This article briefly describes the history of formal CME/CPD in the US and the significant work that has developed into major advances in the field of CME, including innovative learning formats by the American Academy of Family Physicians, the American Medical Association and the American Osteopathic Association as the three organizations that own the three major CME credit systems. The description of these advances include the evolution, although not yet completed, from a time metric to a value metric as the way to quantify involvement in CME on the part of physicians. It also briefly describes how the credit systems have evolved from accepting participation to requiring a higher level of achievement or active involvement in the activity in order to receive CME credit. It then highlights Performance Improvement CME as one of the learning formats recognized for CME credit. Each of the three CME credit systems offers multiple ways for physicians to earn CME credit and many, but not all, can be found in all three of them. As an example, the list of different ways to receive credit under the AMA CME credit system is provided.
The article goes on to describe how the specialty certification philosophy has evolved, using the American Boards of Medical Specialties (ABMS) as an example, from a lifetime certificate for most specialties to an ongoing engagement with educational activities and quality improvement efforts to maintain certification. The role that CME/CPD plays in that philosophy is also described. It then discusses the current licensing system in the US, the changes that have been proposed by the Federation of Medical Boards and the possible role of CME/CPD in this new framework as well.
The article concludes with a reference to the research evidence in support of the effectiveness of CME/CPD and the impact that Continuous Quality Improvement and Performance Improvement have had on CME/CPD, on the new program to maintain specialty certification and on the proposed new licensure framework, and how they all interact.
En este artículo se describe brevemente la historia de la educación médica continua (EMC) y del desarrollo profesional continuo (DPC) en los Estados Unidos, así como el trabajo significativo que ha dado lugar a los mayores avances en el campo de la EMC, incluidos los formatos de aprendizaje innovadores de la American Academy of Family Physicians, la American Medical Association (AMA) y la American Osteopathic Association como organizaciones poseedoras de los tres principales sistemas de créditos de EMC. La descripción de estos avances incluye la evolución, aún incompleta, de una medida por tiempo a una medida por valor como método para cuantificar la implicación en la EMC por parte de los médicos. Por otro lado, también se describe la evolución de los sistemas de créditos desde la aceptación de la participación hasta el requisito de un nivel de resultados más alto o la implicación activa en la actividad para recibir el crédito de EMC. Más adelante se hace hincapié en la EMC de mejora del desempeño como uno de los formatos de aprendizaje reconocidos para el crédito de EMC. Los tres sistemas de créditos ofrecen a los médicos múltiples maneras de obtener créditos de EMC, y muchas, aunque no todas, se encuentran en los tres. A modo de ejemplo, se incluye la lista de las diferentes maneras para obtener créditos según el sistema de créditos de EMC de la AMA.
El artículo continúa con una descripción de la evolución de la filosofía de certificación por especialidades, utilizando como ejemplo el ABMS (American Boards of Medical Specialties), desde un certificado de por vida para casi todas las especialidades hasta una participación continua en actividades educativas y un compromiso con la mejora de la calidad para conservar la certificación. Además, también se describe el papel de la EMC y el DPC en esa filosofía. A continuación se aborda la cuestión del sistema estadounidense de obtención de licencias actual, los cambios propuestos por la Federation of Medical Boards y la posible función de la EMC y el DPC en este marco.
El artículo concluye con una referencia a las pruebas de investigaciones que respaldan la eficacia de la EMC y el DPC y el efecto que la mejora continua de la calidad y la mejora del desempeño han tenido en la EMC y el DPC, en el nuevo programa para mantener el certificado de la especialidad, y en el nuevo marco de licenciatura propuesto, y cómo se relacionan entre ellos.
This article will attempt to briefly summarize Continuing Professional Development for physicians, the process for maintaining specialty/subspecialty certification, the laws and regulations governing licensure to practice medicine, and the integration of quality improvement concepts into those three areas of their professional life in the United States. It will then discuss how the interaction of those areas of professional life interact in an effort to create an environment that aims to support the professional growth of physicians, improve patient care and protect the public from individuals that are not qualified to practice medicine. Examples will be used to illustrate the concepts discussed and references are provided for a more in depth review of the systems described.
Continuing Physician Professional Development in the United StatesThe medical profession has long realized the importance of continuing professional development. In the Aphorisms of Hippocrates, the first one reads: “Life is short, and Art long; the crisis fleeting; experience perilous, and decision difficult. The physician must not only be prepared to do what is right himself, but also to make the patient, the attendants, and externals cooperate.”1 While 2400 years ago the term continuing professional development (CPD) was not yet in use, there was recognition that physicians need to continue to learn the art throughout their professional life and that realization has been echoed multiple times over the centuries. Postgraduate Medical Education In the United States, a report commissioned by the AMA Council on Medical Education, published in 1955, and authored by Douglas D. Vollan, MD, starts with a quote from Maimonides’ Daily Prayer of a Physician: “May there never develop in me the notion that my education is complete, but give me the strength and leisure and zeal continually to enlarge my knowledge.” Dr. Vollan goes on to write in the report: “The continuing education of a physician throughout his professional life is absolutely essential if he is to use judiciously and effectively the new developments in the diagnosis, treatment, and prevention of disease that are necessary for adequate medical care.”2
Just as medical school education evolved and became more formalized and structured, and the training in the different specialties also evolved in a similar way, some of the activities that comprise the universe of professional development activities have become more formalized as well. In the United States, the first continuing medical education (CME) credit system was created by the American Academy of Family Physicians (AAFP), known at the time as the American Academy of General Practice, in 1947. The AAFP, from its inception, required members to engage in 150hours every three years of what at the time was referred to as postgraduate education in order to maintain membership in the organization. That requirement continues today. The types of AAFP CME credit have evolved over the years and currently there are two: AAFP Prescribed Credit and AAFP Elective Credit. AAFP Prescribed Credit must be directly related to patient care or a physician's ability to provide patient care or select nonclinical topics. In addition, the development of the educational activity must be carried out with the participation of a family physician who is also an AAFP member to ensure that if focuses on the educational needs of the intended audience: family physicians.3
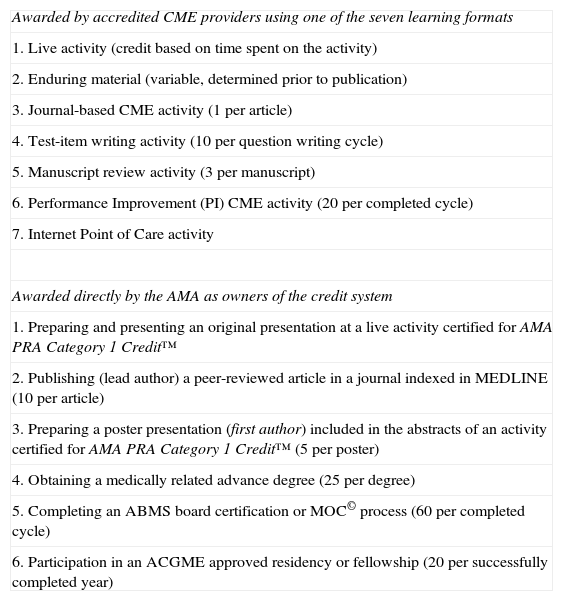
Founded in 1847, the American Medical Association (AMA) had an interest in “postgraduate medical education” as far back as the early 1900s. After several initiatives, including the Vollan Report referenced earlier, the AMA started a formal system to approve organizations as sponsors of CME activities in 1967. In 1968, the AMA created the Physician Recognition Award (PRA) to recognize and encourage physicians to voluntarily engage in 150hours of CME every three years. The AMA PRA CME credit system was created in support of the Award. There are currently two types of AMA CME credit: AMA PRA Category 1 Credit™ and AMA PRA Category 2 Credit™. In the AMA system there are currently approximately 1900 accredited CME providers in the US which are granted the privilege by the AMA to award AMA PRA Category 1 Credit™, provided they comply with AMA PRA rules. The current accreditation system has been in place since 1981 when the AMA, together with six other national organizations, created the Accreditation Council for Continuing Medical Education (ACCME) to determine if an organization merits being granted the privilege to award AMA PRA Category 1 Credit™ by the AMA. This accreditation function by the ACCME, together with state medical societies, had previously been performed first by the AMA, as noted earlier, and then by a group of organizations led by the AMA. Physicians may also claim CME credit directly from the AMA, as the owner of the AMA PRA CME credit system, and receive AMA PRA Category 1 Credit™ for engaging in six additional categories of activities that have educational value as determined by the Council on Medical Education (table 1). Physicians may also self-report AMA PRA Category 2 Credit™ based on guidance provided by the AMA (table 2).4,5
AMA PRA Category 1 Credit™* (Number of credits awarded in parenthesis).
| Awarded by accredited CME providers using one of the seven learning formats |
| 1. Live activity (credit based on time spent on the activity) |
| 2. Enduring material (variable, determined prior to publication) |
| 3. Journal-based CME activity (1 per article) |
| 4. Test-item writing activity (10 per question writing cycle) |
| 5. Manuscript review activity (3 per manuscript) |
| 6. Performance Improvement (PI) CME activity (20 per completed cycle) |
| 7. Internet Point of Care activity |
| Awarded directly by the AMA as owners of the credit system |
| 1. Preparing and presenting an original presentation at a live activity certified for AMA PRA Category 1 Credit™ |
| 2. Publishing (lead author) a peer-reviewed article in a journal indexed in MEDLINE (10 per article) |
| 3. Preparing a poster presentation (first author) included in the abstracts of an activity certified for AMA PRA Category 1 Credit™ (5 per poster) |
| 4. Obtaining a medically related advance degree (25 per degree) |
| 5. Completing an ABMS board certification or MOC© process (60 per completed cycle) |
| 6. Participation in an ACGME approved residency or fellowship (20 per successfully completed year) |
The Physician's Recognition Award and credits system — Information for accredited providers and physicians. 2010 revision. Pages 4-7 and 9.5
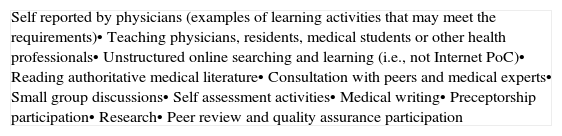
AMA PRA Category 2 Credit™*
| Self reported by physicians (examples of learning activities that may meet the requirements)• Teaching physicians, residents, medical students or other health professionals• Unstructured online searching and learning (i.e., not Internet PoC)• Reading authoritative medical literature• Consultation with peers and medical experts• Small group discussions• Self assessment activities• Medical writing• Preceptorship participation• Research• Peer review and quality assurance participation |
The Physician's Recognition Award and credits system — Information for accredited providers and physicians. 2010 revision. Page 10.5
The AMA has recognized for a long time the value of CME activities provided in other systems outside the US. That recognition has been formalized in two ways: 1) The International Conference Recognition Program of the AMA reviews, at their request, major conferences or congresses that meet the AMA guidelines for CME, presented by international organizations, and certifies them for AMA PRA Category 1 Credit™. 2) The AMA also has agreements with the European Union of Medical Specialists/European Accreditation Council for Continuing Medical Education and with the Royal College of Physicians and Surgeons of Canada whereby the AMA will convert the CME credit issued to physicians by those two systems for participation in select CME activities to AMA PRA Category 1 Credit™.
Founded in 1887, the American Osteopathic Association (AOA) represents osteopathic physicians or doctors of osteopathic medicine. There are two paths to becoming a physician in the US. One is by obtaining an MD (Medicinae Doctor or Doctor of Medicine) or allopathic degree. The other path is by obtaining a DO (Doctor of Osteopathic Medicine) or osteopathic degree. The two paths are similar in many ways. Entrance to either an allopathic or osteopathic medical school requires a Bachelor's Degree, with an expectation that it include a number of premedical courses that may vary by school, and taking the Medical College Admission Test. Both the allopathic and the osteopathic medical schools typically include four years of study, consisting of a scientifically based curriculum. One difference is that osteopathic schools, because of the emphasis on the musculoskeletal system, require 200hours of manipulation and manual therapy training in the curriculum. Residencies in both paths are similar, lasting between three and seven years. Currently the two residency systems are working to unite into one single system of specialty training for both MDs and DOs. The licensing requirements are also similar although the licensing exams are produced by different organizations.6
The AOA had also been interested in postgraduate medical education prior to the creation of its CME program in 1973 and, similarly to the AAFP system, it mandated at its inception 150hours of CME for AOA members in order to maintain membership. Prior to 1973, and as early as 1949, osteopathic physicians had to meet CME requirements set by some state licensing boards. There are currently four AOA CME Categories of Credit: 1-A, 1-B, 2-A and 2-B. The “1” denotes content that is unique to the osteopathic medical profession while the “2” refers to medical education not specific to the osteopathic profession. The “A” refers to formal or live activities while “B” refers to less formal education. Category 1-A can only be sponsored by an AOA accredited Category 1CME sponsor, accredited by the AOA Council on CME.7
Similarly to the way that medical school and specialty education continues to evolve to meet the needs of current and future physicians and patients, so has CME continued to adapt to a changing environment and to explore more effective ways of learning in order to help physicians and improve patient care. The three CME credit systems in the US, while independent from each other, cooperate and collaborate in the advancement of this stage of physician education, the longest stage of physician education. All three systems have moved from a time based metric to a value based metric for most types of activities. And for many CME activities, but not yet for all, credit is being earned for accomplishing or meeting educational or performance goals and not just for participation. These trends can be see in all three credit systems. This article will use the AMA CME credit system as an example to illustrate some of these trends.
The three systems changed the terminology from hours to credits as part of that evolution from a time based metric to a value based metric. In table 1, the only Learning Format in which the participating physician is awarded credit based solely on the amount of time he or she has spent participating in the activity is “Live Activity”. The amount of credit awarded for the other learning formats can be found in parenthesis. In live activities a physician may be asked if, as a result of the activity, there will be a change in competence, performance, or patient outcomes. But in the other formats there may be an objective evaluation, such as passing a post test (e.g., Enduring Materials and Journal CME), or the successful completion of a task (e.g., Manuscript Review), or the requirement or the collection of patient outcomes data (e.g., Performance Improvement CME), before a physician may receive CME credit. The details about the educational requirements for each format, and the structural quality markers imbedded in most of them, can be found in the reference at the bottom of the table.
One of the Learning Formats listed in table 1 is Performance Improvement CME (PI CME). PI CME is a three stage learning model approved for AMA PRA Category 1 Credit™ by the AMA Council on Medical Education in September 2004, as a result of a pilot study lasting several years and sponsored by the AMA in collaboration with the AAFP and other stakeholders. Inspired by the work of W. Edwards Deming and Joseph W. Juran, and based on a quality improvement cycle, this Learning Format is a structured long-term process that can be developed by an accredited CME provider in which evidence-based measures and quality improvement (QI) interventions, not traditionally thought of as CME, are used to change physician performance. There are three stages to the format. In Stage A (Learning from current practice performance assessment) the physician(s), assisted by the CME staff, assesses his or her practice using evidenced based performance measures, either through chart reviews, record reviews, electronic health records, registry data, or other appropriate data sources. The physician(s) then analyzes the results to determine the cause(s) for any deficiencies or less than desirable performance and identifies appropriate intervention(s). In Stage B (Learning from the application of PI to patient care) the physician(s) implements interventions based on the results of Stage A. The interventions generally involve changes to the processes or procedures that are in place to provide the care being evaluated, involve other members of the health care team, and are rarely purely didactic activities, unless the reason for the substandard performance is a lack of knowledge. In Stage C (Learning from the evaluation of the PI effort) there is a re-assessment and reflection on performance in practice, measured after implementation of interventions in Stage B, by comparing the results of the re-assessment to the assessment done in Stage A and determining the process and/or outcomes changes that resulted from conducting the PI CME activity. For the completion of the three stage cycle the physician learner earns 20 CME credits in either the AMA or the AAFP credit system.5,8
A physician will not learn everything that he or she needs to know in medical school or residency, neither can it be learned only through formal CME/CPD activities certified for CME credit. Not all activities that advance the education of physicians can be certified for CME credit nor do they need to be. Therefore, the AMA CME system recognizes a variety of educational pursuits for which it awards AMA PRA Category 1 Credit™ directly and which are also listed in table 1. AMA PRA Category 2 Credit™ allows physicians to claim CME credit for additional professional development activities that they determine are a worthwhile educational experience related to their practice. But a physician's education should not stop there, after all, as Don José de Letamendi Manjarrés (1828-1897), so eloquently expressed, “El médico que solo medicina sabe, ni medicina sabe.”9
Specialty certification in the United StatesWith two paths to the practice of medicine in the US, allopathic and osteopathic medical education, each also has had its own pathway, although similar to each other, to obtain and maintain specialty board certification. Originally the specialty boards provided certification, lifetime in most specialties, after the successful completion of appropriate residency/fellowship training and additional requirements such as a secure exam(s). Over time specialty certificates became time limited with a requirement to take and pass a recertifying exam every 7-10 years in order to maintain one's certification. In the recent past the requirement has changed to a concept of ongoing engagement in self-assessment to guide continuing learning and improvement as well as the use of performance improvement principles to enhance the quality of care while also continuing the practice of the secure exam. This program or process, created by the American Board of Medical Specialties (ABMS) as the umbrella organization for the 24 allopathic boards, has been named the Maintenance of Certification (MOC®) program. The American Osteopathic Association's Bureau of Osteopathic Specialists (AOA-BOS) and its 18 certifying boards has instituted a similar program, the Osteopathic Continuous Certificate (OCC) process. We will illustrate the concept using the ABMS MOC® program as an example. A more in depth discussion, by Hawkins et al., on the theory and evidence for it was published in 2013.10
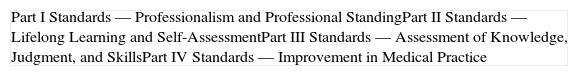
The ABMS MOC® framework consists of four standards (table 3). The most recent revision, approved January 15, 2014, by the ABMS Board of Directors for implementation in January 2015, expands on the guidance previously provided.11 The framework aims to incorporate in each cycle all six ABMS/Accreditation Council for Graduate Medical Education (ACGME) Core Competencies: Practice-Based Learning & Improvement; Patient Care & Procedural Skills; Systems-based Practice; Medical Knowledge; Interpersonal & Communication Skills; and Professionalism. Part I Standards-Professionalism and Professional Standing, includes an expectation for the physician to hold a valid, unrestricted license to practice medicine. Part II-Lifelong Learning and Self-Assessment describes the expectations to meet this requirement, for example, through engagement in 25 credits of CME per year, one third of which should incorporate self-assessment. Part III Standards-Assessment of Knowledge, Judgment, and Skills, requires the “examination of diplomates’ knowledge of core content, judgment, and skills in the specialty no less often than every 10 years.” There is now, with this most recent revision, the expectation that diplomates will be provided with feedback on their performance on secure examinations so that it can inform further their professional development, expanding the role of the exam beyond that of summative feedback to now provide formative feedback as well. Part IV Standards-Improvement in Medical Practice, aims for “improved patient care through ongoing assessment and improvement in the quality of care provided by diplomates in their individual practices and/or in the larger hospital, health system, or community setting in which the diplomates practice medicine.” The physician may accomplish this by using “registries, patient logs, patient surveys, peer surveys, practice improvement modules, performance improvement CME activities, etc.”
Standards for the American Board of Medical Specialties Program for Maintenance of Certification*
| Part I Standards — Professionalism and Professional StandingPart II Standards — Lifelong Learning and Self-AssessmentPart III Standards — Assessment of Knowledge, Judgment, and SkillsPart IV Standards — Improvement in Medical Practice |
Standards for the ABMS Program for Maintenance of Certification (MOC). For Implementation in January 2015. Approved by the Board of Directors of the American Board of Medical Specialties (ABMS) January 15, 2014.11
The license to practice medicine in the US is awarded by the individual state(s) or territories where a physician practices. Because some of those jurisdictions have different licensing boards for allopathic and for osteopathic physicians, there are 69 licensing or medical boards in the US. The vast majority of licensing boards currently require participation in CME in order for a physician to renew the license to practice medicine. The renewal period varies between one and three years, depending on the licensing board, and the number of required CME credits for those that require CME can be as many as 50 credits per year. Some of the licensing boards also require completion of CME courses on specific topics such as pain management, human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS), patient safety or risk management, at times regardless of whether the topic is related to the individual physician's scope of practice.
The Federation of State Medical Boards (FSMB) is the umbrella organization for the 70 medical boards (one of them is a disciplinary board, not a licensing board) in the US, and all of them are represented in the FSMB House of Delegates. The mission of the FSMB, posted on its website (www.fsmb.org) is that it “leads by promoting excellence in medical practice, licensure, and regulation as the national resource and voice on behalf of state medical boards in their protection of the public.” In an effort to further that purpose, the FSMB developed the concept of Maintenance of Licensure (MOL), which they describe as a “framework for medical license renewal that recognizes the value of continuous professional development.”12 An article detailing some of the literature and policy statements on the topic was published by Chaudhry et al in 201313.
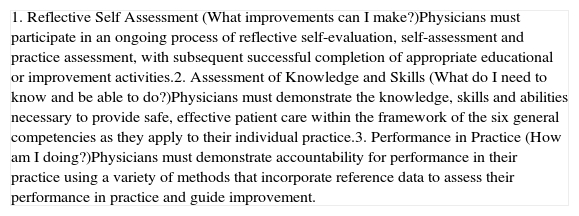
MOL, which would apply to allopathic as well as osteopathic physicians, has not been implemented yet by any licensing board but several of them, working with FSMB, have been piloting some of the concepts. The MOL framework consists of three components (table 4). The first one (Reflective Self Assessment or What improvements can I make?) aims to have physicians determine their education and improvement needs. The second one (Assessment of Knowledge and Skills or What do I need to know and be able to do?) includes the demonstration of “knowledge, skills and abilities” within the context of the physician's practice and the six general ABMS/ACGME competencies already listed. The purpose of the third component (Performance in Practice or How am I doing?) is that physicians assess their performance and engage in improvements. Here too Performance Improvement CME is listed as one of the assessment tools that could be used to demonstrate compliance with this expectation. An MOL Task Force on CPD activities document presented to the FSMB House of Delegates at its 2014 annual meeting12 describes, in Appendix B, how all three components could potentially be met by CME activities that fulfill the descriptions for each one of them while allowing for other non-CME options as well.
Framework of the Federation of State Medical Boards for Maintenance of Licensure*
| 1. Reflective Self Assessment (What improvements can I make?)Physicians must participate in an ongoing process of reflective self-evaluation, self-assessment and practice assessment, with subsequent successful completion of appropriate educational or improvement activities.2. Assessment of Knowledge and Skills (What do I need to know and be able to do?)Physicians must demonstrate the knowledge, skills and abilities necessary to provide safe, effective patient care within the framework of the six general competencies as they apply to their individual practice.3. Performance in Practice (How am I doing?)Physicians must demonstrate accountability for performance in their practice using a variety of methods that incorporate reference data to assess their performance in practice and guide improvement. |
FSMB Maintenance of Licensure (MOL) Task Force on Continuous Professional Development Activities. March 11, 2014.12
Not all physicians in the US are certified in a specialty and board certification in a specialty is not a requirement to obtain a license to practice. In an article published in 2013, Young et al.14 analyzed the 2012 data supplied by the licensing boards and found that there were a total of 812,019 allopathic physicians in the US (out of a total of 878,194 licensees) and 671,755 ABMS boards certified physicians, some of which may be have been osteopathic physicians. Meeting MOC or OCC requirements is needed by physicians in order to maintain their specialty certification, unless they have a lifetime certificate. If implemented in all states and territories, MOL would eventually apply to all physicians.
ConclusionThe responsibility that physicians have to continue to learn throughout their professional lives has been enshrined in the Code of Medical Ethics of the AMA: “A physician shall continue to study, apply, and advance scientific knowledge, maintain a commitment to medical education, make relevant information available to patients, colleagues, and the public, obtain consultation, and use the talents of other health professionals when indicated.” In the US, physician organizations created CME systems that would serve as a framework to require or encourage physicians to engage in educational activities. Research into the effectiveness of CME has been conducted over the years and although a thorough review of the literature is beyond the scope of this article, a number of articles have looked at studies published on the topic and describe the findings including CME's effectiveness and the nuances related to the different types of educational interventions and their relative impact.15–19 While all the different educational interventions have a place in facilitating the journey from novice to master, we need to continue to improve our assessment tools, educational interventions and practice improvement tools, especially using new technology for the new learners.
Quality improvement concepts and philosophy had been making inroads into the medical field for some time, most often in larger organizations such as hospitals, when in 2001 the AMA began its pilot on PI CME. By 2002, the 16 organizations represented in the Conjoint Committee for Continuing Medical Education were on record as supporting the integration of performance improvement into CME.20 By 2013 PI CME, in the AMA system, had grown to a total 548 activities that year with 65,835 physician participants and 8,973 non physician participants. That number is likely to grow as additional CME providers and physicians become more experienced with this still relatively new learning format.
The ultimate goal of the three US CME credit systems, the licensure requirements in each jurisdiction, and the certification requirements for the different specialties, is to advance the well-being of patients and the public by ensuring that physicians are not only qualified but that also continue to learn and improve. The implementation of MOC® and the potential implementation of MOL, and to some extent CME rules and requirements, have caused concerns among physicians as it relates to cost, complexity, time commitments and effectiveness, on top of all the current demands on a physician in today's increasingly complex environment.21 While it is reassuring that all the requirements seem to be emphasizing similar principles of self-assessment, continuing professional development and practice improvement, it will be important to achieve these goals in ways that do not add an undue burden to physicians or the health care system. Particularly, it behooves all the organizations involved to continue to work together to avoid duplication of effort and waste of limited resources. An example of that is the recommendation from the FSMB that physicians that are actively involved in MOC® or OCC in their area of practice should be judged by the licensing boards to be “in substantial compliance with MOL.”12
As long as we keep in mind that our ultimate aims are to advance the art and science of medicine and improve the health of our patients and of the public, we should be able to have systems that work cooperatively to ensure that physicians can continue to advance their knowledge and skills and improve the care they provide.
DisclaimerThe opinions expressed in this article represent those of the author and not necessarily the views or policies of the American Medical Association, the University of Illinois at Chicago College of Medicine, or any other organization with which he is affiliated.
My appreciation goes to my colleagues at the AMA, Mary F. Kelly for her assistance in proofreading the manuscript and Yolanda Davis for her help in obtaining reference articles.