To assess the association between age, parity, nationality, educational level, employment and partner support with depression and anxiety during pregnancy. To determine the impact of the evolution of the COVID-19 pandemic on the anxiety and depression levels of the participants.
MethodCross-sectional descriptive correlational study carried out in the Osakidetza/Basque Health Service, Primary Care, Bizkaia (Spain). A total of 295 pregnant women between 8 and 41 weeks participated. The association between age, parity, nationality, educational level, employment, partner support and COVID-19 incidence rates during the study period and depression (measured with the Edinburgh Postnatal Depression Scale) and anxiety (measured with the State-Anxiety Inventory/STAI-S subscale) scores during pregnancy was measured. A logistic regression model was constructed and odds ratios and their 95% confidence intervals were estimated.
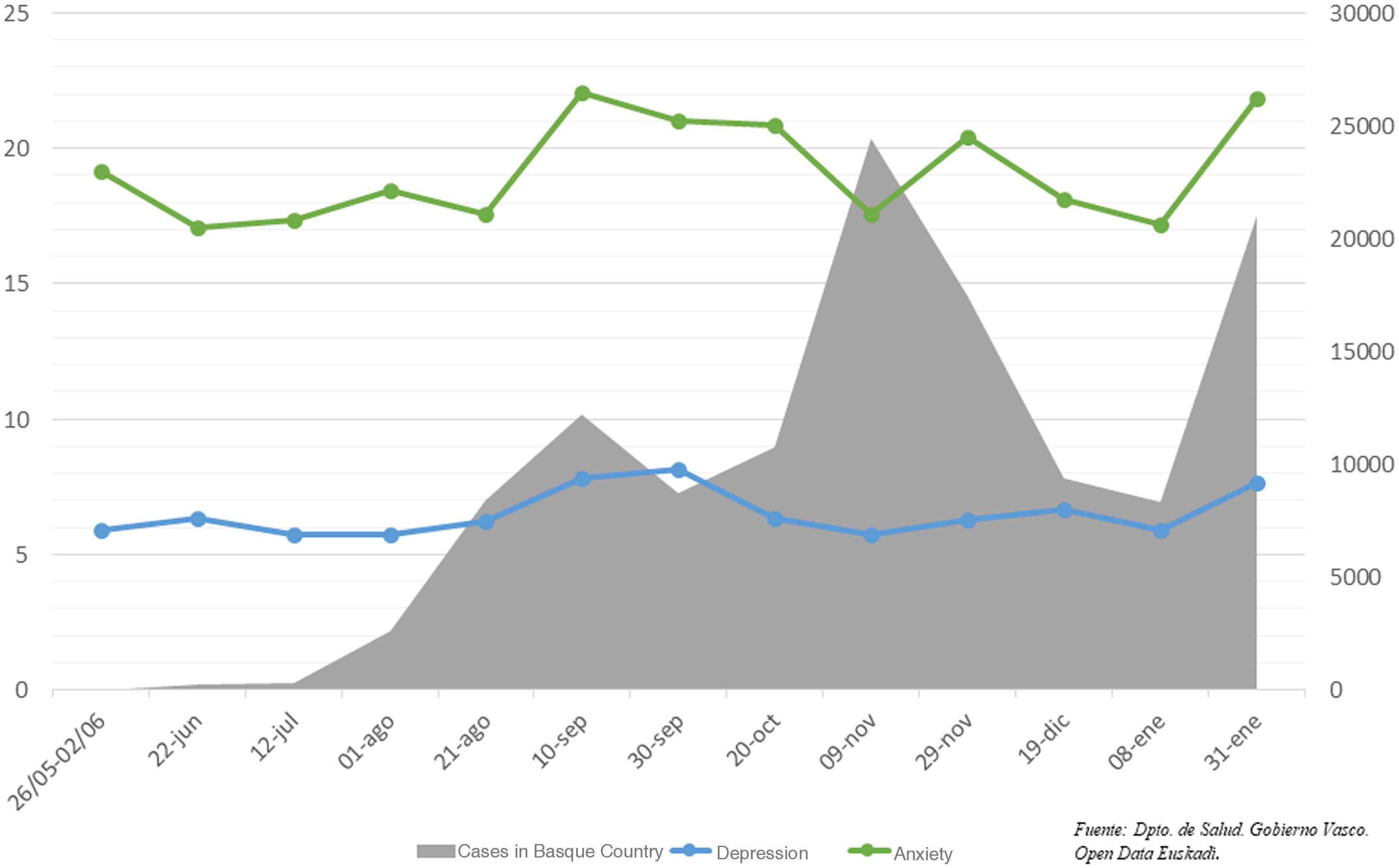
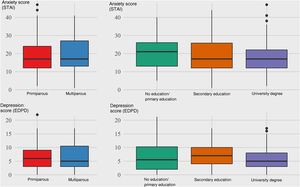
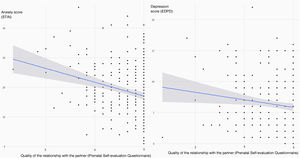
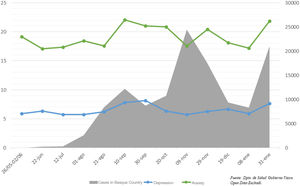
ResultsThe mean score was 18.75 points for anxiety (SD=8.69) and 6.45 points for depression (SD=4.32). Women expecting their second or later child had higher scores for depression (OR 2.51[95%IC: 1.26–5.01)) and anxiety (OR 1.98 [95%IC: 1.01–3.89]). Having completed university studies was associated with lower scores in depression (OR 0.28 [95%IC: 0.11−0.77]) and in anxiety (OR 0,2 [95%IC: 0.08−0.54]). A good relationship with the partner was associated with lower levels of anxiety (OR 0.45 [95%IC: 0.24−0.81]). The mean anxiety and depression scores are related to the incidence of COVID-19 cases; the anxiety score was significantly higher in periods of higher incidence.
ConclusionsGreater emotional care for pregnant women with low educational level, multiparous and with weak support from their partner, would reduce anxiety and depression in pregnancy. Health emergency situations affect mental health during gestation.
Evaluar la asociación entre edad, paridad, nacionalidad, estudios, empleo y apoyo de la pareja con la depresión y ansiedad durante el embarazo. Determinar el impacto de la evolución de la pandemia COVID-19 en los niveles de ansiedad y depresión de las participantes.
MétodoEstudio descriptivo correlacional transversal realizado en el Osakidetza/Servicio Vasco de Salud, Atención primaria, Bizkaia (España). Participaron 295 gestantes entre 8 y 41 semanas. Se midió la asociación entre edad, paridad, nacionalidad, nivel de estudios, empleo, apoyo de la pareja y tasas de incidencia de COVID-19 durante el periodo del estudio y las puntuaciones de depresión (medido con la Escala de Depresión Postnatal de Edimburgo) y de ansiedad (medido con la subescala de ansiedad Estado-Rasgo del State-Anxiety Inventory/STAI-S) durante el embarazo. Se construyó un modelo de regresión logística y se estimaron los odds ratios y sus intervalos de confianza de 95%.
ResultadosLa puntuación media en ansiedad fue de 18,75 puntos (DE=8,69) y en depresión 6,45 puntos (DE=4,32). Las mujeres que esperaban su segundo hijo o más obtuvieron puntuaciones más altas en depresión (OR 2,51[IC95%:1,26−5,01]) y ansiedad (OR 1,98[IC95%:1,01–3,89]). Haber cursado estudios universitarios se asocia con puntuaciones más bajas en depresión (OR 0,28 [IC95%:0,11−0,77]) y ansiedad (OR 0,2 [IC95%:0,08−0,54]). Una buena calidad en la relación de pareja se asocia con menores niveles de ansiedad (OR 0,45 [IC95%:0,24−0,81). La puntuación media en ansiedad y depresión se relacionan con la incidencia de casos COVID-19; la puntuación en ansiedad fue significativamente más alta en los periodos de mayor incidencia.
ConclusionesMayor atención emocional a las gestantes con bajo nivel de estudios, multíparas y con un débil apoyo de su pareja, permitiría reducir la ansiedad y depresión en el embarazo. Situaciones de emergencia sanitaria afectan a la salud mental durante la gestación.
What do we know?
Anxiety and depression are the most prevalent psychological disorders during pregnancy which are underestimated and underdiagnosed, with consequent significant repercussions for maternal-foetal health.
What does it contribute?
Multiparity, weak partner support, and low educational attainment are associated with higher scores for anxiety and depression during pregnancy. The anxiety score was significantly higher during periods of higher incidence of COVID-19.
In our shared social and cultural consciousness, motherhood continues to be associated with a gratifying state "of grace", a sublime and highly romanticised achievement, despite the fact that in 1985, psychiatrist Gisela B. Oppenheim questioned this premise for the first time, demonstrating the presence of anxious and depressive symptoms in 30% of pregnant women.1 Currently, it is estimated that 17–18% of women suffer from depression during pregnancy and about 8% have generalised anxiety disorder.2,3 Some come to pregnancy with previous mental illness, and others experience mental health issues for the first time at this stage.
Unfortunately, pregnancy does not prevent mental health problems: quite the opposite -pregnancy is a stage that predisposes women to depression.4 The physical and emotional changes inherent to motherhood involve adjustments in the personal, domestic, social and work spheres that can affect the quality of life of pregnant women, making them more susceptible to suffering from a mental disorder.5 The conflict of interest between personal needs, aspirations, expectations and the obligation to take on board new responsibilities determines the fact that pregnancy is a stage with a greater propensity to presenting psychological stress/discomfort.3
Prenatal symptoms of anxiety and depression can lead to changes in pregnant women's physical activity, diet, and sleep; changes that affect foetal development. Anxiety and depression increase the risk of miscarriage, preterm birth, low birth weight, and a lower Apgar score.6 We also know that children of mothers who experienced a lot of stress during pregnancy are more likely to have cognitive and behavioural problems6,7 and are at higher risk of mental health problems later in life. Prenatal anxiety and depression are also associated with changes in brain structure and function in infants and children.6,8 Also, suffering from anxiety or depression during pregnancy increases the chances of suffering from postnatal depression.2
Despite all these repercussions on maternal-foetal health, anxiety and depression are underestimated and underdiagnosed events. Family physicians tend to view perinatal depression as more of a psychosocial phenomenon than a biomedical one, leading to underdiagnosis and avoidance of treatment. Doctors observe a variety of problems that lead to distress and sadness by ing them calmly, with a "watch and wait" approach and doubt that these problems will be solved with pharmacological treatment; This strategy is considered inappropriate in the perinatal period.2 The Spanish Clinical Practice Guidelines for Pregnancy Care9 do not make any reference to the psychological needs of pregnant women but rather only mention the detection of mental disorders during the first few weeks postpartum (puerperium), completely forgetting about mental health during pregnancy. However, ensuring the emotional well-being of pregnant women should be part of prenatal care.10,11
In our health system, the midwife is the professional who maintains the closest contact with pregnant women, since she is in charge of monitoring most of the prenatal visits in low-risk pregnancies and the one who leads the maternal education sessions,9 however she does not have a pregnancy care guide that provides resources to identify pregnant women at greater risk of suffering emotional distress,9 as is covered in the guides in neighbouring countries.10 The use of extensive questionnaires to detect mental health problems is not feasible in a routine primary care pregnancy visit due to the time and resource constraints of these outpatient visits; however, knowledge of the factors that protect against or exacerbate mental health problems in pregnant women12 would enable initial screening and early care for the most vulnerable women. The main objective of the study was, therefore, to assess the association between certain variables and depression and anxiety in pregnant women in Bizkaia between May 2020 and January 2021. A secondary aim was to determine the impact of the evolution of the COVID-19 pandemic on the levels of anxiety and depression in these pregnant women.
MethodDesign and selection of participantsThe data from this study forms part of a larger research project that analysed the perceptions and needs of women during pregnancy, childbirth and postpartum, and the resources available to them to adapt to the new situation, the protocol for which has been published previously.13
This was a cross-sectional correlational descriptive study run in Osakidetza, at the Basque Health Service in the province of Bizkaia. Bizkaia is one of the three provinces that make up the autonomous community of the Basque Country (Spain) with a population of 1,141,407 inhabitants,14 7,720 births in 2020 and 6,957 in 2021.15 Osakidetza is the public health service in Bizkaia that has five integrated healthcare organisations, with a reference hospital in each of them and a total of 79 primary care centres of which 64 have a midwifery surgery/service.
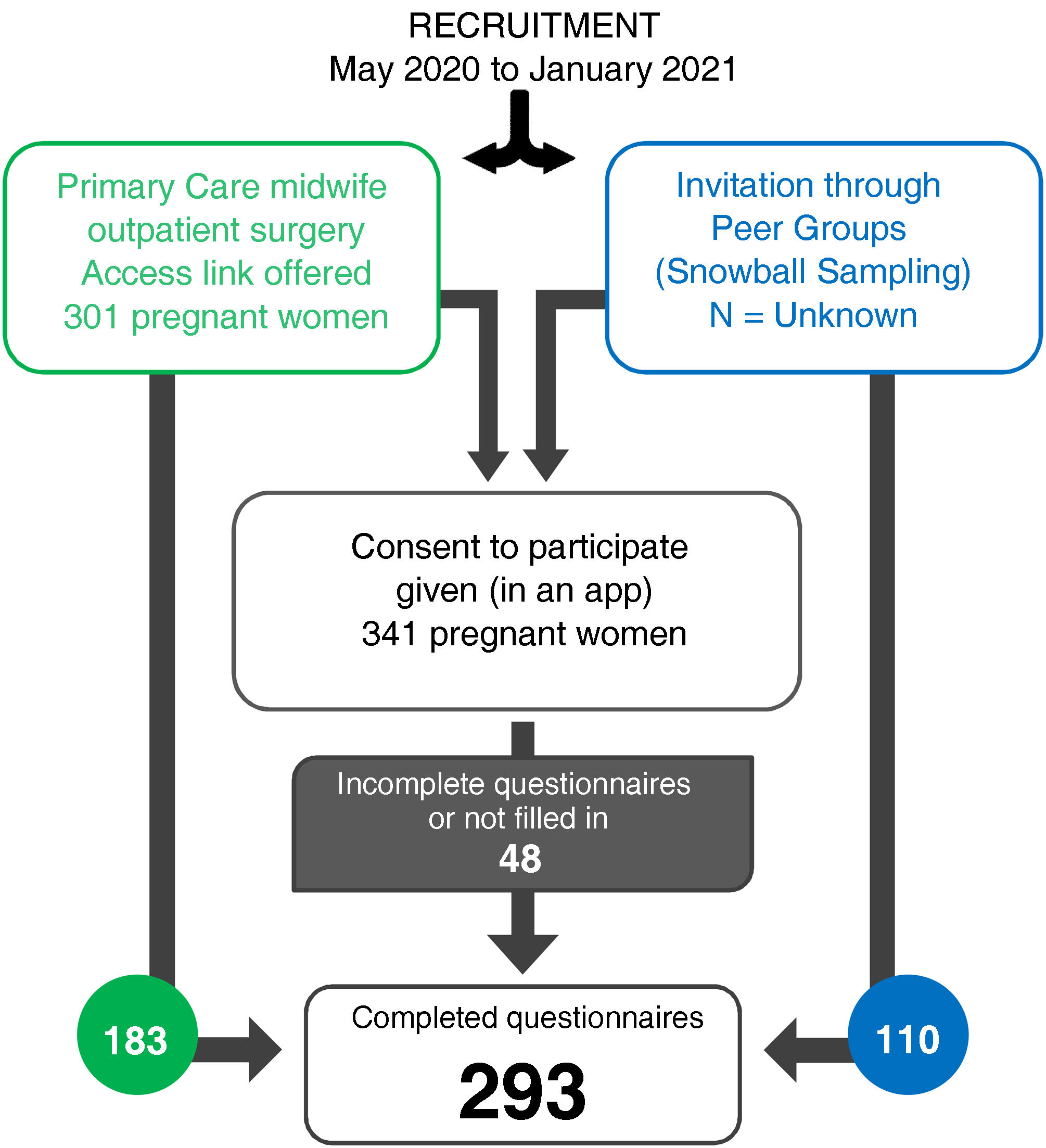
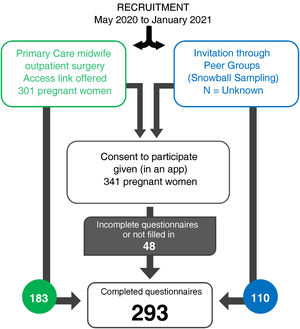
Recruitment of the participants was undertaken consecutively and non-randomly between May 2020 and January 2021 by the midwives at the outpatient surgeries for low-risk pregnancy monitoring in primary care. Recruitment was supplemented with snowball sampling, making it easier for pregnant women to share the link to access the questionnaire with other pregnant women until the necessary sample was completed.
All pregnant women from the eighth week of pregnancy, between 18 and 45 years of age, with current non-pathological pregnancies, who had sufficient command of the Spanish language to be able to understand and answer the questions presented, were invited to participate in the study. All pregnant women who did not meet these requirements were excluded.
Given that the information to be collected required a certain atmosphere of privacy, an online questionnaire was considered the best option for data collection, as it was possible to complete it at any time and any location. The questionnaire was chosen to be hosted by the encuestafacil.com platform as this offered data protection security in accordance with European regulations. Thus, all the women who agreed to participate in the study were offered an access link that enabled them to identify themselves using their medical I.D. number, obtain access to information about the study, respond to the request for informed consent and, after acceptance, access the questionnaire. Data was transferred to an Excel format (Microsoft 365 MSO, Impressa Systems, Santa Rosa, California. USA) and was subsequently anonymised by the person responsible before proceeding with database cleaning and analysis.
The process of recruiting the participants was continuously monitored, as well as the quality of the collection, organisation, management and analysis of the data by those responsible for this task within the research team and also expert staff at the Biocruces Bizkaia Research Institute.
Calculation of the sample sizeAssuming a weak effect of the sample size (OR=1.5), accepting an alpha risk of 0.05 and a power of 0.80, it was estimated that at least 242 women needed to participate. Given the type of questionnaire to be run, where the answer to all questions was mandatory, a follow-up loss rate of 0% was estimated.
Measuring instrumentsTo measure anxiety, the Spanish adaptation of the state-trait anxiety subscale in the State-Anxiety Inventory (STAI) was adopted.16 The use of this scale was considered because it showed a good fit to the one-dimensional model as well as very high reliability (χ2 = 696.3; p<0.001; χ2/gl=4.5; Comparative Fit Index [CFI]=0.97; Tucker-Lewis Index [TLI]=0.97; Root Mean Square Error of Approximation [RMSEA] [90% CI]=0.10 [0.10−0.12], Standardised Root Mean-Square [SRMR]=0.10, ordinal=0.93 α). This was a self-report composed of 20 items with a four-point Likert response system according to intensity (0=hardly ever/not at all; 1=a bit/sometimes; 2=quite a lot/often; 3=a lot/almost always). The total score ranged from 0 to 60 points, with a higher score corresponding to a higher degree of anxiety. In terms of clinical significance, the STAI-State scale (STAI-S) does not have a clinical criterion in its Spanish version; Therefore, our study followed the initial recommendation to use the 75th percentile17 as a cut-off point to consider anxiety clinically relevant, as other authors have opted for.18
Depression during pregnancy was measured using the Edinburgh Postnatal Depression Scale (EPDS), whose cut-off points have been validated for pregnant Spanish women.19 The self-administered scale consisted of 10 items on the presence of various depressive symptoms in the last seven days, with four response categories according to the increase in the severity of the symptoms described. Its internal structure showed an excellent fit to the one-dimensional model (χ2 = 80.9; p<0.001; χ2/gl=2.44; IFC=0.99; TLI=0.98; RMSEA [90% CI]=0.07 [0.05−0.09], SRMR=0.09) and adequate internal consistency (αordinal=0.83). The cut-off point was a score of 10 points to discriminate for the presence of depressive symptoms.20
In addition to describing the levels of anxiety and depression, the possible influence of some variables that could be associated with emotional states during pregnancy was also considered, such as: parity (first pregnancy/previous births),21 nationality (Spanish/non-Spanish), level of education completed (primary education/secondary education/university degree), paid work (yes/no) and partner support.12 The variables of age, parity, nationality, level of education and employment were collected through questions integrated within the online questionnaire.
The quality of the relationship with the partner was measured using a six-item scale (χ2=8.23, gl=9, p=0.512 2χ/gl=0.91, CFI=0.99, TLI=0.99, RMSEA [90% CI]=0.01 [0.00−0.06], SRMR=0.02), whose internal consistency (α ordinal=0.93; α ω=0.90), association (rs=0.81) and rate of agreement in the classification with the gold standard were excellent (K=0.66). The six questions refer to understanding, support, cooperation, communication and interest in the needs of pregnant women, taken from the Prenatal Self Evaluation Questionnaire (Lederman, 1996), validated for the Spanish population.22 The six questions were answered on a Likert scale from less (1) to greatest agreement (5). The cut-off point in the Prenatal Self Evaluation Questionnaire for acceptance was 17.
The data on the epidemiological situation of COVID-19 in the Basque Country was taken from Open Data Euskadi, a platform set up by the Basque government that promotes openness of government data in open formats and, within an exhaustive catalogue of data, contains data corresponding to the evolution of COVID-19 since the beginning of the pandemic.23 For the study, the data that was gathered was on the incidence of COVID-19 cases during the period from May 2020 and January 2021.
Statistical analysisTo study the relationship between variables, the mean and the standard deviation (SD) were calculated in each questionnaire to describe the continuous variables, and the absolute and relative frequencies in the case of categorical variables. A bivariate analysis of the relationship between possible sociodemographic predictors and depression and anxiety was run on the cut-off points set. A logistic regression model was constructed with all the variables to be studied for each outcome variable, also estimating the ORs and their 95% CIs. The maximum likelihood ratio was used (significance criterion p<0.05) and a backward elimination strategy was followed to construct the final model. Analyses were run using SAS version 9.4 (Cary, North Carolina, USA).
Given the period over which the study was conducted, an analysis of the possible influence of the COVID-19 pandemic could not be ignored. As the study was correlational and it was not possible to analyse cause and effect, we have described the evolution of anxiety and depression levels throughout the pandemic period and the possible correlations of the results with the periods of highest incidence of COVID-19 cases.
Ethical aspectsThe study was accepted by the Ethics Committee of the Basque Country (PI2019110). All participants received information about the study and agreed to participate. When the participants accessed the online questionnaire, they received information about the characteristics of the study, the possibility of dropping out without any consequences and a request for informed consent that, only once accepted, gave access to the questionnaire.
ResultsA total of 293 pregnant women between eight and 41 weeks’ pregnant responded to the anxiety and depression questionnaires (mean=28.87; SD=7.34), as described in Fig. 1. A similar number of pregnant women at less than 28 weeks and those between 28 and 37 weeks were recruited, in addition to also recruiting a smaller number of full-term cases (Table 1).
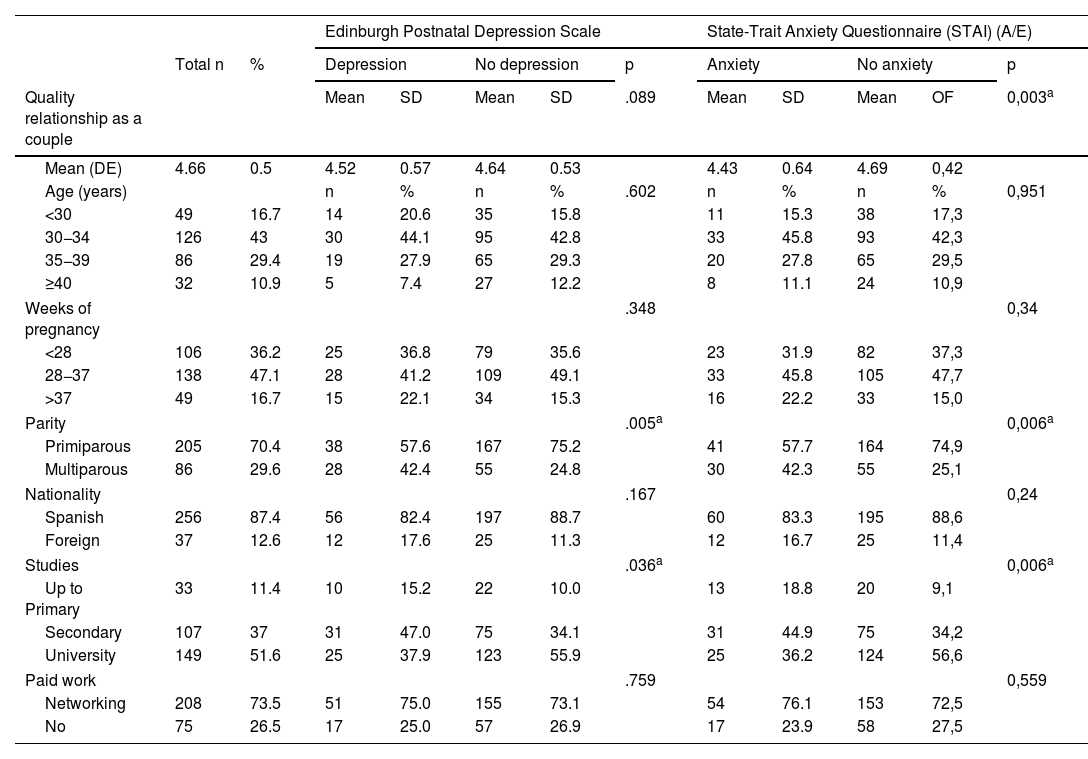
Descriptive characteristics of the sample and bivariate analyses of the relationship between anxiety and depression during pregnancy and sociodemographic variables (age, nationality, level of education, paid work); parity and quality of the relationship with the partner.
| Edinburgh Postnatal Depression Scale | State-Trait Anxiety Questionnaire (STAI) (A/E) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total n | % | Depression | No depression | p | Anxiety | No anxiety | p | |||||
| Quality relationship as a couple | Mean | SD | Mean | SD | .089 | Mean | SD | Mean | OF | 0,003a | ||
| Mean (DE) | 4.66 | 0.5 | 4.52 | 0.57 | 4.64 | 0.53 | 4.43 | 0.64 | 4.69 | 0,42 | ||
| Age (years) | n | % | n | % | .602 | n | % | n | % | 0,951 | ||
| <30 | 49 | 16.7 | 14 | 20.6 | 35 | 15.8 | 11 | 15.3 | 38 | 17,3 | ||
| 30−34 | 126 | 43 | 30 | 44.1 | 95 | 42.8 | 33 | 45.8 | 93 | 42,3 | ||
| 35−39 | 86 | 29.4 | 19 | 27.9 | 65 | 29.3 | 20 | 27.8 | 65 | 29,5 | ||
| ≥40 | 32 | 10.9 | 5 | 7.4 | 27 | 12.2 | 8 | 11.1 | 24 | 10,9 | ||
| Weeks of pregnancy | .348 | 0,34 | ||||||||||
| <28 | 106 | 36.2 | 25 | 36.8 | 79 | 35.6 | 23 | 31.9 | 82 | 37,3 | ||
| 28−37 | 138 | 47.1 | 28 | 41.2 | 109 | 49.1 | 33 | 45.8 | 105 | 47,7 | ||
| >37 | 49 | 16.7 | 15 | 22.1 | 34 | 15.3 | 16 | 22.2 | 33 | 15,0 | ||
| Parity | .005a | 0,006a | ||||||||||
| Primiparous | 205 | 70.4 | 38 | 57.6 | 167 | 75.2 | 41 | 57.7 | 164 | 74,9 | ||
| Multiparous | 86 | 29.6 | 28 | 42.4 | 55 | 24.8 | 30 | 42.3 | 55 | 25,1 | ||
| Nationality | .167 | 0,24 | ||||||||||
| Spanish | 256 | 87.4 | 56 | 82.4 | 197 | 88.7 | 60 | 83.3 | 195 | 88,6 | ||
| Foreign | 37 | 12.6 | 12 | 17.6 | 25 | 11.3 | 12 | 16.7 | 25 | 11,4 | ||
| Studies | .036a | 0,006a | ||||||||||
| Up to Primary | 33 | 11.4 | 10 | 15.2 | 22 | 10.0 | 13 | 18.8 | 20 | 9,1 | ||
| Secondary | 107 | 37 | 31 | 47.0 | 75 | 34.1 | 31 | 44.9 | 75 | 34,2 | ||
| University | 149 | 51.6 | 25 | 37.9 | 123 | 55.9 | 25 | 36.2 | 124 | 56,6 | ||
| Paid work | .759 | 0,559 | ||||||||||
| Networking | 208 | 73.5 | 51 | 75.0 | 155 | 73.1 | 54 | 76.1 | 153 | 72,5 | ||
| No | 75 | 26.5 | 17 | 25.0 | 57 | 26.9 | 17 | 23.9 | 58 | 27,5 | ||
Analysis of variance; SD, Standard Deviation; Q: Probability.
The mean anxiety score was 18.75 points (SD: 8.69). Depressive symptoms (score ≥10) were identified in 23.6% of cases, with a mean depression score of 6.45 points (SD 4.32). In this sample, the 75th percentile on the STAI scale was set as a score of ≥ 24. Bivariate analyses of the relationship between anxiety and depression during pregnancy and sociodemographic variables (age, nationality, level of education, paid work, parity) and the quality of the relationship with their partner are shown in Table 1, while the multivariate analyses are shown in Table 2.
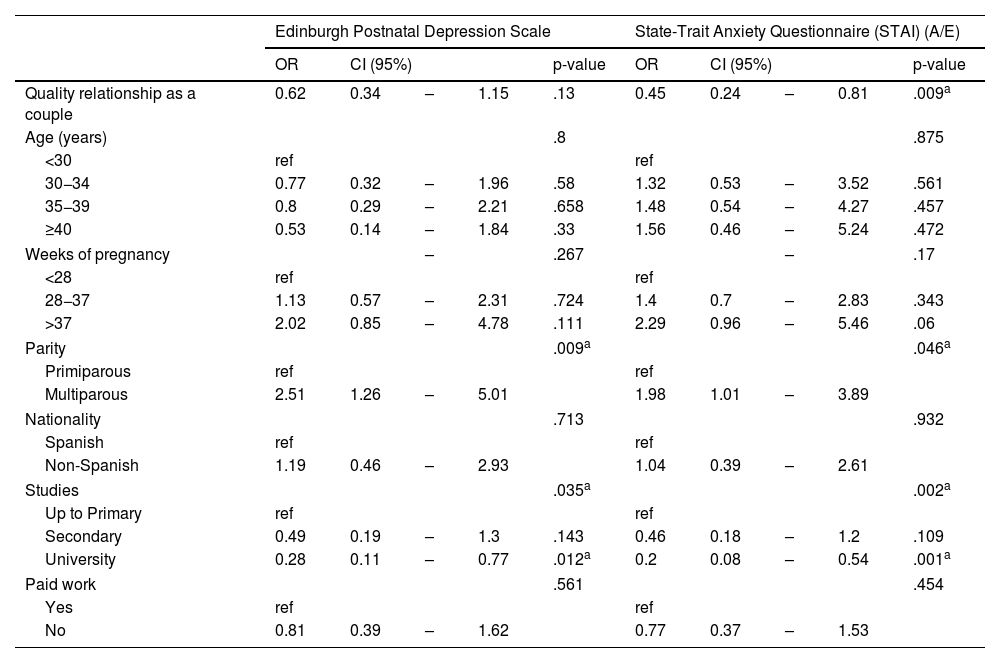
Multivariate analysis of the relationship between anxiety and depression during pregnancy and sociodemographic variables (age, nationality, level of education, paid work), parity and quality of the relationship with the partner.
| Edinburgh Postnatal Depression Scale | State-Trait Anxiety Questionnaire (STAI) (A/E) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | CI (95%) | p-value | OR | CI (95%) | p-value | |||||
| Quality relationship as a couple | 0.62 | 0.34 | – | 1.15 | .13 | 0.45 | 0.24 | – | 0.81 | .009a |
| Age (years) | .8 | .875 | ||||||||
| <30 | ref | ref | ||||||||
| 30−34 | 0.77 | 0.32 | – | 1.96 | .58 | 1.32 | 0.53 | – | 3.52 | .561 |
| 35−39 | 0.8 | 0.29 | – | 2.21 | .658 | 1.48 | 0.54 | – | 4.27 | .457 |
| ≥40 | 0.53 | 0.14 | – | 1.84 | .33 | 1.56 | 0.46 | – | 5.24 | .472 |
| Weeks of pregnancy | – | .267 | – | .17 | ||||||
| <28 | ref | ref | ||||||||
| 28−37 | 1.13 | 0.57 | – | 2.31 | .724 | 1.4 | 0.7 | – | 2.83 | .343 |
| >37 | 2.02 | 0.85 | – | 4.78 | .111 | 2.29 | 0.96 | – | 5.46 | .06 |
| Parity | .009a | .046a | ||||||||
| Primiparous | ref | ref | ||||||||
| Multiparous | 2.51 | 1.26 | – | 5.01 | 1.98 | 1.01 | – | 3.89 | ||
| Nationality | .713 | .932 | ||||||||
| Spanish | ref | ref | ||||||||
| Non-Spanish | 1.19 | 0.46 | – | 2.93 | 1.04 | 0.39 | – | 2.61 | ||
| Studies | .035a | .002a | ||||||||
| Up to Primary | ref | ref | ||||||||
| Secondary | 0.49 | 0.19 | – | 1.3 | .143 | 0.46 | 0.18 | – | 1.2 | .109 |
| University | 0.28 | 0.11 | – | 0.77 | .012a | 0.2 | 0.08 | – | 0.54 | .001a |
| Paid work | .561 | .454 | ||||||||
| Yes | ref | ref | ||||||||
| No | 0.81 | 0.39 | – | 1.62 | 0.77 | 0.37 | – | 1.53 | ||
Multivariate logistic regression: Backward Stepwise Regression.
OR: odds ratio; CI (95%): 95% confidence interval; Q: Probability.
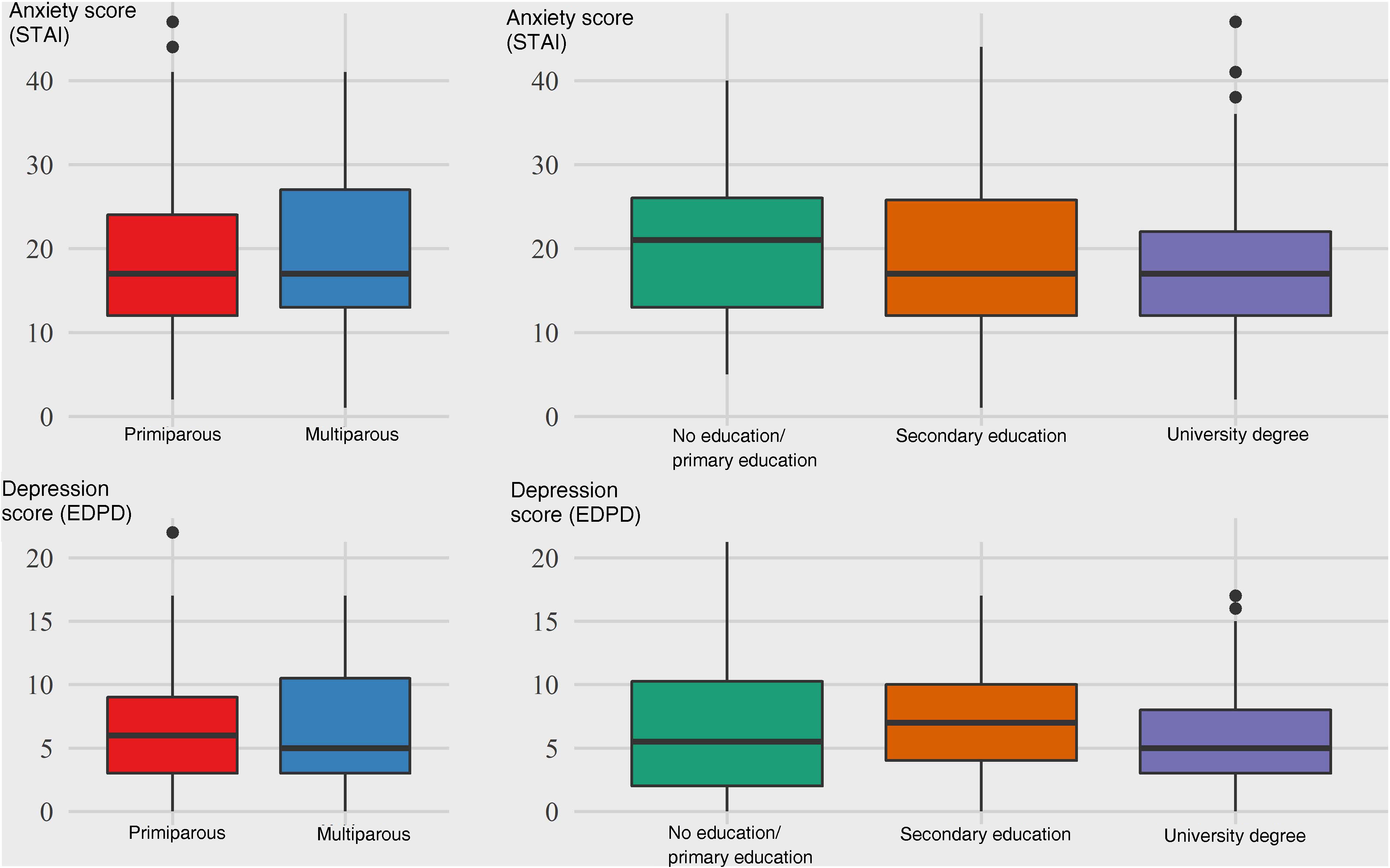
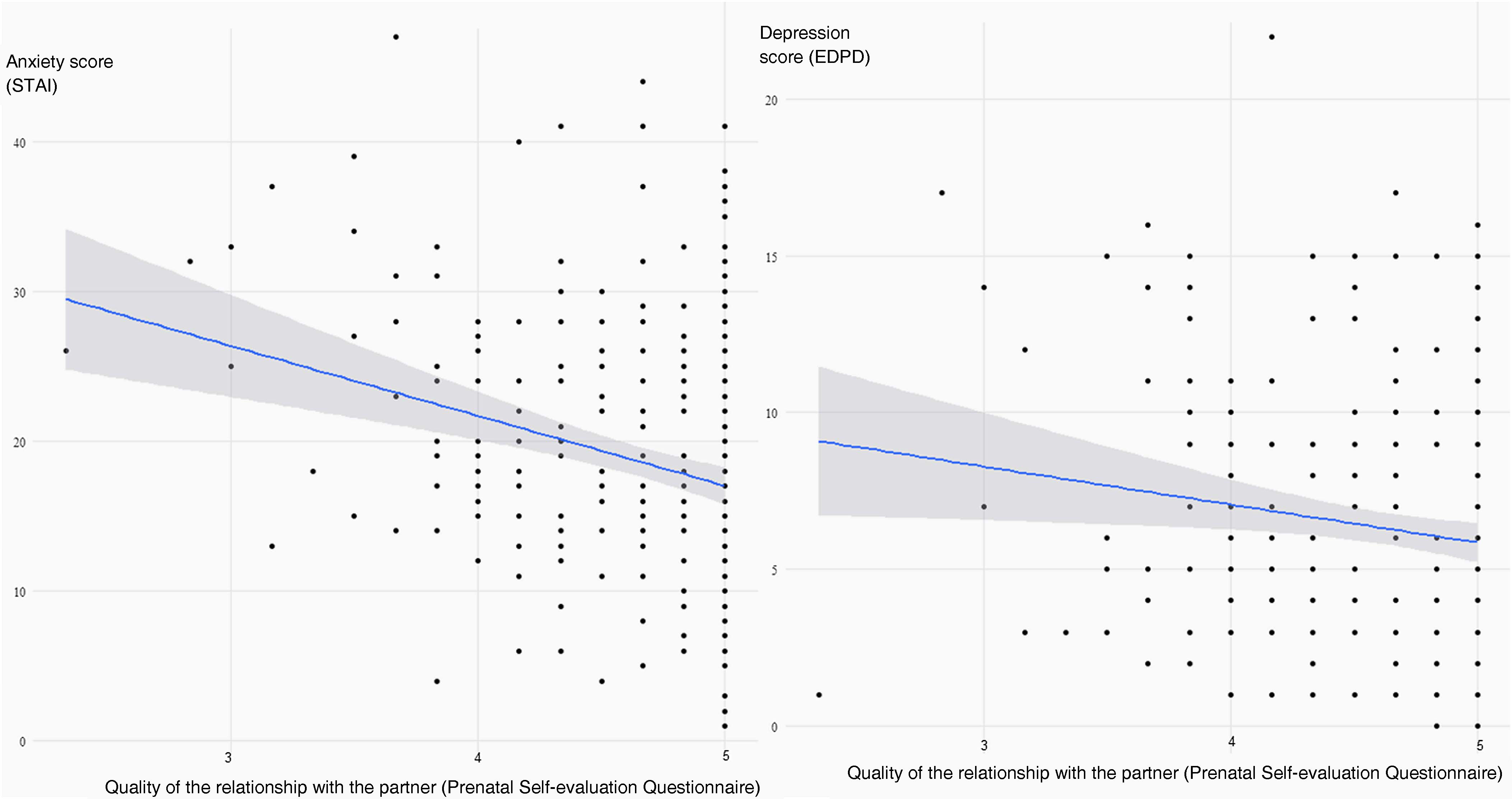
The final logistic regression model showed that women who were expecting their second child or more were more likely to have clinical symptoms of depression (OR 2.51; 95% CI: 1.26–5.01) and more likely to score higher on the anxiety scale (OR 1.98; 95% CI: 1.01–3.89) (Fig. 2). However, having completed a university degree was associated with a lower probability of depressive symptoms (OR 0.28; 95% CI: 0.11−0.77) or a score in the top quartile of the anxiety scale (OR 0.2; 95% CI: 0.08−0.54) (Fig. 2). The perception of greater quality in the relationship with the partner was also associated with lower levels of anxiety during pregnancy (OR 0.45; 95% CI: 0.24−0.81) (Fig. 3).
Anxiety and depression varied throughout pregnancy but there was no significant relationship between weeks of pregnancy and anxiety (p=.34) or between weeks of pregnancy and depression (p=.348), as shown in Table 1. In the case of anxiety, a progressive increase was observed as pregnancy progressed, this being 17.8 at the beginning of pregnancy, 18.49 between 27 and 36 weeks and reaching 22.3 at weeks 38–41 (F=2.115, gl [4.290], p=.079), however there were no differences that could be considered clinically significant.
The average score in anxiety and depression observed throughout the study period underwent variations that can be related to the periods of highest incidence of COVID-19 cases in the environment where the study was run. Thus, the mean anxiety score increased from 17.58 to 22.04 (p=.04) in the period from 21st August to 10th September, 2020; from 17.57 to 20.41 (p=.053) between 9th and 29th November 2020 and from 17.17–21.83 (p=.056) from 8th to 31st January 2021, reflecting the incidence of the disease in the Basque Country at these dates24 (Fig. 4).
DiscussionThe results of the study show that the anxiety and depression scores in the pregnant women taking part were similar to those of the general population16 and also similar to those reported by other studies.2,3 Knowing that pregnant women in our environment were no more anxious or depressed than non-pregnant women is comforting for healthcare professionals, a result that can be related to the quality of maternal and neonatal care in Spain, one of the countries with a high quality rating within the European region, even during the COVID-19 pandemic.24
Parity is associated with a higher degree of anxiety and depression. If being a mother is associated with greater emotional distress due to the increased responsibilities involved, it seems logical that the greater the number of children, the greater the stress.25 On the other hand, from a more realistic perspective, the fear of facing childbirth for women who have already had previous children, may be greater, especially for those who had traumatic experiences during previous births19 or bad experiences related to health care, the support received, or the restrictions imposed by protocols, etc.3
Women with a high level of education had a lower risk of high levels of anxiety and depression. These are people with a greater capacity to cope with the uncertainty and emotional stress that motherhood implies26 and a high level of education was considered one of the strongest predictors of mental health during pregnancy.27
Support and good communication with one's partner was related, as expected, to a lower level of anxiety.4,28 We know that social support is an important determinant of physical and psychological well-being, especially during pregnancy,4 however, the support from the partner does not always meet the expectations of the pregnant woman, and the lack of support and communication is a stressor.3 Perhaps the distress experienced by male partners during the perinatal period could affect their ability to provide support, so it would also be beneficial to take care of paternal perinatal mental health.3 In cases where the partner does not provide the expected support, social support from other pregnant women or new mothers appears to be useful as a source of reassurance and normalisation; helping pregnant women feel safe, more tolerant of uncertainty and less anxious.3
The increase in anxiety scores as the pregnancy progresses was an expected result since, as the birth approaches, the uncertainty about the ability to cope with the birth and adapt as mothers is greater.3,29 This means an increase in anxiety very close to statistical significance. Depression or pathological sadness can also increase, however most of the reasons related to depression remain throughout pregnancy, such as personality traits, personal and family history of depression, family or socio-occupational problems, etc.4 Nonetheless, it is necessary to consider some causes of depression that could worsen as the pregnancy progresses, such as the bad relationship with or lack of support from the partner4,28 or new reasons that may arise, such as the appearance of complications that put the health of the mother or her child at risk: preeclampsia, threat of preterm birth, intrauterine growth retardation, etc.3
The average anxiety score varied over the months studied, reflecting in some way the incidence of COVID-19 cases in our environment; since this score was significantly higher in periods of higher incidence of COVID-19 cases. Although the average anxiety score in the pregnant women taking part was not higher than in other populations or at other times, it cannot be said that the sample was insensitive to the exceptional health situation in which the study took place, since this posed a real threat to the mothers’ own health and that of the baby, together with poor prenatal care and social isolation.25 This result coincides with other studies that show a clear influence of the pandemic on anxiety in different populations.29
Given the potentially serious consequences of untreated anxiety and depression in pregnancy, it would appear vital to start by identifying those women at higher risk of suffering from these disorders in order to improve their emotional well-being6 with intervention strategies that reinforce social support and positive coping strategies.25 Psychological interventions such as cognitive behavioural therapy (CBT) and interpersonal therapy (IPT) offer benefits in reducing depression and increasing social support.6,30 One-on-one telephone counselling with midwives trained in psychotherapy has also been found to be an effective intervention.30 Digital health (e-health) interventions offer an opportunity that needs further study to achieve widespread dissemination31,32 but which must be considered in our current sociocultural context, as they offer hopeful results in reducing symptoms of anxiety and depression in pregnancy.33 In this direction, self-administered tools that enable the identification of warning signs in the mental health of pregnant women could lead to early care and reduce the impact of anxiety and depression.13
In any case, we must not forget that the relationship of trust with health professionals reduces the risk of ruling out new or considerable symptoms,2 which is why a quality interpersonal relationship between pregnant women and healthcare professionals is essential, where the midwife plays a fundamental role due to their closeness to women throughout the prenatal period. It is suggested that medical and mental health professionals work collaboratively to provide prenatal care when needed and be proactive in initiating treatment during pregnancy.2
Some limitations of the study should be noted. Having information on the participants' history of mental illnesses, factors associated with COVID-19 that could influence anxiety and depression, unknown at the time,34 and the participants in the maternal education sessions would have made it possible to analyse the participants’ possible relationship with levels of anxiety and depression, adding value to the study. Another limitation is that the sampling was not random and not all the women invited to participate in the study answered the questionnaire - and it may be that these women have specific personal characteristics. An attempt has been made to minimise this limitation by taking measures to ensure the representativeness of the sample, such as the diversification of recruitment centres and the consecutive selection of women to eliminate selection bias.
Greater attention to the mental health of pregnant women with a low level of education, multiparous and with weak support from their partner, together with screening of the emotional state of women during pregnancy34,35 would allow for individualised care that would improve the psychological well-being of pregnant women and reduce the risks that anxiety and depression can cause in maternal-foetal health. Faced with an uncertain future in which we cannot rule out new health emergency situations, the support of digital health (e-health) interventions may be promising for early detection and the reduction of emotional distress.36
FundingThe research project within which this study was run was funded by the Instituto de Salud Carlos III, file number PI20/00899, within the State Plan for R+D + i 2017–2020, co-financed by the ISCII- Subdirectorate General for Evaluation and Promotion of Research within the European Regional Development Fund (ERDF). The study also received funding from the Department of Health of the Basque Government, file number 2018111087.
Conflict of interestThe authors declare no conflict of interest.
We wish to acknowledge all the women who took part in the study for sharing their experiences at such an important and complex time in their lives as the COVID-19 pandemic in its early stages. We would also like to acknowledge the support of the Biocruces-Bizkaia Research Institute and all the midwives who enthusiastically collaborated in recruiting participants.
[El grupo ema.Q es un grupo multidisciplinar formado principalmente por matronas del Servicio Vasco de Salud, además de otros profesionales médicos, psicólogos, técnicos de calidad y expertos en investigación: Sonia Alvarez, Pilar Amorrortu, Mónica Blas, Inés Cabeza, Itziar Estalella, Ana Cristina Fernández, Gloria Gutiérrez de Terán-Moreno, Kata Legarra, Gorane Lozano, Amaia Maquibar, David Moreno-López, CNM. Mª Jesús Mulas, Covadonga Pérez, CNM. Angela Rodríguez, Mercedes Sáenz de Santamaría, Jesús Sánchez, CNM. Gema Villanueva].