The prevalence of diabetes mellitus (DM) has increased in low- and middle-income countries and in marginal areas of developed countries. In Spain, it grew by 3.42% from 1993 to 2020. In the Canary Islands, the increase was even greater.
ObjectivesThe main one was to evaluate the possible relationship of the income level with DM, different markers of metabolic control and the use of Primary Care services, in Las Palmas de Gran Canaria (LPGC). Secondary ones are to determine the prevalence of DM in the city of LPGC, to describe the sociodemographic characteristics, the use of Primary Care services of the population with DM, the level of registry of variables related to metabolic control and the main process indicators and intermediate results of the metabolic control in the population with DM in the city of LPGC.
Material and methodAll patients with DM over 14 years of age, living in LPGC as of 12/31/22 were included. Data were collected from the electronic medical records of the Canarian Primary Care Service, the National Institute of Statistics and the National Tax Agency.
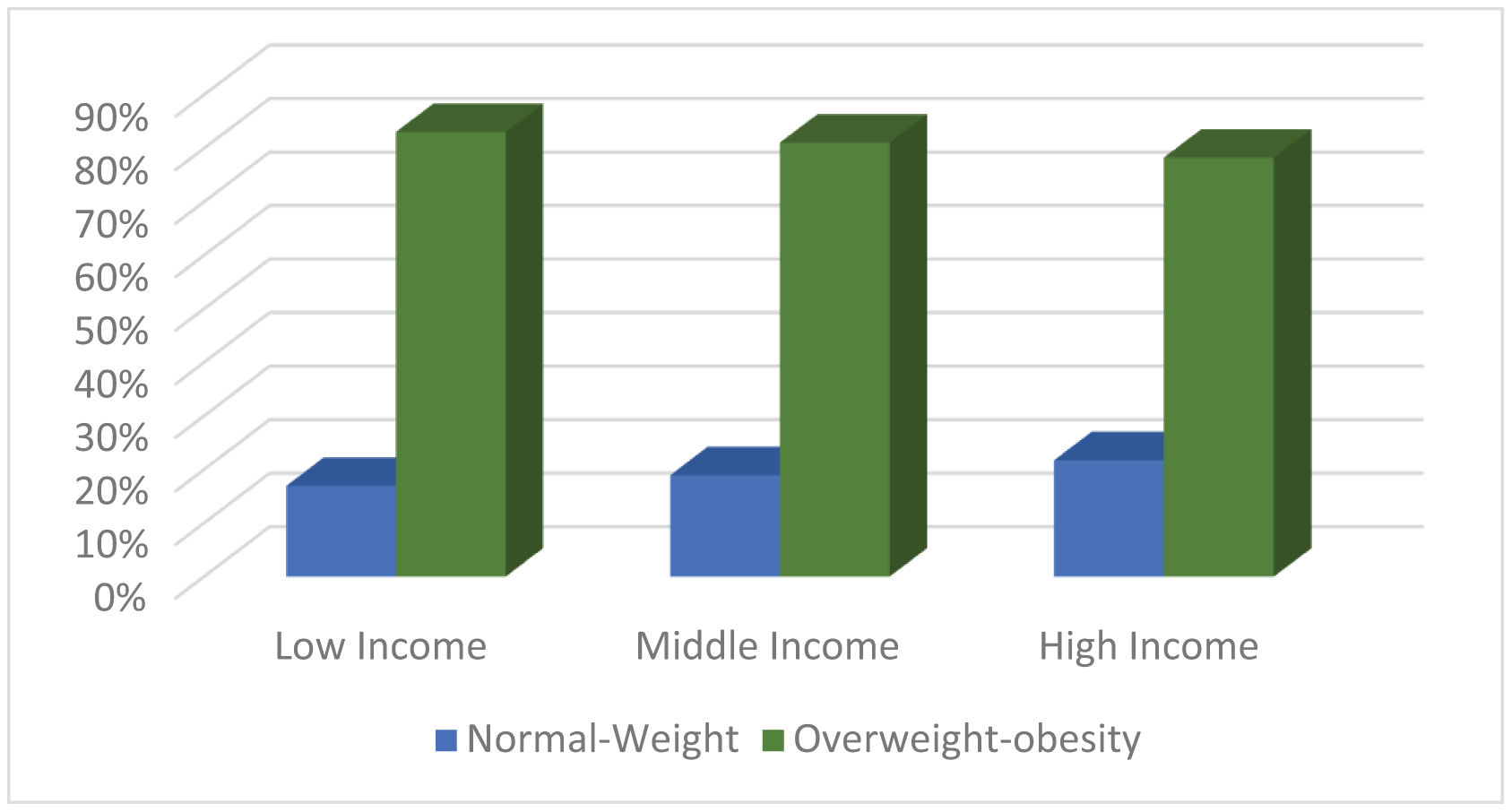
Results and conclusionThe overall prevalence of DM was 11.39%. The mean age of participants was 67.06 years (SD=13.86), lower in men than in women. The groups with low or moderate income accounted for more than 40% of the prevalence each, while those with high income barely accounted for 10%. Higher income levels corresponded to lower use of health resources and registration of metabolic variables, while decreasing income levels were associated to higher prevalence of overweight/obesity, worse lipid and glycemic profiles and higher risk of diabetic foot. The middle-income group showed the highest prevalence of pathological/uncertain diabetic retinopathy, lower glomerular filtration and higher LDL levels.
La prevalencia de diabetes mellitus (DM) ha aumentado en países de ingresos bajos y medios y en zonas marginales de países desarrollados. En España creció un 3,42% de 1993 a 2020. En Canarias el aumento fue aún mayor.
ObjetivosEl principal es evaluar la posible relación del nivel de ingresos con la DM, diferentes marcadores de control metabólico y el uso de los servicios de Atención Primaria, en Las Palmas de Gran Canaria (LPGC). Los secundarios son determinar la prevalencia de DM en la ciudad de LPGC, describir las características sociodemográficas, la utilización de los servicios de Atención Primaria de la población con DM, el nivel de registro de variables relacionadas con el control metabólico y los principales indicadores de proceso y resultados intermedios del control metabólico en la población con DM de dicha ciudad.
Material y métodosSe incluyeron todos los pacientes con DM mayores de 14 años, residentes en LPGC el 31/12/22. Los datos se recogieron de la historia clínica electrónica del Servicio Canario de Atención Primaria, del Instituto Nacional de Estadística y de la Agencia Tributaria Nacional.
Resultados y conclusiónLa prevalencia global de DM fue del 11,39%. La edad media de los participantes fue 67,06 años (DE=13,86), menor en hombres que en mujeres. Los grupos de ingresos bajos o moderados representaron más del 40% de la prevalencia cada uno, mientras que los de ingresos altos apenas representaron el 10%. Los mayores niveles de ingresos correspondieron a un menor uso de recursos sanitarios y de registro de variables metabólicas, mientras que los menores niveles de ingresos se asociaron con una mayor prevalencia de sobrepeso u obesidad, peores perfiles lipídicos y glucémicos y mayor riesgo de pie diabético. El grupo de ingresos medios mostró la mayor prevalencia de retinopatía diabética patológica o incierta, menor filtración glomerular y niveles más altos de LDL.
Diabetes mellitus (DM) is a chronic disease characterized by certain metabolic disorders due to alterations in the secretion and action of insulin.1 The prevalence of DM worldwide has tripled since 1980, due to the increase in sedentary lifestyle, overweight and obesity, which are still very present today.2 According to the International Diabetes Federation (IDF), 151million adults were living with DM in 2000, the estimated amount was three-fold higher (463million people) in 2019 and 700million people with DM are expected by 2045 worldwide.2–4
In Spain, the prevalence of DM raised from 4.09% in 1993 to 7.51% in 2020, and reached a maximum of 7.8% in 2017. At present, older people show the highest prevalence rates. Although the prevalence used to be higher in women in former times, the highest prevalence in 2020 corresponded to men (8.52% in men vs. 7.11% in women).1,5 In the Canary Islands, the prevalence grew markedly in recent years, up to the maximum declared prevalence in Spain, with 3.19 points above the national average.5,6 In this regard, the average rate of obesity and overweight (one of the main modifiable risk factors for DM) in the Canary Islands is higher than the national one, with a joint prevalence of obesity and DM of 25–30% in the island of Gran Canaria.1,5
Regarding main complications, the Canary Islands show the highest incidences in Spain of DM-related major amputations (0.81/100,000 people), with an upward tendency, in contrast to the negative trend of the national mean.7
The concept of health integrates many determinants, like social factors. One of the social factors behind regional differences in the prevalence of DM and its consequences is the income level. There is a strong line of research that supports the relationship between the socioeconomic status and lifestyle, diet, health care and control of the disease in people with DM. Financial inequity not only affects life expectancy, but also raises by two the probability of developing DM.2,4–6,8
Besides showing the highest DM prevalence, the southern regions of Spain also have the lowest incomes. The mean annual per-capita net income in the Canary Islands was €9487 in 2019, namely €2193 lower than the Spanish national mean. In addition, 32.1% of the population in the Canary Islands is at risk of poverty, as compared to 21.5% in the whole country.5 The prevalence of DM in Las Palmas de Gran Canaria (LPGC), located on the Grand Canary Island, was 11.41% in 2019 namely, higher than the mean of the island (10.89%) and Spain (7.8% >18 years).9,10 Furthermore, there are large economic differences between different districts of the city.
ObjectivesMain objectiveTo investigate the possible relationship of the income level with DM, as well as with other markers of metabolic control and use of health services by the population with DM in the city of LPGC.
Secondary objectives- 1.
To determine the prevalence of DM in the city of LPGC.
- 2.
To describe the sociodemographic characteristics of the population with DM in the city of LPGC.
- 3.
To describe the use of Primary Care services by the population with DM in the city of LPGC.
- 4.
To describe the level of registry of variables related to metabolic control corresponding to the population with DM in the city of LPGC
- 5.
To describe the main process indicators and intermediate results of the metabolic control in the population with DM in the city of LPGC.
Cross-sectional descriptive study analyzing the data of all patients alive to 31/12/2022 who met the following inclusion criteria:
- -
Older than 14 years.
- -
Diagnosed with DM regardless of type.
- -
Resident in LPGC.
The studied period was from January 1st, 2022 to December 31st, 2022. Data on the use of Primary Care services corresponded to the whole year 2022. Data related to recorded process indicators and intermediate metabolic control results, as well as indicator values also corresponded to the whole year 2022, except for patients with incomplete data, whose last measurement was used, regardless of the moment it was made.
Data were collected from the following sources:
- -
Clinical information and data on the use of primary care health services of people assigned to the public health service were collected from the Electronic Medical Record of Primary Care of the Canary Islands Health Service (DRAGO-AP).
- -
Municipal gross and net incomes classified by LPGC postal codes were collected from the Personal Income Tax declarations of largest municipalities in 2020, published on the website of the Spanish tax agency, Agencia Estatal de Administración Tributaria (AEAT).9
- -
The number of people living in the municipality of LPGC, total and classified by sex, was collected from the Spanish institute of statistics, Instituto Nacional de Estadística (INE), to calculate the prevalence of DM in the whole population and by sex.
Variables were grouped as follows:
- a)
Demographic variables
- -
Age: quantitative variable categorized in subgroups according to the threshold established in the agreed management program “Programa de Gestión Convenida 2020”.11 (≤70/>70).
- -
Sex (male/female).
- -
Postal code of the residence (35001–35019).
- b)
Variables related to the use of primary care services in a health center, at home, by telephone, online, or in the emergency room:
- -
Number of visits to the doctor in 2022 grouped into 3 categories: 1–4 visits, 5–8 visits or more than 8 visits.
- -
Number of visits to the nurse in 2022 grouped into 3 categories: 1–4 visits, 5–8 visits or more than 8 visits.
- c)
Variables related to metabolic control and DM care process:
- -
Last recorded values of glycosylated hemoglobin (HbA1C).
- -
Last recorded values of high-density lipoprotein cholesterol (HDL).
- -
Last recorded values of low-density lipoprotein cholesterol (LDL).
- -
Last recorded values of triglyceride (TGL).
- -
Last recorded values of glomerular filtration (estimated with the MDRD-4 IDMS formula) (GF).
- -
Last recorded albumin/creatinine ratio.
- -
Last recorded body mass index (BMI).
- -
Examination of feet, with patients classified into: low, moderate or high risk in accordance with the action guidelines for diabetic foot of the Canary Islands (Guía de Actuación. Pie diabético en Canarias).12
- -
Examination for diabetic retinopathy, with patients classified into: normal or pathological/uncertain diabetic retinopathy.
- -
Additionally, the registration dates of data corresponding to each variable in the healthcare process were recorded.
- d)
Economic variables:
Patients’ individual mean gross income in 2020 classified by postal code and grouped into 3 categories: low income (≤ €22.292), middle income (€22.292–€35.666) and high income (≥ €35.666).
Categories low, middle and high income were based on the Organisation for Economic Co-operation and Development (OECD) classification, which is centered on the median income, considering income levels below 75% of the median as low income, those in the range 75–200% of the median as middle income, and those above 200% of the median as high income. The OECD splits middle income into two subgroups, lower-middle income between 75 and 125% of the median and upper-middle income between 125 and 200% of the median.14 The 2020 median income in the Canary Islands was € 17.833.13 In this study, middle-low (75–125% of the median) and low (<75% of the median) incomes were included into the low-income group, those between 125 and 200% of the median were in the middle-income group and those over 200% were in the high-income group.
In the descriptive analysis of results, categorical variables were expressed as frequencies and percentages and quantitative variables as measures of centralization (mean) and dispersion (standard deviation). In the bivariate analysis, the χ2 test was used for qualitative variables and the Student's t test for quantitative ones. The level of statistical significance was established in 5% (p<0.05), equivalent to a 95% confidence interval (95%CI). Data were analyzed with the Statistical Package for the Social Sciences (SPSS), v 28 software.
ResultsPrevalenceThe total prevalence of DM in people over 14 years of age in LPGC was 11.39% (38,422/337,410); in women, the prevalence was 11.24% (19,815/176,287), while in men it was 11.55% (18,607/161,123); in people over 70 years of age was 3469% (16,968/48,918), while in people ≤70 years of age was 7,44% (21,454/288,492).15
Sociodemographic characteristics:The sample was composed of 48.4% men (n=18,607). The total mean age was 67.06 years (SD=13.86); the mean age of women was 67.71 years (SD=14.59) while that of men was 66.36 years (SD=12.99). The majority of subjects were of middle income (47.78%), followed by low (40.49%) and high (11.73%) income; with higher incomes corresponded to older individuals (Table 1).
Distribution of the sample according to income level.
| Income level | Mean age (years) | Statistical significance | ≤70 years | >70 years | Total | Total | |||
|---|---|---|---|---|---|---|---|---|---|
| Women | Men | Women | Men | Women | Men | Women+men | |||
| Low | 66.74 (SD=13.61) | <0.001 | 4375 | 4533 | 3900 | 2750 | 8275 | 7283 | 15,558 (40.49%) |
| Moderate | 67.08 (SD=13.93) | 4867 | 5327 | 4393 | 3771 | 9260 | 9098 | 18,358 (47.78%) | |
| High | 68.10 (SD=14.34) | 1115 | 1237 | 1165 | 989 | 2280 | 2226 | 4506 (11.73%) | |
| Total (%) | 67.06 (SD=13.86) | 10,357 | 11,097 | 9458 | 7510 | 19,815 | 18,607 | 38,422 | |
| 21,454 (55.84%) | 16,968 (44.16%) | (51.57%) | (48.43%) | ||||||
The DM population living in LPGC included in the study made a total of 347,263 visits to the family doctor (61.52%) and 217,204 visits to the nurse (38,48%) in 2022, which corresponded to a mean of 9.04 visits to the doctor (SD=6.66) and 5.65 to the nurse (SD=10.43) per person. Both the mean number of visits to the doctor and to the nurse significantly decreased with increasing income levels (Table 2).
Mean number of visits to the doctor and the nurse in different income levels.
| Low income | Moderate income | High income | Statistical significance | |
|---|---|---|---|---|
| Visits to the doctor95%CI | 9.16 (9.05–9.26) | 9.02 (8.92–9.12) | 8.71 (8.51–8.91) | <0.001 |
| Visits to the nurse95%CI | 6.06 (5.88–6.23) | 5.50 (5.35–5.66) | 4.88 (4.66–5.11) | <0.001 |
In general, all variables showed a significant decreasing trend with increasing incomes. Variables less frequently registered were BMI, diabetic retinopathy and diabetic foot (Fig. 1).
DM care process indicators and intermediate metabolic control resultsTable 3 shows the values of care process-related variables, classified by income level at any moment or in the whole year 2022.
Mean values of care process-indicators and intermediate metabolic control results of DM patients classified by income level.
| Test | Low income | Middle income | High income | Statistical sig | ||||
|---|---|---|---|---|---|---|---|---|
| At any time | 2022 | At any time | 2022 | At any time | 2022 | At any time | 2022 | |
| HbA1C195%CI | 7.14 (7.11–7.16) | 7.14 (7.11–7.17) | 7.13 (7.11–7.15) | 7.11 (7.08–7.14) | 6.99 (6.95–7.03) | 7.01 (6.96–7.06) | <0.05 | <0.05 |
| BMI295%CI | 30.37 (30.26–30.47) | 30.01 (29.82–30.20) | 29.94 (29.84–30.04) | 29.78 (29.58–29.98) | 29.36 (29.17–29.56) | 29.47 (28.96–29.97) | <0.05 | 0.06 |
| HDL395%CI | 49.40 (49.16–49.63) | 49.61 (49.32–49.89) | 50.07 (49.85–50.29) | 50.30 (50.04–50.57) | 50.56 (50.04–51.08) | 50.72 (50.03–51.41) | <0.05 | <0.05 |
| LDL495%CI | 95.66 (95.04–96.28) | 93.24 (92.48–94.01) | 97.03 (96.47–97.59) | 95.03 (94.33–95.74) | 96.12 (94.97–97.28 | 93.52 (92.69–95.69) | <0.05 | <0.05 |
| TGL595%CI | 155.93 (154.41–157.45) | 153.32 (151.64–154.99) | 150.53 (149.21–151.86) | 148.12 (146.60–149.64) | 146.20 (143.57–148.83) | 143.65 (140.77–146.52) | <0.05 | <0.05 |
| GF695%CI | 79.58 (79.19–79.96) | 80.24 (79.65–80.83) | 78.75 (78.39–79.10) | 79.07 (78.51–79.63) | 78.60 (77.87–79.34) | 79.17 (77.99–80.34) | <0.05 | <0.05 |
| Microalbumin795%CI | 24.66 (23.70–25.63) | 22.57 (21.45–23.69) | 24.55 (23.66–25.43) | 22.73 (21.71–23.75) | 23.94 (22.13–25.74) | 22.49 (20.21–24.77) | 0.79 | 0.97 |
| Diabetic foota | 331/5979 (5.54%) | 203/3580 (5.67%) | 331/6289 (5.26%) | 178/3480 (5.11%) | 55/1122 (4.90%) | 27/671 (4.02%) | <0.05 | <0.05 |
| Diabetic retinopathya | 3373/11,335 (29.76%) | 889/4003 (22.21%) | 4474/11,739 (38.11%) | 945/3088 (30.60%) | 955/2728 (35.01%) | 163/605 (26.94%) | <0.05 | <0.05 |
1. Cut point 1–20. 2. Cut point 5–80. 3. Cut point 0–300.
4. Cut point 0–500. 5. Cut point 0–1200. 6. Cut point 0–200.
7. Cut point 0–500.
With increasing income, HbA1C, BMI and TGL decreased, while HDL increased. Furthermore, the prevalence of high risk of diabetic foot was higher for low incomes. However, the prevalence of pathological/uncertain diabetic retinopathy was highest for middle incomes, as well as LDL values, while GF was lower for high incomes. Furthermore, values corresponding to 2022 were significantly better for all variables than values regardless of the date, except for the high risk of diabetic foot in people with low incomes and BMI and HbA1C in people with high incomes.
Last measured BMI (regardless of the date) classified into underweight, normal-weight or overweight/obesity, according to the level of income, showed that BMI increased with decreasing income, since the low-income group showed the highest overweight/obesity and lowest normal-weight prevalence (Fig. 2).
DiscussionDM is suitable to assess health-related inequalities, due to its demonstrated higher prevalence in the most socially disadvantaged groups in developed countries. In the Netherlands, people with low socioeconomic status at the beginning of their lives were found to have a higher probability of suffering pre-DM or DM.16 In Portugal an association was found between DM and lower schooling, unemployment and lower income.17 In Tehran, DM prevalence was significantly lower in people with more wealth, better education and living in richer areas.18 Similar results were found in a study conducted in Saudi Arabia.19 Conversely, a study carried out in China reported higher probability of suffering from DM in people with higher family wealth, although people with DM with higher family wealth and education level were more likely to adhere to prescribed medications and to take measures to control their disease.20 Similarly, a study from South Africa showed that self-reported DM and total DM (undiagnosed DM+diagnosed DM) were significantly concentrated in the wealthy population, although non-self-reported or underdiagnosed DM was higher among the poorest ones.21 There are some similar studies carried out in Spain in the same time period (2022). In this case, one from Andalusia shows that the average age of people with DM is even higher than in the present study (71 years). They made 20 doctor visits per year, assuming a direct cost of approximately 5000euros, highlighting the great economic burden of DM.22
Our results may be greatly influenced by the fact that the Canary Islands have a lower mean income than the country as a whole. Moreover, the population with higher education is also smaller (27.9% vs. 30.6%). Consequently, there is a higher percentage of people at risk of poverty (32.1% vs. 21.5% of the national mean).
In this context, it is important to highlight that the choice of the median income used to establish the different income-groups raised doubts since, on the one hand, the Canarian median income was rather lower than the national one (17.833 vs. 21.067) and, on the other hand, the municipality of LPGC was like an “oasis” in the Canary Islands with a median income (20.933) higher than the regional (17.833) or the provincial (18.154) one, and similar to the national one. However, because of the large heterogeneity within LPGC with high income variability in different postal code districts, using the national median left only one high-income district in the city, thus reducing statistical power. Therefore, the Canarian median was used with the aim of ensuring representativity of all the three income-groups.
Moreover, we decided to melt the OECD low-income and low-middle income groups into one low-income group in this study because, since we used district means and not real income values, there was no low-income district left when any of the median values were used (either the median of Spain, the Canary Islands, the province of Las Palmas or LPGC).13 Thus, using the median of the Canary Islands and melting the OECD low and medium-low income groups, representativity was granted also for the lowest stratum, with 29% tax declarants in 2020 in the low-income, 50% in the middle-income and 21% in the high-income level.13
Previous studies conducted in our region, the Canary Islands reported DM prevalence of 13.2% in municipalities such as Telde, 13.6% in all the islands23,24 or 10.7% in the whole autonomous region of the Canary Islands.1,5 A study reported 11.41% DM prevalence in LPGC in 2019 namely, higher than the mean of the island of Gran Canaria (10.89%) and the whole Spain (7.8%>18 years).9 In agreement with these findings, the overall DM prevalence in LPGC in our study was 11.39%.
Previous studies also showed that DM prevalence was always higher in men. In the municipality of Telde, 15.8% in men versus 10.6% in women were reported, while other studies described 12% in men versus 10% in women.23,25 This trend was also observed in our study, although the differences were smaller with 11.6% in men versus 11.2% in women. On the other hand, the 2020 European Health Survey showed a gradient in the prevalence of self-reported DM in Spain according to social class, with higher prevalence observed in social class IV followed by class V (low income groups).26
Finally, as described in the Canary Islands Health Survey (ESC) published in 2021 by the Canary Islands Institute of Statistics, the lower social classes required more assistance at public health centers. This result is in line with our study, in which higher incomes corresponded to lower numbers of visits to doctors and nurses. In addition, in the Canary Islands, 13% of people belonging to class I have private insurance, compared to 1% of those in class VI, which could also explain the results. This is related to the fact that in our study as income increases, the level of registration decreases. Despite this, it is contrary to what other studies in our country show, which state that they make more visits to nursing than to medicine. This is probably related to the fact that these are multi-pathological patients who go to the doctor for another pathology.27,28
In our study, the low levels of records regarding diabetic foot and Diabetic Rethinopathy are of special interest. This has different explanations: on the one hand, there are deficiencies in the nursing staff when performing the technique. Likewise, there are different exclusion criteria for not performing DR on some specific patients, such as being in home care. Finally, as these are techniques that require more time, the fact of the pandemic has also influenced this, since the nursing staff in 2022 played a very important role in COVID vaccination.
Studies indicate that lower socioeconomic status is associated with an increased risk of complications such as diabetic ketoacidosis in people with type 1 DM.29 Furthermore, available evidence clearly indicates that there are socioeconomic inequalities in DM care. The most disadvantaged socioeconomic levels are associated with worse process indicators and worse intermediate outcomes, which result in higher risks of micro and macrovascular complications also in type 2 DM.30 It has also been found that DM patients with higher socioeconomic status show better controlled glycemia in HbA1c tests,31 in agreement with our results.
Regarding one of our outcome variables, the risk of diabetic foot, the literature evidences that the Canary Islands show the highest incidence of DM-related major amputations in Spain, with studies describing rates of 1.34–1.94/1000 in the whole island of Gran Canaria5 or 320/100,000 in the south of the island of Gran Canaria.32 In our study, the global prevalence of high risk of diabetic foot was 5.28% (408/7731) in 2022.
The Spanish mean rate of Diabetic Retinopathy was 15.28% with 1.92% at high risk of suffering from it soon7; on the island of Gran Canaria, it was around 20%.5 In the present study, 25.95% of the sample presented pathological/uncertain diabetic retinopathy in 2022.
Furthermore, as described in the Canary Islands Health Survey (ESC) published in 2021 by the Canary Islands Institute of Statistics, people belonging to classes V and VI (low income groups) are those with the highest percentages of obesity and overweight (they have worse eating habits and do less physical exercise). This coincides with what was observed in our sample of patients with diabetes.27
LimitationsThe existing limitations are related to the type of study, an ecological study.
On the one hand, there is an aggregation bias, in this case as far as the income variable is concerned and, since the data have been extracted from the Statistics of Personal Income Tax Filers of the largest municipalities by postal code of LPGC of 202022 (CP: 35001–35019), this could grant a level of income that does not correspond to each individual, despite living in a certain neighborhood; with the consequent information bias when using a classification by postal code of the response variable that may be imprecise. This is explained by the AEAT simply taking an average of the income of the taxpayers from a given postal code, regardless of the possible dispersion that may exist within the same postal code.
Furthermore, due to the structure of the project itself, since it is an observational study, causality cannot be established, but only an association between known and observed factors, without ruling out that there are unknown or unobserved factors that explain the results obtained and are left out of our analysis such as lifestyle and management of their baseline disease, type of DM and years with the disease or concomitant acute or chronic pathologies that may indirectly influence the status and control of DM, its metabolic variables or the use of primary care resources, so inferences cannot be made about the causes of risk at the individual level.
On the other hand, when dealing with secondary sources of information, it always depends on the level of registration and this can be a great handicap when carrying out the study. There may be a registration deficit on the part of health professionals when including the information in the electronic medical record, or a registration deficit due to the fact that the patients themselves are the ones who do not attend a consultation when it is required or because they do it outside the registration systems, that is, going to private healthcare, so this information for the present study is not available with the consequences that this entails at an analytical level. Also important is the fact that there may be human errors when recording the information and this is palpable in the fact that when quantifying the values of the different metabolic control variables, significant errors have been seen and, for this reason, Therefore, cut-off points have been delimited in them to avoid taking very extreme and illogical values that have been found at the time of carrying out the study.
Conclusions- -
The overall prevalence of DM was 11.39%. Women was 11.24% and men was 11.59%. People over 70 years of age was 34.69% while people ≤70 years of age was 7.44%.
- -
The mean age of participants was 67.06 years (SD=13.86), lower in men than in women. The groups with low or moderate income accounted for more than 40% of the prevalence each, while those with high income barely accounted for 10%.
- -
As the income level increases, the use of health resources in patients with DM decreases.
- -
The record of variables related to DM decreases as the population's income level increases.
- -
As income decreases, the prevalence of overweight-obesity increases, they have a worse lipid and glycemic profile and have a greater risk of having diabetic foot. Middle incomes have higher prevalence of pathological/doubtful DR, lower GFR and higher LDL levels.
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.