Mononeuritis multiplex (MM) is an infrequent disorder that may be secondary to a number of diseases, which makes aetiological diagnosis difficult.1 Infectious and inflammatory aetiologies may be difficult to differentiate. Magnetic resonance imaging (MRI) and cerebrospinal fluid (CSF) analysis are useful tools for determining the cause of MM. We present the challenging case of a patient with MM whose symptoms were initially thought to be associated with herpes simplex virus (HSV) infection but who later developed the typical symptoms of systemic lupus erythematosus (SLE). Very few cases of MM secondary to SLE have been described in the literature2; cases of MM as an initial manifestation of SLE are even rarer. Our patient was a 42-year-old man with a history of hemifacial spasm due to left-sided facial paralysis in adolescence and recurrent symptoms of oral herpes virus infection.
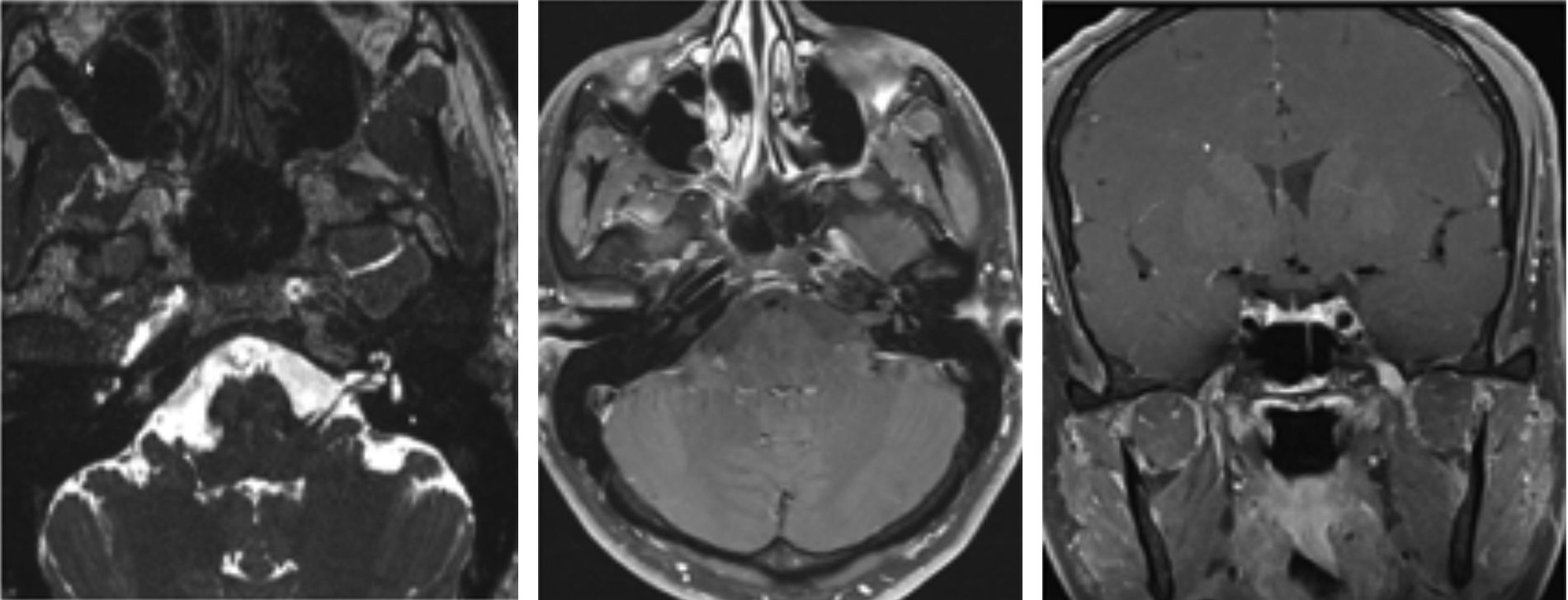
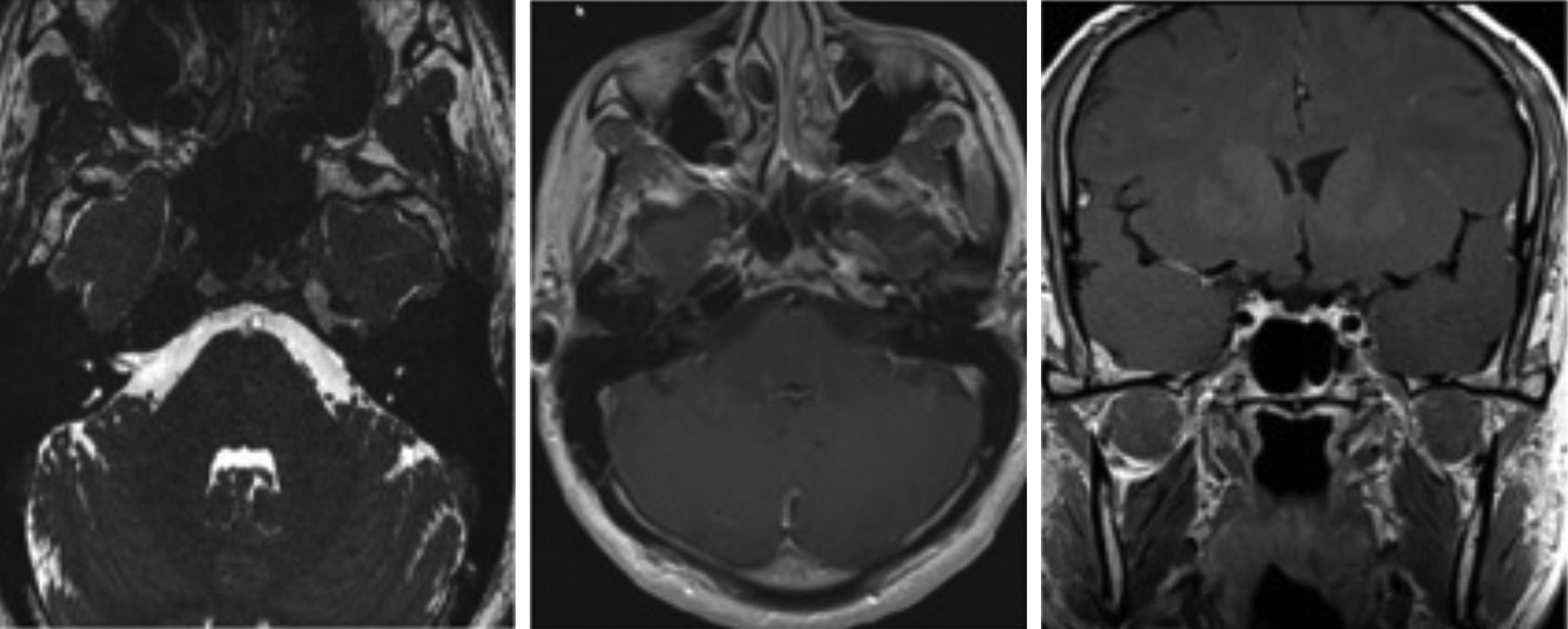
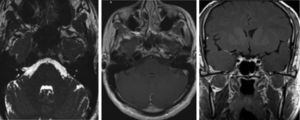
The patient came to our department due to left-sided facial dysaesthesia, which was interpreted as neuralgia of the second branch of the left trigeminal nerve. Symptomatic treatment achieved little improvement. A brain MRI scan revealed thickening of the left trigeminal nerve (Fig. 1). Our patient had experienced recurrent symptoms of oral herpes virus infection a month previously; the MRI findings were therefore thought to be due to HSV reactivation. The patient returned to our department 9 months later, reporting worsening of the dysaesthesia; he also presented diplopia, secondary to left sixth cranial nerve palsy. We performed an additional brain MRI scan: thickening of the second branch of the trigeminal nerve persisted, with the sixth cranial nerve showing no alterations. A CSF analysis disclosed no relevant findings, viral serology results were negative, and the results of an immunological study were negative for antiphospholipid antibodies and positive for antinuclear antibodies (1:320). The patient was not receiving any drugs that may have induced lupus erythematosus. Due to suspicion of MM of inflammatory origin, we started treatment with megadose methylprednisolone therapy, achieving symptom improvement after 3 weeks of treatment. The patient was examined by the rheumatology department, reporting a 6-month history of arthritis affecting the elbows and lower limbs, which prevented him from exercising, a 2-month history of mouth ulcers, and photosensitivity. These symptoms, together with the presence of positive antinuclear antibodies, pointed to SLE.3,4 The patient was diagnosed with SLE as the initial manifestation of MM, and started treatment with cyclophosphamide; symptoms disappeared and the MRI findings of nerve thickening and contrast uptake resolved (Fig. 2). Around 50% of patients with SLE display central nervous system (CNS) involvement.5 This usually occurs 2 years after diagnosis of SLE.4 Cranial nerve palsy is infrequent, accounting for 0.5%-1% of all neuropsychiatric manifestations.5 Most of the cases published in the literature report isolated cranial nerve palsies, with cranial MM being extremely rare.2 Cranial nerve palsy is rarely associated with SLE; palsies are normally secondary to a concomitant central or peripheral nervous system disorder (meningitis, Guillain-Barré syndrome, or cavernous sinus inflammation). In many cases, the pathogenic mechanism of cranial neuropathies in SLE is difficult to determine. Several mechanisms have been proposed; the most widely accepted is antibody-mediated neuronal involvement, which causes vasculopathy, intrathecal production of proinflammatory cytokines, and accelerated atherosclerosis.6 It is uncertain whether the pathogenic mechanism of SLE is inflammatory, thrombotic, or mixed. The eighth and tenth cranial nerves are the most frequently affected in SLE.7 The literature describes 2 cases of isolated twelfth cranial nerve involvement secondary to SLE8,9 and 3 cases of isolated fifth cranial nerve involvement.10 Optic neuropathy is the most frequent neuro-ophthalmological manifestation of SLE.7 Ocular involvement secondary to cranial nerve palsy is rare, with the sixth cranial nerve being the most frequently involved.7 Regarding MM, Keane2 examined the causes of multiple cranial neuropathy in 979 patients and found only one case secondary to SLE. The literature includes 2 cases of MM associated with SLE: one patient with SLE and sarcoidosis who displayed third and sixth cranial nerve involvement combined with peripheral neuropathy,5 and another patient with SLE with neuro-ophthalmological manifestations, who was diagnosed with left-sided MM secondary to SLE.7 To our knowledge, this is the first case of MM associated with fifth and sixth cranial nerve involvement as the initial manifestation of SLE. Immunosuppressive treatment (cyclophosphamide or azathioprine) and corticosteroids are indicated for inflammatory MM. Patients with positive antiphospholipid antibodies should also receive anticoagulation therapy.6 Our patient responded well to cyclophosphamide. No diagnostic algorithm is available for MM due to the lack of evidence-based guidelines. In these cases, we should aim to detect biomarkers or neuroimaging findings that might identify the underlying pathological mechanism. SLE should be considered in the differential diagnosis of MM.
Axial T2-weighted and axial postcontrast fat-suppressed T1-weighted MR images display uniform thickening and contrast uptake in the maxillary branch of the left trigeminal nerve from the Meckel cave to the pterygopalatine fossa. Coronal T1-weighted sequence showing nodular thickening of the mandibular branch of the left trigeminal nerve at the foramen ovale.
The authors have received no funding.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Crespo Cuevas AM, Hervás Garcia JV, Abraira del Fresno L, Grau López L. Multineuritis craneal como comienzo de lupus eritematoso sistémico: un reto diagnóstico. Neurología. 2018;33:135–137.