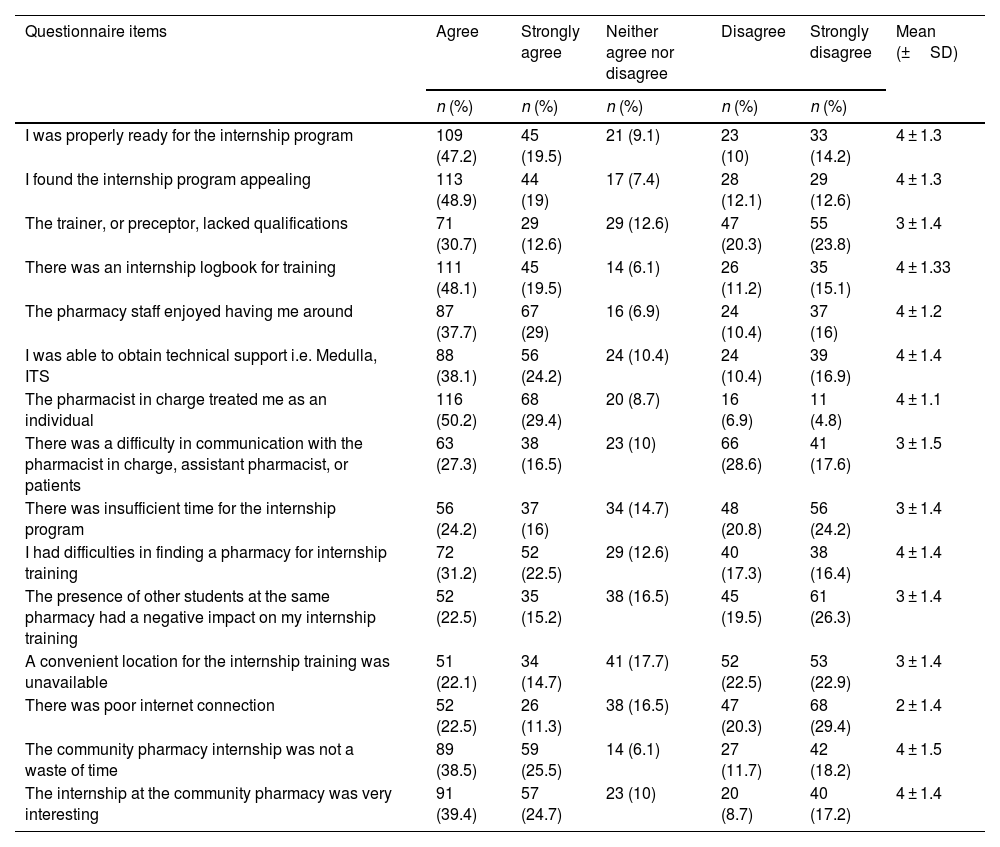
The majority of the trainees reported disagreement regarding the preceptor lacking qualifications (43.3%); (mean 3 ± 1.4, p < 0.0001), the presence of other students at the same pharmacy had a negative impact on my internship training (45.8%); (mean 3 ± 1.4, p < 0.0001), there was insufficient time for the internship program (45%); (mean 3 ± 1.4, p < 0.0001), and there was a difficulty in communication with the pharmacist in charge, assistant pharmacist, or patients because of a language barrier (46.2%); (mean 3 ± 1.5, p < 0.0001). However, most of the trainees reported some barriers and challenges during the internship, including that there were difficulties in finding a pharmacy for internship training (53.7%); (mean 4 ± 1.4, p < 0.0001), as shown in Table 5.
Perception of the pharmacy students toward the barriers during the internship program.
| Questionnaire items | Agree | Strongly agree | Neither agree nor disagree | Disagree | Strongly disagree | Mean (±SD) |
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | ||
| I was properly ready for the internship program | 109 (47.2) | 45 (19.5) | 21 (9.1) | 23 (10) | 33 (14.2) | 4 ± 1.3 |
| I found the internship program appealing | 113 (48.9) | 44 (19) | 17 (7.4) | 28 (12.1) | 29 (12.6) | 4 ± 1.3 |
| The trainer, or preceptor, lacked qualifications | 71 (30.7) | 29 (12.6) | 29 (12.6) | 47 (20.3) | 55 (23.8) | 3 ± 1.4 |
| There was an internship logbook for training | 111 (48.1) | 45 (19.5) | 14 (6.1) | 26 (11.2) | 35 (15.1) | 4 ± 1.33 |
| The pharmacy staff enjoyed having me around | 87 (37.7) | 67 (29) | 16 (6.9) | 24 (10.4) | 37 (16) | 4 ± 1.2 |
| I was able to obtain technical support i.e. Medulla, ITS | 88 (38.1) | 56 (24.2) | 24 (10.4) | 24 (10.4) | 39 (16.9) | 4 ± 1.4 |
| The pharmacist in charge treated me as an individual | 116 (50.2) | 68 (29.4) | 20 (8.7) | 16 (6.9) | 11 (4.8) | 4 ± 1.1 |
| There was a difficulty in communication with the pharmacist in charge, assistant pharmacist, or patients | 63 (27.3) | 38 (16.5) | 23 (10) | 66 (28.6) | 41 (17.6) | 3 ± 1.5 |
| There was insufficient time for the internship program | 56 (24.2) | 37 (16) | 34 (14.7) | 48 (20.8) | 56 (24.2) | 3 ± 1.4 |
| I had difficulties in finding a pharmacy for internship training | 72 (31.2) | 52 (22.5) | 29 (12.6) | 40 (17.3) | 38 (16.4) | 4 ± 1.4 |
| The presence of other students at the same pharmacy had a negative impact on my internship training | 52 (22.5) | 35 (15.2) | 38 (16.5) | 45 (19.5) | 61 (26.3) | 3 ± 1.4 |
| A convenient location for the internship training was unavailable | 51 (22.1) | 34 (14.7) | 41 (17.7) | 52 (22.5) | 53 (22.9) | 3 ± 1.4 |
| There was poor internet connection | 52 (22.5) | 26 (11.3) | 38 (16.5) | 47 (20.3) | 68 (29.4) | 2 ± 1.4 |
| The community pharmacy internship was not a waste of time | 89 (38.5) | 59 (25.5) | 14 (6.1) | 27 (11.7) | 42 (18.2) | 4 ± 1.5 |
| The internship at the community pharmacy was very interesting | 91 (39.4) | 57 (24.7) | 23 (10) | 20 (8.7) | 40 (17.2) | 4 ± 1.4 |
Data presented as number (n) and percentage (%); SD: Standard deviation.
Since pharmacists are on the front lines of patient care, it is vital to focus on their education and training so that they can play a leading role in patient care, supporting patients using medications as efficiently and affordably as possible with strong interpersonal and communication skills. The study findings showed that the students were satisfied with their training experiences and had positive perspectives about the skills, knowledge, and attitudes they had acquired. Students' perceptions of the trainer, the training setting, and their perspectives on the training's outcome have been reported in several earlier studies. These findings are consistent with earlier studies in Saudi Arabia,4 Nepal,5 Qatar,6 Ethiopia,21 and the Philippines.22 The universities and the training settings must create a professional agreement that outlines the training's objectives as well as the practice's responsibilities and standards with relation to students' education. Therefore, it is crucial to assign students to specified training settings with full responsibility to ensure that all professional and learning competencies are satisfied. In the current study, the majority of the students reported favorable feedback for their pharmacy training programs and relevant, easily accessible drug information sources. This provided them with direction on how to effectively provide pharmaceutical care services to patients in a community pharmacy setting and provided a practical setting to enable students to interact with patients. Similar results were also reported in previous studies in Nepal,5 Qatar,6 and Jordan.20
Since the effectiveness and quality of preceptors largely determine the quality of pharmacy education, the interns should constantly have the support of their preceptors, be available to understand their requirements as students, and make an effort to bridge the gaps between theoretical and practical aspects.23 Notably, the preceptor's encouragement and support are crucial elements since they will enhance the student's performance. Their knowledge of the standards that satisfy the needs of students will subsequently boost their trust in themselves. Therefore, the effectiveness and quality of the preceptor have a major influence on the quality of community pharmacy training.24 In the present study, most of the interns provided positive responses, indicating agreement or strong agreement with the corresponding sentences. They were satisfied with their pharmacy preceptors regarding pharmaceutical training tasks, a patient-oriented manner obtained during the internship, gaining more pharmaceutical knowledge and the chance to interact with other members of the healthcare team. Additionally, they revealed the preceptors' effective interpersonal skills, which have benefitted their training. Meanwhile, the respondents reported that their preceptors had supported and encouraged them during their training time which led to student satisfaction improvement and training productivity. Similar to our findings, Abu Farha et al.20 and Zeitoun et al.25 reported that the increased rate of satisfaction in the community pharmacy context was related to improved interaction between students and site preceptors. Furthermore, they indicated the critical function of the preceptors in offering encouragement and assistance for acquiring more practical knowledge. These results are also in accordance with those previous studies carried out by Almetwazi et al.,4 El Hajj et al.,6 and Alnajjar and Mohammed,15 from which around half of the students were satisfied with their preceptors, who encouraged them during the period of training, with 51.0%, 49.0%, and 40.8%, respectively.
Furthermore, students reported having a good opportunity to meet with patients; the pharmacy internship program reduces the stress of direct patient contact, and students were able to conduct patient interviews to acquire patient information. This allowed students the opportunity to practice communication skills, patient counseling, and patient interviews under the supervision of professional pharmacists, preparing them to be a patient-centered member of the pharmacy team with strong interpersonal and communication abilities. This is consistent with previous studies that highlight the importance of increased student-patient interactions, which is important for their experience satisfaction.20,25 The present study showed that most of the participants were permitted by their preceptors to actively perform their training, be involved in a patient-orientated manner, and provide them the opportunity to interact with other healthcare personnel on the team. However, these results are lower than those reported in other relevant studies conducted in Saudi Arabia by Almetwazi et al. (67%),4 and Canada by Kassam (93%),26 but higher than the study conducted in the United Arab Emirates by Alnajjar and Mohammed.15
While the development of professional responsibilities is regarded as critical for healthcare professions, learning outcomes related to these skills should be addressed during pharmacy degree courses. As a result, the interns acknowledged that they developed the necessary skills required to obtain, assess, and give information regarding drugs, and they indicated that their internship program equipped them with the knowledge and abilities that they needed to provide patient care. Furthermore, the majority of the respondents indicated agreement or strong agreement that their internship experience had increased their involvement in the pharmacy profession, and they have learnt new skills that were not covered during theoretical study., The internship program assisted in encouraging the responsible use of medications, and the pharmacy internship program alleviated the stress of direct patient contact. These findings were consistent with a study conducted in the United Arab Emirates by Alnajjar and Mohammed,7 in Denmark by Sorensen et al.,24 and in Jordan by Abu Farha et al.20 Most of the trainees reported few barriers during the internship. Difficulties in finding a pharmacy for internship training was particularly mentioned.This finding was similar to previous studies that have reported few barriers.27
To the best of our knowledge, this is the first national study conducted in Türkiye to explore the perceptions and the experience of undergraduate pharmacy students of their training practices in community pharmacies and to identify the related barriers during the internship training program. Notably, the training program is designed to enable students to enroll in an educational and learning program that will enable them to become skilled pharmacists.The study can provide insights for the development of future internship programs. However, some limitations have been encountered with the present study. A self-administered questionnaire was used to collect the data, which could have led to social desirability bias because students might not have accurately reflected their own behaviors. Additionally, the results may not be as widely applicable as the data was gathered via Google-based questionnaire. Taking these limitations into consideration, it may be highly suggested to conduct further research that could use qualitative techniques to delve deeper into aspects such as perceived barriers and the role of the preceptor. Furthermore, it is also useful to assess undergraduate pharmacy students' perceptions and experiences regarding their training practices in community pharmacies among university students across the whole country.
In conclusion, the findings of the current study revealed that pharmacy students reported a good level of experience and knowledge during their internship and had favorable perceptions of the training sites and preceptors. It is recommended that the learning outcomes related to internship programs should be addressed during pharmacy degree courses and structured preparation programs could be implemented by the pharmacy schools in advance to the start of the internship. In addition, collaboration with the preceptors of the community pharmacies for systematic and productive internship programs would be very useful and effective for the internship process.
Informed consentInformed consent was obtained from all participants enrolled in the study.
Ethics approvalThe study was approved by the Ethics Committee of Istinye University (No. 24-44).
FundingThis research received no funding or specific grant from any funding agency in the public, commercial sectors. All costs associated with its execution were covered by the author, Inci Kayin.
The authors have no conflicts of interest to declare.