Selective parathyroidectomy, the treatment of choice for primary hyperparathyroidism, requires precise preoperative localization. Our purpose was to compare the accuracy and concordance of pre-surgical MIBI parathyroid scintigraphy and ultrasonography, as well as to assess the relevance of hybrid acquisition (SPECT/CT) in compromised circumstances: low-weight or ectopic adenomas, coexisting thyroid disease and re-interventions.
MethodsThe study included 223 patients with primary hyperparathyroidism operated in a single Surgical Unit from August 2016 to March 2021. Preoperative ultrasonography and double-phase MIBI were performed with early SPECT/CT acquisition. A minimally invasive surgical approach was initially attempted, except in patients with concomitant thyroid surgery or multiglandular parathyroid disease.
ResultsSelective parathyroidectomy was accomplished in 179 patients (80.2%); cervicotomy and/or thoracoscopy in 44. Removal of the parathyroid lesion was achieved in 211 patients (94.6%), corresponding 204 (96.7%) to adenomas (37 ectopic). The cure rate was 94.2%. Preoperative MIBI SPECT/CT showed higher sensitivity and accuracy (84%; 80%) compared to ultrasound (72%; 71%), being more precise in defining the exact anatomical location (75.8% vs 68.7%). These differences reached statistical significance in ectopic glands. The existence of concomitant thyroid pathology did not decrease the sensitivity of SPECT/CT (84.2%). Mean parathyroid weight was 692.2mg (95%CI: 443.5-941) in MIBI-negative cases and 1145.9mg (95%CI: 983.6-1308.3) in MIBI-positive (p=0.001). Re-intervention was successful in the 8 patients with previous surgery.
ConclusionMIBI SPECT/CT presents greater sensitivity, accuracy and anatomical precision than ultrasound for preoperative parathyroid localization, even in the case of ectopic glands or coexisting thyroid pathology. The weight of the pathological gland is a significantly limiting factor.
La paratiroidectomía selectiva, tratamiento de elección del hiperparatiroidismo primario, requiere una precisa localización preoperatoria. Nuestro propósito fue comparar la exactitud y la concordancia de la gammagrafía-MIBI y la ecografía preoperatorias, así como evaluar la relevancia de la adquisición híbrida (SPECT/TC) en circunstancias comprometidas: adenomas de bajo peso o ectópicos, patología tiroidea coexistente, reintervenciones.
MétodoEl estudio incluyó 223 pacientes con hiperparatiroidismo primario operados en una única unidad quirúrgica (agosto de 2016 hasta marzo de 2021). Se realizó ecografía preoperatoria y MIBI en doble fase, con SPECT/TC precoz. Se intentó de inicio una cirugía mínimamente invasiva, excepto en pacientes con patología tiroidea concomitante o enfermedad paratiroidea multiglandular.
ResultadosSe realizó paratiroidectomía selectiva en 179 pacientes (80,2%) y cervicotomía y/o toracoscopia en 44. Se logró la extirpación paratiroidea en 211 pacientes (94,6%), correspondiendo 204 (96,7%) a adenomas (37 ectópicos). La tasa de curación fue del 94,2%. MIBI SPECT-TC mostró mayor sensibilidad y precisión (84%; 80%) respecto a la ecografía (72%; 71%), siendo más precisa en la ubicación anatómica exacta (75,8% frente a 68,7%). En glándulas ectópicas, esta diferencia fue significativa. La coexistencia de patología tiroidea no disminuyó la sensibilidad de SPECT/TC (84,2%). El peso medio de la glándula paratiroidea fue de 692,2mg (IC95%: 443.5-941) en los casos MIBI negativos y de 1.145,9mg (IC95%: 983.6-1308.3) en los MIBI positivos (p=0.001). La reintervención tuvo éxito en los 8 pacientes con cirugía previa.
ConclusiónLa MIBI SPECT/TC muestra mayor sensibilidad, exactitud y precisión anatómica que la ecografía para la localización paratiroidea preoperatoria, incluso en el caso de glándulas ectópicas o patología tiroidea coexistente. El peso de la glándula patológica es un factor significativamente limitante.
Primary hyperparathyroidism (pHPT) is a common endocrine disorder caused by a parathyroid adenoma in 80–85% of the cases and less frequently by multiglandular disease: double adenoma or hyperplasia (15–20%) and rarely by parathyroid carcinoma (1%).1
The diagnosis of pHPT is based on laboratory tests, and in most cases is detected in the pre-clinical stage. Surgery is the appropriate treatment in symptomatic patients2 and is also recommended in other circumstances,3 such as patients aged<50 years, with serum calcium level 1mg/dL above normal values, hypercalciuria (24-h urinary calcium level superior to 400mg/dL), renal lithiasis, osteoporosis or glomerular filtration<60mL/min.1
Evidence-based recommendations enhance optimal management in referral hospitals by skilled surgeons, as it is well demonstrated that volume of operations correlates inversely with complication rate and reoperations. Surgeons who perform more cases/year have better outcomes compared to lower-volume surgeons.2,4
In recent years, improved presurgical imaging has facilitated the development of a less extensive surgical approach compared to traditional bilateral cervical exploration, without a decrease in surgical efficacy.5 Thus, minimally invasive parathyroidectomy (MIP) has become the surgical procedure of choice in solitary adenomas, since it achieves high cure rates of up to 96.96–99.4%7 and involves a smaller cervical incision, shorter surgery duration, lower rates of postoperative complications,6 a shorter hospital stay and consequently financial advantages.7
As a result, bilateral cervicotomy is performed only in certain circumstances, such as multiglandular disease, the simultaneous indication of thyroidectomy, and exceptionally in some patients with previous cervical surgery or ectopic adenoma localization.2
In this regard, the role of pre-surgical localization techniques is of critical importance in enabling a successful MIP. Tc-99m MIBI Scintigraphy (MIBI) and cervical ultrasonography (US) are the imaging tests currently performed first for preoperative parathyroid localization8,9 as the most cost-effective strategy.2 MIBI presents a slightly higher sensitivity, specificity and accuracy compared to US,10 probably related to technical advances, such as hybrid Single Photon Emission Computed Tomography/Computed Tomography (SPECT/CT) acquisition.9,11,12 When MIBI and US are concordant, MIP presents very low recurrence rates.6
On the other hand, in cases of MIBI-US discordance or localization failure, second-line techniques are performed prior to surgery, such as 18F-choline, 11C-methionine or 11C-choline PET/CT, as well as morphological techniques (CT, MRI).9 PET tracers have demonstrated excellent sensitivity, relying on its optimal resolution, probably higher for Choline.13
Meanwhile, in patients with concomitant nodular thyroid, the acquisition of a Tc-99m Pertechnetate Thyroid Scintigraphy is helpful to distinguish parathyroid lesions from MIBI-positive thyroid nodes and avoid false positive results.14
The primary objective of this study was to determine the accuracy and concordance of MIBI SPECT/CT double-phase scintigraphy and cervical US for preoperative localization of parathyroid lesion in patients with pHPT treated in a single Endocrine Surgery Unit, checking its usefulness for a MIP approach.
The second objective was to analyse the factors that influence MIBI and US localization, considering the efficiency of both, particularly MIBI SPECT/CT, in adverse scenarios: low-weight parathyroid adenomas, coexisting thyroid nodular disease,15 previous cervical surgery16,17 or ectopic parathyroid localization,10,18 since in these compromised clinical circumstances, the accuracy of preoperative imaging and consequent surgical success are usually lower.
Material and methodsAn observational study was conducted, including all patients with biochemical pHPT and surgical criteria operated consecutively in a single Endocrine Surgery Unit at a tertiary teaching hospital (University Hospital of Navarra, Spain), from MIP implementation (August 2016) until March 2021. The minimum follow-up was therefore 6 months. The study was approved by the Institution's Ethics Committee.
Presurgical data were recorded for the following variables: gender, age, BMI (kg/m2), preoperative serum calcaemia (mg/dL), PTH (pg/mL) and 25-hydroxyvitamin D (ng/mL), BMD (T-score), associated thyroid nodular disease, previous cervical surgery.
All patients underwent conventional cervical US and double-phase MIBI scintigraphy with early SPECT/CT prior to surgery. Planar imaging was acquired 15min (early phase) and 3h (delayed phase) after the intravenous administration of 740MBq (20mCi) of Tc99m MIBI. SPECT/CT was performed in all cases immediately after early planar imaging. The SPECT/CT acquisition followed the current recommendations. A General Electric Infinia Xeleris 2 and a Siemens Symbia T16 scanner, both equipped with a dual-head high-resolution collimator, were used.
In doubtful or inconclusive MIBI cases, particularly those with coexisting thyroid nodes on US, subsequent Tc99m Thyroid Scintigraphy (conventional planar and SPECT-CT acquisitions) was performed on a different day.9 In the event of negative or non-concordant MIBI-US, subsequent 18F-choline, 11C-methionine or 11C-choline PET/CT and/or CT were performed according to the recommended procedures.9
Nuclear imaging studies were evaluated by two skilled independent nuclear physicians.
Two concordant preoperative imaging techniques, preferably one anatomical and one functional, were required to perform parathyroid surgery. The MIP approach was always attempted initially, except in cases of simultaneous thyroid surgery indication or known multiglandular disease, or rarely in some patients with previous cervical surgery or ectopic lesions in whom a longer cervical incision was required. Intraoperative histopathology determined the end of the intervention; definitive histopathology was the reference value. Gland weight (mg) was recorded.
The parathyroid glands located at the inferior pole of the thyroid gland or adjacent to its posterior surface were considered to be the lower and upper eutopic parathyroid glands, respectively. Those located at any other site, including intra-thyroid glands, were labelled as ectopic.
The normalisation of calcaemia lasting a minimum of 6 months after surgery indicated the success of the procedure (cure rate).2 Persistent HPT was defined as hypercalcemia within 6 months of the initial parathyroidectomy related to a surgical failure; recurrent HPT was defined as hypercalcemia occurring 6 months or more after surgery following a normocalcaemic interval.16
Sensitivity, positive predictive value (PPV) and accuracy were calculated for MIBI and US. For statistical analysis, all data were analysed using the IBM SPSS Statistics 25.0 program. Continuous variables are described as median (standard deviations) and mean (interquartile ranges). Categorical variables are described using percentages. Exact binomial 95% confidence intervals (CIs) are reported for proportions. The t test was used to compare the continuous variables and the χ2 analysis for categorical variables. A p value less than 0.05 was considered statistically significant.
ResultsPreoperative dataThe study included 223 patients, 179 (80.3%) females with a median age of 63.5 years. The preoperative laboratory data and other clinical features are shown in Table 1. The prevalence of concomitant nodular thyroid pathology, confirmed by ultrasound and/or other diagnostic procedures, was 59.6%. Previous cervical surgery was recorded in eight patients (3.6%), including three unsuccessful parathyroidectomies.
Patient characteristics.
| Age (years): median (IQR) | 63.5 (52.9–71.9) |
| Gender N (%) | |
| Female | 179 (80.3) |
| Male | 44 (19.7) |
| BMI (kg/m2): median (IQR) | 26 (23–29) |
| Surgical criterion prevalence N (%) | |
| Renal stones, nephro-urologic symptoms | 84 (37.6) |
| Calciuria (solitary) | 37 (16.6) |
| Osteoporosis/bone injury | 95 (42.6) |
| Age under 50 y. | 29 (13) |
| Hypercalcemia (solitary) | 51 (22.8) |
| Other symptoms (asthenia, psychiatric, …) | 3 (1.3) |
| Preoperative serum tests: median (IQR) | |
| Calcium (normal 8.4–10.2mg/dL) | 11 (10.6–11.4) |
| PTH (normal 14–80pg/mL) | 182 (142–254) |
| Vitamin D (normal 20–60ng/mL) | 19 (13–27) |
| Thyroid nodular pathology N (%) | |
| Not known | 90 (40.4) |
| Yes | 133 (59.6) |
| Previous cervical surgery N (%) | |
| None | 215 (96.4) |
| Parathyroid | 3 (1.3) |
| Thyroid | 4 (1.8) |
| Other | 1 (0.5) |
Median elapsed time from the MIBI diagnostic exploration to the date of surgery was 7 months (IQR: 5–11). These values for US were: median 7 (IQR: 4–9)
SurgeryThe most frequent surgical procedure was MIP (179 cases, 80.2%). This focused parathyroidectomy was radioguided in the last 46 (20.6%) patients, as this procedure was included recently in our centre (March 2020).
A cervicotomy was performed in 41 (18.4%) patients, mostly due to the concomitant indication of thyroid surgery (17), less frequently in cases of multiglandular disease (8 patients), cervical reoperation (5), ectopic parathyroid location (5) and as an intra-operative conversion of unsuccessful initial selective approach (6). Four of these six “extended surgeries” also corresponded to ectopic lesions; one was required to remove a very large lesion; finally, in one patient a cervicotomy was attempted to resolve an unsuccessfully initial minimal access, although the parathyroid lesion could not be found either.
Finally, three patients required a thoracoscopy, corresponding to one double adenoma, one mediastinal adenoma and one parathyroid carcinoma with extensive cervical and thoracic infiltration.
The parathyroid lesion was successfully removed from 211 (94.6%) patients, with 204 (96.7%) corresponding to adenomas (5 double), 6 (2.8%) hyperplasia and 1 carcinoma (0.5%).
With regard to anatomical location, 174 (82.5%) were found in the typical location, while 37 (17.5%) were excised from ectopic sites: mediastinum/intrathymic (11), retro-esophageal/prevertebral (11), tracheoesophageal groove (8), intrathyroid (5), pre-tracheal (2).
Considering the 12 failed surgeries, no parathyroid gland could be identified intraoperatively in 6, while in the remaining 6, the suspicious excised parathyroid gland was ultimately normal in the definitive histopathology.
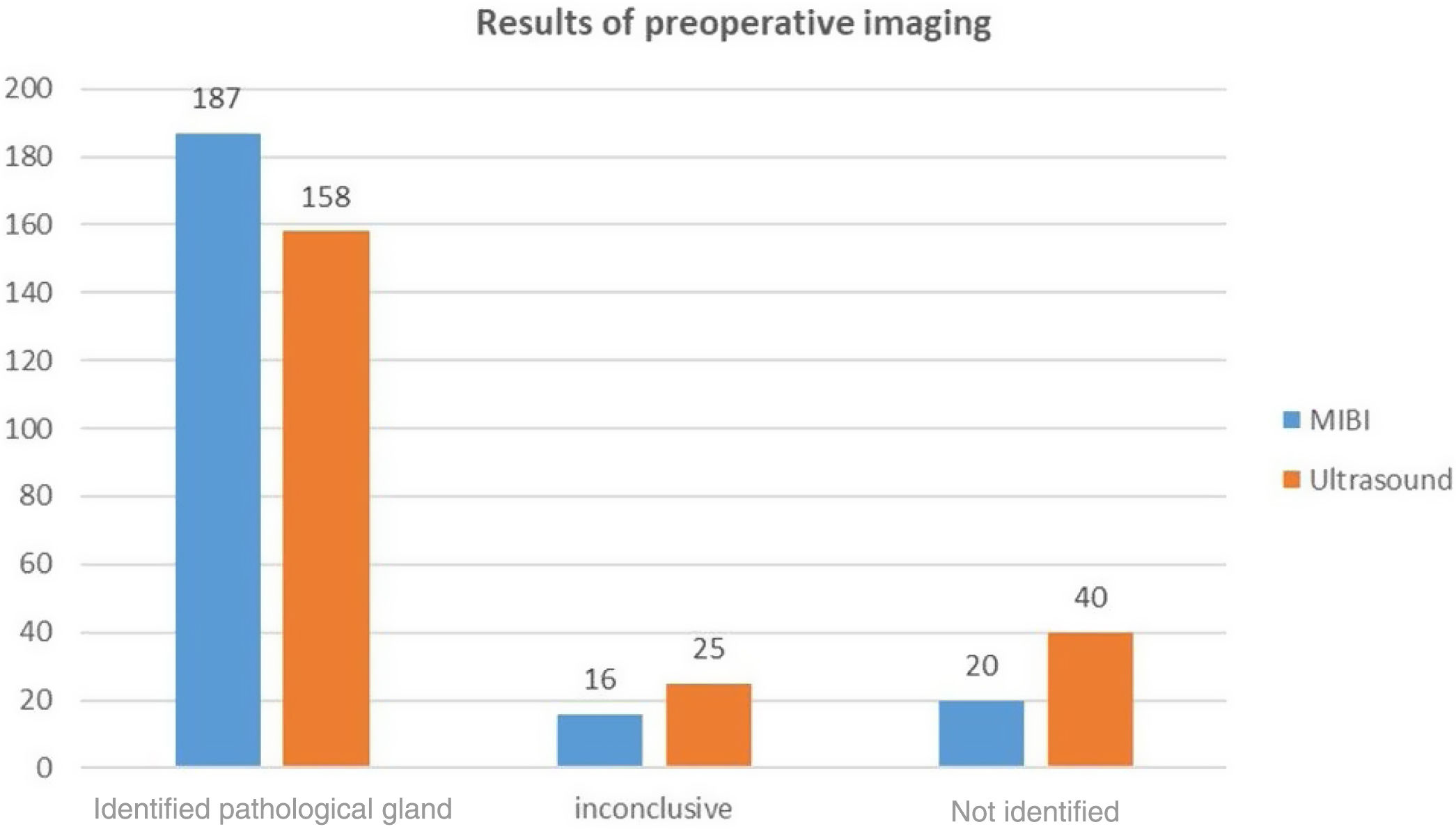
Preoperative diagnostic proceduresThe MIBI located the parathyroid lesions in 187 patients (83.9%) (32 in an ectopic site), failed to identify any pathological parathyroid gland in 20 (9%), and was inconclusive or doubtful in 16 (7.2%). Thus, the MIBI showed a sensitivity of 84%, a PPV of 95% and an accuracy of 80% (Fig. 1).
Additional thyroid scintigraphy was performed in 52 patients (23.3%) and contributed to diagnosis by MIBI in 47 (21%). Thus, the absence of thyroid nodes in concordance with the MIBI uptake focus, i.e. the MIBI (parathyroid)-Tc99m (thyroid) incongruence permitted the diagnosis of parathyroid lesion in 35 patients and the concordance with thyroid nodes excluded it in 12 patients.
On the other hand, preoperative US was positive in 158 patients (70.9%) (18 ectopic), negative in 40 (17.9%) and inconclusive or doubtful in 25 (11.2%). Hence, sensitivity, PPV and accuracy for US were 72%, 96% and 71%, respectively (Fig. 1).
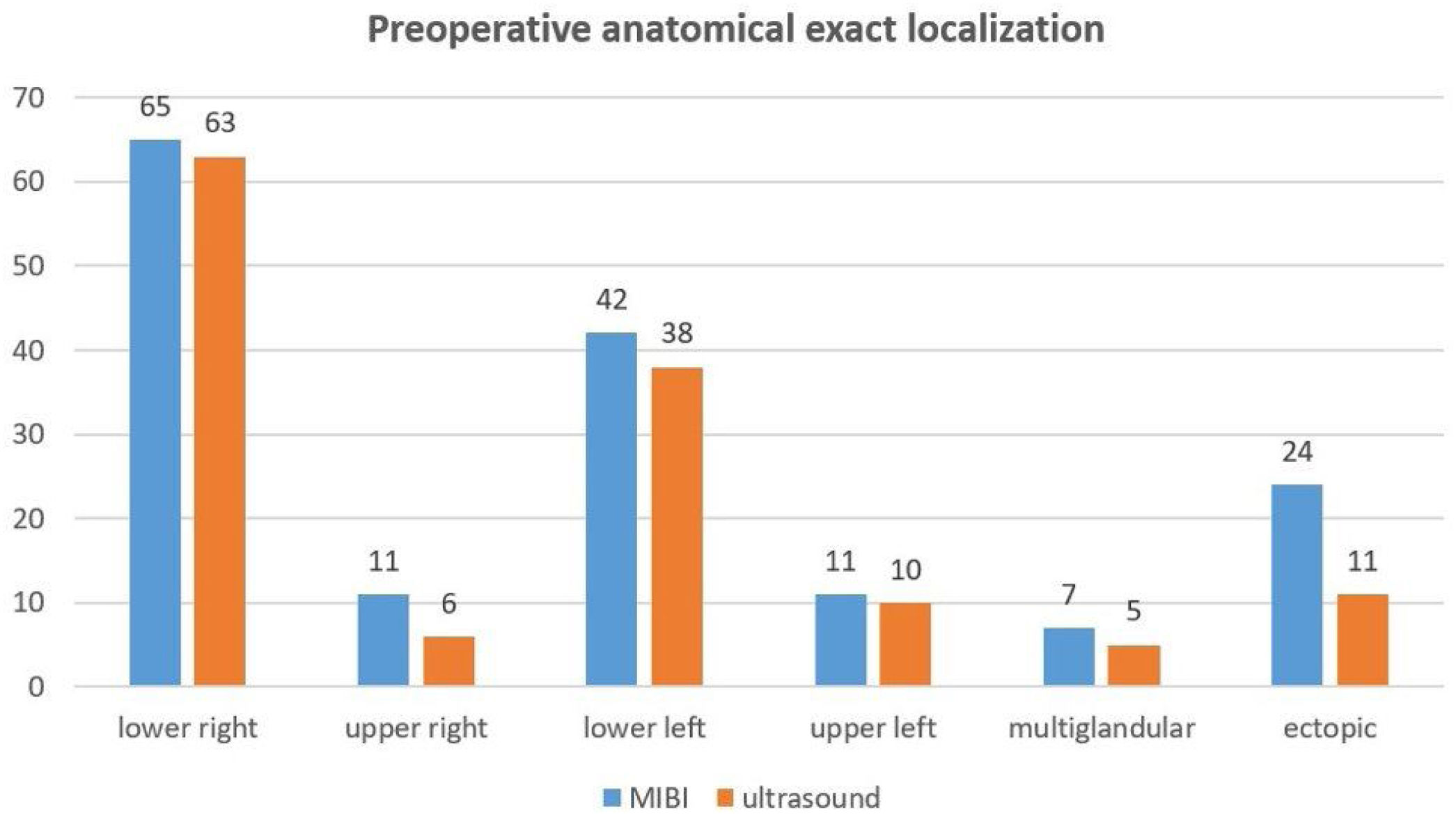
When compared with intraoperative findings, the MIBI reported the precise surgical location (exact quadrant, ectopic site) in 160 patients (75.8%). The MIBI exactly matched the anatomical quadrant in 136 (78%) of 174 patients with parathyroid lesions removed from the typical location (65 lower right gland, 11 upper right, 42 lower left, 11 upper left, 7 multiglandular disease) and specified the exact site in 24/37 glands resected from ectopic sites (64.8%) (Fig. 2).
On the other hand, US located the pathological gland in the correct intraoperative site in 133 (68.7%) patients, 122 eutopic (70.1%), 11 ectopic (29.7%). The MIBI-US difference to indicate the precise ectopic parathyroid site was significant (p=0.002).
In turn, MIBI and US were exactly concordant with each other in the anatomical localization of the lesion in 118 patients (53%), 108 eutopic and 10 ectopic. Some of the remaining 105 (47%) patients in whom either of these two techniques failed or were mismatched were explored with 18F-choline, 11C-methionine or 11C-choline PET/CT (67 cases) and/or CT (22) being diagnostic 64 (95%) and 16 (72%), respectively.
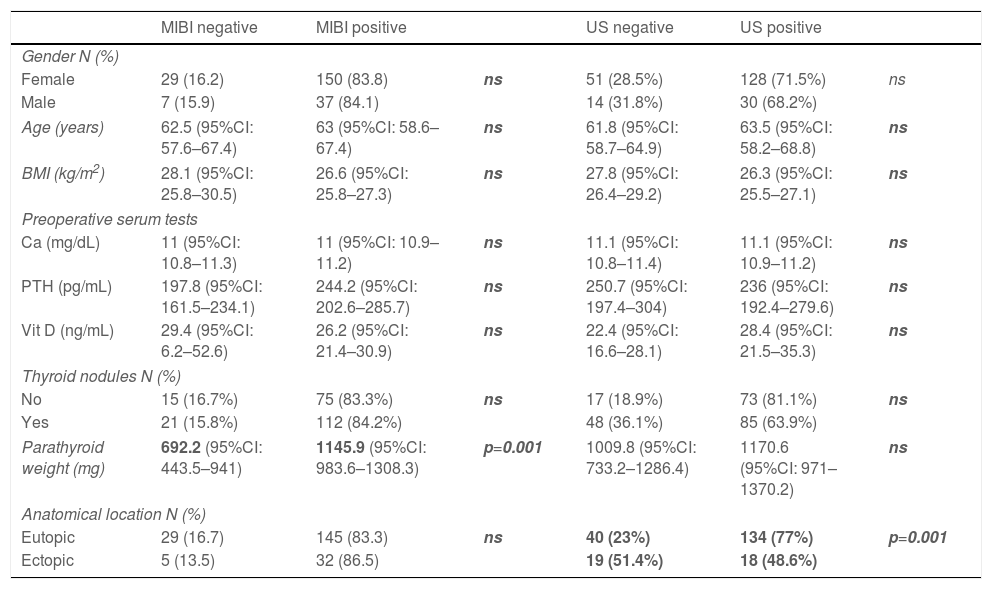
Factors related to preoperative localizationNeither MIBI nor US found a statistically significant difference in the location rate of the parathyroid lesion with regard to gender, age, BMI, calcium, PTH and 25-hydroxyvitamin D levels or the coexistence of concomitant thyroid nodular pathology (Table 2). In this regard, MIBI was positive in 112 (84.2%) patients with underlying thyroid pathology, doubtful or negative in 21 (15.8%), whereas US was positive in 85 (63.9%) and doubtful or negative in 48 (36.1%).
Factors related to MIBI/US location.
| MIBI negative | MIBI positive | US negative | US positive | |||
|---|---|---|---|---|---|---|
| Gender N (%) | ||||||
| Female | 29 (16.2) | 150 (83.8) | ns | 51 (28.5%) | 128 (71.5%) | ns |
| Male | 7 (15.9) | 37 (84.1) | 14 (31.8%) | 30 (68.2%) | ||
| Age (years) | 62.5 (95%CI: 57.6–67.4) | 63 (95%CI: 58.6–67.4) | ns | 61.8 (95%CI: 58.7–64.9) | 63.5 (95%CI: 58.2–68.8) | ns |
| BMI (kg/m2) | 28.1 (95%CI: 25.8–30.5) | 26.6 (95%CI: 25.8–27.3) | ns | 27.8 (95%CI: 26.4–29.2) | 26.3 (95%CI: 25.5–27.1) | ns |
| Preoperative serum tests | ||||||
| Ca (mg/dL) | 11 (95%CI: 10.8–11.3) | 11 (95%CI: 10.9–11.2) | ns | 11.1 (95%CI: 10.8–11.4) | 11.1 (95%CI: 10.9–11.2) | ns |
| PTH (pg/mL) | 197.8 (95%CI: 161.5–234.1) | 244.2 (95%CI: 202.6–285.7) | ns | 250.7 (95%CI: 197.4–304) | 236 (95%CI: 192.4–279.6) | ns |
| Vit D (ng/mL) | 29.4 (95%CI: 6.2–52.6) | 26.2 (95%CI: 21.4–30.9) | ns | 22.4 (95%CI: 16.6–28.1) | 28.4 (95%CI: 21.5–35.3) | ns |
| Thyroid nodules N (%) | ||||||
| No | 15 (16.7%) | 75 (83.3%) | ns | 17 (18.9%) | 73 (81.1%) | ns |
| Yes | 21 (15.8%) | 112 (84.2%) | 48 (36.1%) | 85 (63.9%) | ||
| Parathyroid weight (mg) | 692.2 (95%CI: 443.5–941) | 1145.9 (95%CI: 983.6–1308.3) | p=0.001 | 1009.8 (95%CI: 733.2–1286.4) | 1170.6 (95%CI: 971–1370.2) | ns |
| Anatomical location N (%) | ||||||
| Eutopic | 29 (16.7) | 145 (83.3) | ns | 40 (23%) | 134 (77%) | p=0.001 |
| Ectopic | 5 (13.5) | 32 (86.5) | 19 (51.4%) | 18 (48.6%) | ||
The mean weight of the excised parathyroid lesion was 692.2mg (95%CI: 443.5–941.0) in MIBI-negative patients, significantly lower than the gland weight of the MIBI-positives: 1145.9mg (95%CI: 983.6–1308.3); p=0.001. This regard was not significant on ultrasound.
MIBI was not significantly affected by parathyroid lesion location (Table 2), whereas ultrasound detection of ectopic glands was significantly diminished. In this regard, US identified 134 (77%) of eutopic glands and 18 (48.6%) of the ectopic: p=0.001.
Finally, in all eight patients with a cervical surgical background (including three previous unsuccessful parathyroid surgeries), MIBI location was obtained and a parathyroid adenoma was resected, three by MIP. Three glands were in an ectopic location.
Follow-upMedian follow-up is 34 months (IQR 22–47). All patients except two (lost to follow-up) were monitored for 6 months or longer (maximum 64 months).
Considering the group of successful surgeries first, five patients were closely monitored with the suspicion of recurrent HPT due to hypercalcaemia and inappropriately high PTH in the absence of Vitamin D deficit (recurrence rate 2.3%). The remaining patients remain eucalcaemic after six months.
Of the 12 patients whose surgery was unsuccessful, four were biochemically cured after 6 months despite having had a normal histologic result or a failed localization. The other 8 continued to present persistent hyperparathyroidism after 6 months (persistence rate 3.6%).
Therefore, overall cure rate is 94.2%.
Up until now, five of the eight persistent pHPT have been re-operated (4 bilateral explorations, 1 radio-guided PMI), and resection of an adenoma and biochemical cure were finally achieved in four of them. Only one of them was in an ectopic location. Repeated MIBI, as well as PET/CT in two and CT in another two, were decisive in the success of the second surgery.
DiscussionDouble-phase MIBI parathyroid scintigraphy is based on the slower washout of MIBI from the parathyroid glands than from thyroid tissue. Although its sensitivity is inferior to that of dual-tracer procedures,10,14,19 it has been used widely in parathyroid location, relying on its excellent results and ready accessibility.20
On the other hand, MIP is currently the surgical procedure of choice, at least in solitary adenomas. This targeted parathyroidectomy is highly effective in the treatment of pHPT,1 equal to the most extensive classical surgery.5
In our study, a minimally invasive approach was performed in 80% of the patients with pHPT and surgical indication, similar to other reports.10,21 This percentage seems appropriate, since most of the other cases had been preoperatively scheduled for cervicotomy because of the concomitant indication of thyroid resection or pre-surgical identification of multiglandular parathyroid disease. Overall, 94.6% of our surgeries were successful, with a confirmed cure rate of 94.2% and a recurrence rate of 2.3%. Four patients showed spontaneous remission, although no pathological parathyroid lesion was excised, which occurs exceptionally.22 A systematic review by Ishii et al. reported an overall mean recurrence and cure rates after MIP of 1.6% and 96.9%, respectively.6 Udelsman et al., in a large series of 1.650 patients, obtained an improvement in cure rate (99.4%) compared to conventional surgery (97.1%).7 In addition, the rate of complications, length of stay and total hospital charges also improved.
This minimally invasive approach is directly dependent on a precise preoperative localization, hence parathyroid scintigraphy plays an essential role in defining the surgical strategy.8 In this context, MIBI scintigraphy and US are the current first-line pre-surgical imaging techniques performed, as they constitute the most cost-effective strategy.2 MIBI-US concordance provides a high positive predictive value in MIP.14 In this context, a precise pre-operative localisation averts unsuccessful surgeries and reduces the risk of surgical conversion or failure.8
MIBI has demonstrated slightly higher sensitivity (83–93%),10,20 specificity (87–96%)23 and accuracy (83–96%)19,23 compared to US, probably based on technical developments, such as SPECT/CT hybrid acquisition, that improves resolution12 (Fig. 3). Thus, in a meta-analysis, Treglia et al. reported a pooled detection rate of MIBI SPECT/CT of 88% in pHPT.11 We acquired SPECT/CT in the early phase, which has been reported as the most accurate MIBI protocol24 (Fig. 3). The sensitivity and accuracy obtained (84% and 80%. respectively) were effectively higher compared to US (72%; 71%).
A 62-year-old woman with primary hyperparathyroidism. Planar MIBI shows no pathological uptake in early (A) or delayed (B) imaging. However, early SPECT/CT identifies a pre-vertebral parathyroid lesion (C, D), subsequently confirmed in PET Choline. US was negative. A parathyroid adenoma of 220mg was removed by PMI. The patient is biochemically cured.
The sensitivity of SPECT/CT is closely related to its ability to identify smaller lesions compared to planar image or SPECT alone.14,23,25 Moreover, it shows an improvement in precise parathyroid anatomical localization,26 which permits the surgical planning and guided resection of ectopic lesions.8 Hybrid SPECT/CT also improves parathyroid localization specificity, which is very interesting in patients with concomitant thyroid pathology,27 since false positive results diminish.23 Our study assessed all these theoretical advantages of SPECT/CT.
In this context, some biochemical factors, such as serum calcium or PTH28 and pathological features of parathyroid lesions such as weight and volume,29 percentage of oxyphilic cells,29 cystic component, hyalinization, etc., have been directly related to MIBI uptake and consequently to its sensitivity. In our study, the parathyroid weight was in fact the only factor significantly related to MIBI parathyroid detection, as described previously.26,29
The sensitivity of MIBI in identifying ectopic glands showed no relevant difference with regard to typically sited glands, and is even higher (86.5 vs 83.3), as reported elsewhere.18 However, the sensitivity of US in visualising ectopic glands was significantly lower (48.6% vs 77%), as has been widely reported in the literature.30
Neither was MIBI significantly affected by the coexistence of thyroid pathology. In patients with pHPT, concomitant thyroid disease is not rare (12–67%),2,31 being as high as 59.6% in our population. Current guidelines recommend preoperative thyroid evaluation in patients undergoing parathyroidectomy, since the coexisting thyroid disease can reduce preoperative techniques accuracy. Therefore, in these patients it is crucial to distinguish between thyroid nodules and pathological parathyroid tissue, as thyroid nodules can take up MIBI but parathyroid lesions rarely present Tc-99m uptake. A dual tracer acquisition, i.e. a thyroid scan after the double-phase MIBI, is recommended in endemic goitre areas.14
Accordingly, we performed an additional subsequent thyroid scintigraphy in 23.3% of the patients, which was useful in clarifying diagnosis by MIBI in most of them (21% of the entire series) who, in the absence of this test, would have been misclassified. Hence Tc-99m thyroid imaging encouraged the diagnosis of parathyroid lesion, averting a false negative result in 35 patients and avoided a MIBI-false positive due to thyroid uptake in 12 patients. In this context, Huang et al. report that the diagnosis changed in 13.1% of the patients after accounting for Tc-99m scintigraphy, thus diminishing false positive and false negative MIBI results.19
One of the major benefits of MIBI SPECT/CT is that it can define the anatomical location of a parathyroid lesion exactly. This permits a more direct and minimally extensive approach, shorter surgery time and fewer complications. Concordance rates of 68.5-80%26,27 have been reported between the precise anatomical preoperative location with SPECT/CT and the place where the glands are finally found in surgery. These results vary, depending on the gold standard (laterality vs quadrant) and are usually worse when thyroid pathology coexists.
In our study, the accuracy of MIBI in locating the exact site of a pathological parathyroid gland was 75.8%, although we considered the identification of the exact quadrant or precise ectopic location, not only laterality, as a requirement for concordance. In fact, most of our mismatched cases corresponded to adenomas reported at a typical location but were found intraoperatively in a more posterior location with respect to the thyroid bed, and therefore an ectopic site, despite being on the same cervical side. On the other hand, US showed less overall anatomical accuracy with regard to the exact surgical location, related to its particularly poor ability to determine the ectopic ubication precisely (29.7%).
In this context, the exact concordance between MIBI and US with regard to the same quadrant or ectopic site was 53%, similar to other reports.20 Thus, Ebner et al. found that MIBI-US matched in 76% but concerning the laterality of the lesion.21
The two main causes of unsuccessful parathyroid surgery are the existence of ectopic glands and undetected multiglandular disease.14 MIBI's accuracy and sensitivity decreases in parathyroid hyperplasia,32 so the preoperative identification of multiple disease can avoid inappropriately limited to one gland surgery. It should be noted that none of the re-operated patients in our series corresponded to parathyroid hyperplasia.
Repeated surgery implies a reduction in the success rate and accuracy. Stack et al. revealed lower healing rates in reoperation (84%) compared to first surgery (95%).16 Moreover, second surgery involves an increase in the risk of surgical complications.14,16 Therefore, re-operative parathyroid surgery should be performed exclusively in patients in whom a target gland is identified in preoperative explorations, meaning that imaging localization is mandatory to identify the missing gland and permit its excision.8 Frey et al. healed 62% patients with persistent pHPT by performing a second MIBI that identified a new pathological gland in 50% of the cases.17
Hitherto, in overall assessment, we have carried out a second parathyroid surgery in 8 patients (five due to persistent HPT and three included initially with a history of previous parathyroid surgery), seven of which were successful. Half of the excised adenomas were removed from an ectopic location.
One of the limitations of our study was the long time that elapsed between the MIBI and surgery, which could affect its sensitivity. In addition, in some patients the postoperative follow-up is relatively insufficient to be able to determine the definitive rate of recurrence.
Moreover, the low percentage of patients with multiglandular disease and re-operated cases is insufficient to draw conclusions in these patient subgroups.
ConclusionsMIBI SPECT/CT delivers higher sensitivity and accuracy than US in pre-surgical anatomical localization in pHPT. Correct preoperative imaging permits a successful MIP in most patients, regardless of the lesion's typical or ectopic location.
The only factor significantly related to the sensitivity of MIBI SPECT/CT is gland weight. Underlying nodular thyroid pathology does not cause a decrease in the MIBI's detection rate in relation to the benefit of the thyroid scan.
A multidisciplinary approach to the entire procedure and management in referral Units would seem mandatory.
FundingThis research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Conflict of interestThe authors declare that there is no conflict of interest that could be perceived as compromising the impartiality of the research reported.
The authors express their great appreciation for the valuable collaboration of the participating Departmental staff in the development of this work.