A primary spontaneous pneumothorax (PSP) is due to the presence of air in the pleural space and is of unknown cause or aetiology. The main characteristic of this condition is its high tendency to re-occur. This study has two objectives: (1) to determine the efficacy of lung resection surgery using a videothorascope and talc pleurodesis and (2) to analyse the complications originating from the use of talc.
Material and methodsA review was carried out on a series of 130 PSP cases treated using videothorascopy, with or without parenchymal resection, and pleurodesis with 3g of asbestos-free talc (STERITAL®). Epidemiological data were collected, including the diagnostic method, surgical indication, mortality, general morbidity, and the specific morbidity due to talc pleurodesis, the number of recurrences, and their treatment.
ResultsThe patients had a mean age of 26.4 years, 84.3% were male, and 69% smoked. The surgical indication of the PSP was recurrence in 74.4% of cases. There was morbidity in 9 (7%) cases, with the most frequent complication being an air leak. No specific complication, such as empyema, pachypleuritis or adult respiratory distress syndrome (ARDS), on the use of talc was recorded. The mean follow-up was 10.1 months, during which there was recurrence in 4 (3%) cases.
ConclusionsPSP treatment by videothorascopic talc pleurodesis is highly effective, superior to other techniques used to produce pleurodesis, has a low general morbidity, no mortality, and no specific complications due to the talc.
Llamamos neumotórax espontáneo primario (NEP) a la presencia de aire en el espacio pleural sin causa o etiología conocida. La característica principal de esta enfermedad es su alta tendencia a la recidiva. Nuestro estudio tiene como objetivos: 1) conocer la eficacia del tratamiento quirúrgico mediante resección pulmonar por videotoracoscopia y pleurodesis con talco, 2) analizar las complicaciones derivadas del uso del talco.
Material y métodosSe revisa una serie de 130 casos de NEP tratados mediante videotoracoscopia con o sin resección parenquimatosa y pleurodesis con 3g de talco libre de asbesto (STERITAL®). Hemos recogido datos epidemiológicos, el método diagnóstico, la indicación quirúrgica, la mortalidad, la morbilidad general y la específica de la pleurodesis con talco, el número de recidivas y su tratamiento.
ResultadosNuestros pacientes tienen una edad media de 26,4 años, 84,3% son hombres y el 69% tiene hábito tabáquico. La indicación quirúrgica del NEP fue en el 74,4% por recidiva. Registramos una morbilidad del 7% que representan 9 casos, siendo la complicación más frecuente la fuga aérea. No registramos ninguna complicación específica por el uso del talco, tales como empiema, paquipleuritis o síndrome del distrés respiratorio del adulto (SDRA). Se realiza un seguimiento de 10,1 meses de media, constatándose 4 casos de recidiva que representan el 3%.
ConclusionesEl tratamiento del NEP mediante videotoracoscopia y pleurodesis con talco tiene una alta eficacia, superior a otras técnicas empleadas para producir pleurodesis, una baja morbilidad general, mortalidad nula, y no registramos ninguna complicación específica debida al talco.
Pneumothorax is defined as the presence of air in the pleural cavity. Primary spontaneous pneumothorax (PSP) occurs without apparent cause and with no history of lung disease. Its main feature is the high tendency to recur,1 which is 20%, 60% or 80% depending on whether it is the first, second or third episode.2
The goals of PSP surgical treatment are to remove the cause of the leak, if this is obvious, to obtain a complete re-expansion of the lung parenchyma and to produce an effective pleurodesis to minimise the chance of recurrence; with nil or very low morbidity or mortality.1
The supposed carcinogenic effect of talc is not proven, and may merely be theoretical speculation, probably having originated from the first reports of patients exposed to talc with impurities such as asbestos.
Some publications have reported threatening complications such as ARDS due to the use of talc,3 and late complications such as pulmonary restriction.4 However, no specific study of the use of talc in PSP reports such complications.
Objectives- (1)
To determine the effectiveness of surgical treatment for PSP using videothoracoscopic resection and talc pleurodesis.
- (2)
To analyse overall and specific complications associated with the use of talc.
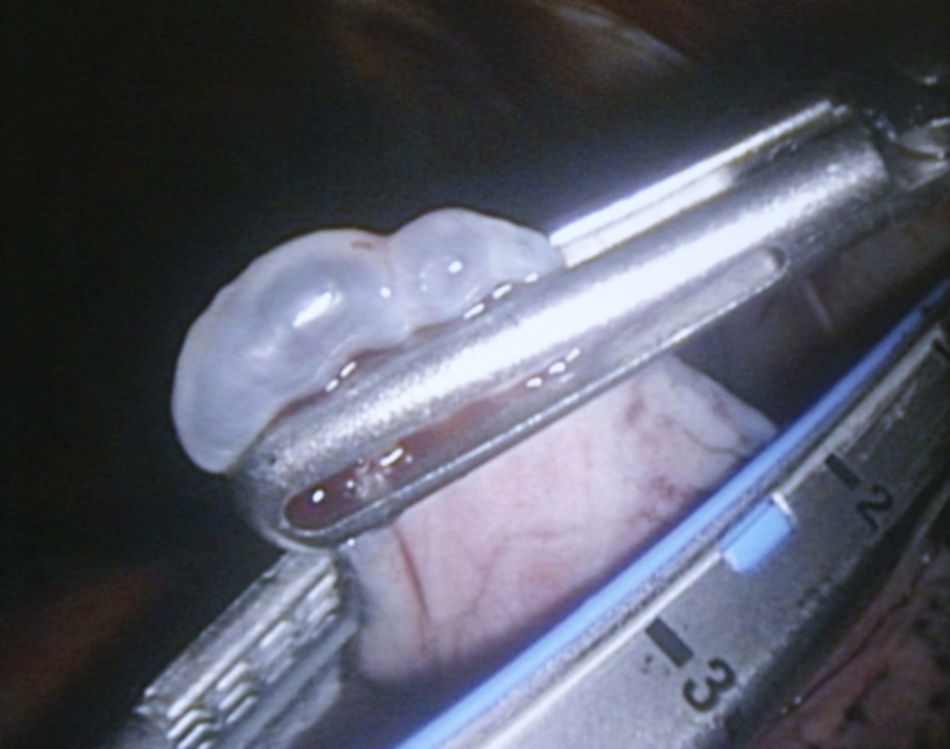
A retrospective descriptive study of 130 PSP cases between January 2001 and December 2009 was conducted on 121 patients treated by videothoracoscopy, with or without resection of parenchymal lesions and chemical pleurodesis with talc. All patients underwent videothoracoscopy via two or three ports. The endoscopic technique includes: (1) review of the pleural cavity, (2) release of any adhesions and (3) resection in the case of finding dystrophic bullae, blebs or apexes, via mechanical stapling ENDOGIA® type 45–3.5mm or 60–3.5mm (Fig. 1). After resection, lung expansion and the lack of air leaks were checked for. Once this was done, chemical pleurosclerosis was performed by applying a spray of 3g of sterile talc, average particle size 33.6μm, free of asbestos (STERITAL®). This was done by applying talcum powder to the visceral and parietal pleura, while trying not to apply it directly to the lung fissures or hilum (Fig. 2). In all cases, a 28 F Argyle drain was left by the anterobasal port, which was removed at 48–72h after verifying that there were no air leaks and a chest radiograph showed proper lung re-expansion. The following data were collected: age, sex, body mass index (BMI), smoking history, affected hemithorax, diagnostic method, pneumothorax type, radiological findings, surgical indication, type of surgery, endoscopic findings classified according to Vanderschueren staging, hospital stay, drain time, mortality, overall and specific talc pleurodesis morbidity, treatment of complications and number of recurs and their treatment. Computed tomography (CT) of the chest and pulmonary function tests (PFT) were performed at follow-up for patients who showed some respiratory symptoms or alterations in the simple chest radiography, which led to restrictive lung disease being suspected.
Statistical analysis was performed with the software G-STAT® 2.0.
ResultsThe average age of the patients was 26.4 years (SD 7.5 years), with 84.3% men, a mean BMI of 20 (3.3) and 70% smokers or ex-smokers. There were virtually no differences in the affected hemithorax, with 52% right and 48% left; 22.6% had non-simultaneous bilateral affectation. No simultaneous bilateral pneumothorax case was recorded.
Diagnosis of suspected PSP was confirmed by plain radiography in all cases. A chest CT was performed in 29 patients with suspected associated lung disease. The CT was reported as normal in 17 patients, 10 cases reported apical bullae, 1 case showed adhesions and bridles, while another had an associated pleural effusion which was a haemothorax.
The surgical indication for PSP was recurrence in 74.4%, persistent air leak in 17%, being bilateral in 7.7%, with 1 case of haemopneumothorax. As for the type of surgery, 76% was performed with resection and pleurodesis with the remaining 24% having only pleurodesis performed. One case was converted to open surgery due to failure of the mechanical staple.
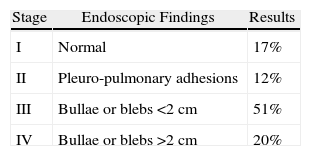
The endoscopic findings are described and classified according to Vanderschueren staging (Table 1).
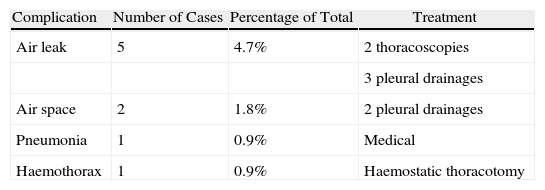
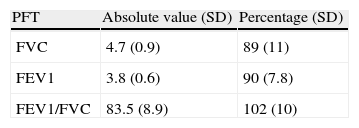
A morbidity of 7% (9 cases) was recorded, with the most common complication being air leakage, which occurred in 5 cases. There were 2 cases of residual air space, 1 case of pneumonia and 1 haemothorax case. Treatment of the complications was as follows: 3 cases of air leak and 2 cases of residual air space were treated with pleural drainage; the haemothorax required haemostatic thoracotomy; 2 cases of persistent air leak were reintervened by thoracoscopy, resection and application of a sealant (Pleura-seal®). The pneumonia case was resolved with medical treatment (Table 2). No complication due to the use of talc, e.g., empyema, pleural thickening or adult respiratory distress syndrome (ARDS) was found. The average drainage time was 2.3 days, with an average stay of 2.3 days after surgery. The outpatient follow-up was 10.1 months on average, and during this time 4 cases of recurrence were observed, representing 3% of our series. These recurrences occurred on average after 3.6 months (range from 0.6 to 6 months). Of these 4 cases, 2 were treated with pleural drainage and 2 required further thoracoscopic intervention. A chest CT scan was performed in 10 cases during follow-up and none of these gave suggestive signs of lung restriction. Also, PFT was performed in 9 cases (Table 3) on average 8.6 months after surgery (range 2–29 months), which presented normal values.
PSP is defined as the presence of air in the pleural space for no known reason, resulting in parenchymal collapse. It is the most common disease in the emergency room for our speciality, usually in young patients between 20 and 40 years of age. The estimated incidence in males is between 7.4 and 28 cases per 100000 inhabitants and year, and for women from 1.2 to 10 cases per 1000001; in our series, it was 8.1 per 100000 inhabitants. The most frequent complication of this disease is recurrence, being 20%, 60%, and 80% after the first, second and third episode, respectively.2
Endoscopic findings according to Vanderschueren staging coincide with those of other series, with the majority having stage III.5
The standard surgical treatment for PSP and its indications are well established,1 with thoracoscopy and pleurodesis currently considered to be an excellent technique,6,7 and it is the method of choice for most surgeons.7 However, the method used for pleurodesis is still under discussion. Using talc as a pleurodesis agent is effective, inexpensive and widely available; it has minimal associated side effects and is increasingly used.8
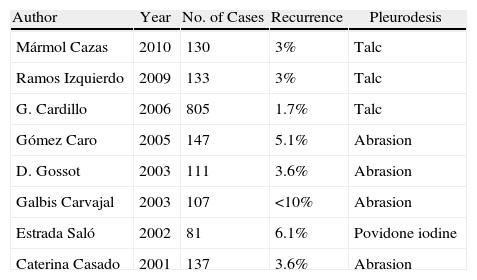
The results obtained using parenchymal resection and the use of talc as a sclerosing agent in the treatment of PSP are highly effective, and comparable with the series using talc pleurodesis,6,7,9–11 which gave results better than other pleurodesis methods2,5,12,13 (Table 4).
Percentage of Recurrence for PSP Surgical Treatment in the Different Published Series.
| Author | Year | No. of Cases | Recurrence | Pleurodesis |
| Mármol Cazas | 2010 | 130 | 3% | Talc |
| Ramos Izquierdo | 2009 | 133 | 3% | Talc |
| G. Cardillo | 2006 | 805 | 1.7% | Talc |
| Gómez Caro | 2005 | 147 | 5.1% | Abrasion |
| D. Gossot | 2003 | 111 | 3.6% | Abrasion |
| Galbis Carvajal | 2003 | 107 | <10% | Abrasion |
| Estrada Saló | 2002 | 81 | 6.1% | Povidone iodine |
| Caterina Casado | 2001 | 137 | 3.6% | Abrasion |
Source: Citations.2,5–7,13,22,23
After reviewing our series, no mortality and a low rate of general complications were found, which is in accordance with most of the reviewed studies6,7,14, with air leak being the most common complication, which resolved in most cases with pleural drainage maintenance.
Concerns about the carcinogenic effect of talc are likely to originate from reports of early patients exposed to talc impurities such as asbestos. In 1979, three United Kingdom centres collected data on patients who underwent talc pleurodesis at least 14 years beforehand. The authors concluded that there was no increased incidence of lung cancer or mesothelioma.9,15
No specific complication due to the use of talc, such as ARDS, empyema or signs of pulmonary restriction was found. We believe that the use of an appropriate dose of large particle size talc (2–4g), such as STERTALC®, produces effective pleurodesis with minimal complications, as was demonstrated in our study, the extensive study by Cardillo6 and other publications relating to PSP.7,10,14 Both American and European publications that use talc for producing pleurodesis in PSP report no cases of ARDS.3,6,10,16,17 Publications with cases of ARDS used talc in malignant pleural effusions, immunosuppressed patients or those with significant comorbidity, or used talc in higher doses than that for PSP or, in the US case, used small particle size talc. According to a study, the talc used in the US had a diameter between 7.8 and 13.5μm, while we used talc with an average of 33.6μm.18 Reported cases of ARDS are mostly from the United States. From the study by Rinaldo19 to current ones,3,16 all agree on the patient characteristics and the type and dose of talc used in cases of ARDS. There are European series with no complications, such as ARDS, due to the use of talc in both PSP and in malignant pleural effusions.6,17 We believe that this may be due to the dose and particle size of the powder used, and this also applies to patient comorbidity. It has also been demonstrated in experimental studies that phenomena such as ARDS and extrapleural talc deposition are dose-dependent, with the use of talc at low doses (3–4g) being very safe.20
We conducted a follow-up of 10.1 months on average, and found no signs or symptoms of pulmonary restriction in our patients. From a sample of 9 patients with clinically suggestive symptoms, lung functionality was normal, as found in the Cardillo study, which was prospective.21
There is some concern that patients treated with talc later have to undergo surgery. We did not have the potential surgical incidence of lung disease for this type of patients, and in any case we believe it is minimal, since by definition they are patients with no history of lung disease. If they did have to be intervened later, we believe it would be technically possible, as the parietal pleura exists and it would be no more complicated than operating on a patient with a history of lung infections, such as tuberculosis, which until recently was an endemic disease in this country, and currently many thoracic surgery patients have a history of pulmonary tuberculosis.
In conclusion, PSP treatment via videothoracoscopic resection and large particle size talc pleurodesis is highly efficient, with low overall morbidity, no mortality in our series and with no specific complications recorded due to the use of talc.
Conflicts of InterestThe authors have no conflicts of interest to declare.
Please cite this article: Mármol Cazas EE, et al. Eficacia y morbimortalidad del tratamiento quirúrgico mediante videotoracoscopia y pleurodesis con talco del neumotórax espontáneo primario. Cir Esp. 2011;89:463–7.