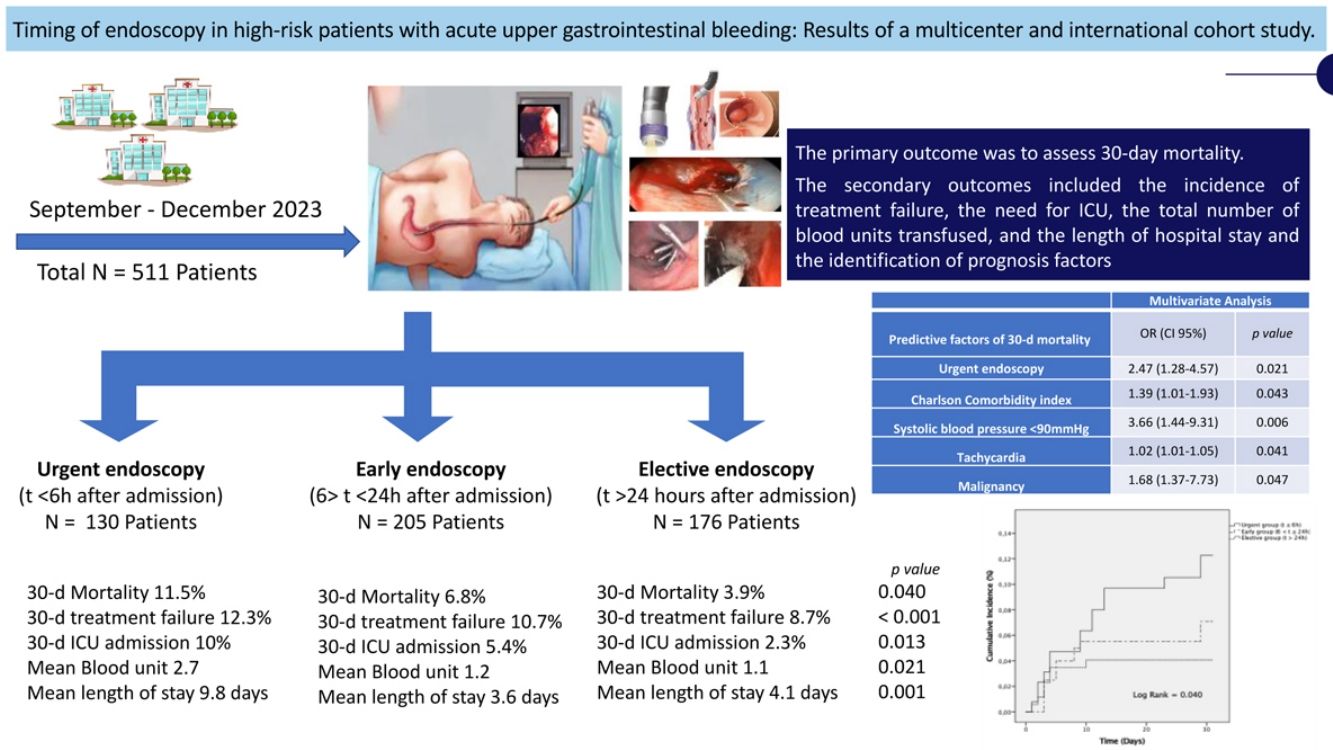
The optimal timing for high-risk patients with acute upper gastrointestinal bleeding (AUGIB) remains uncertain. The study aimed to evaluate whether the timing of endoscopy influences outcomes in high-risk patients with AUGIB.
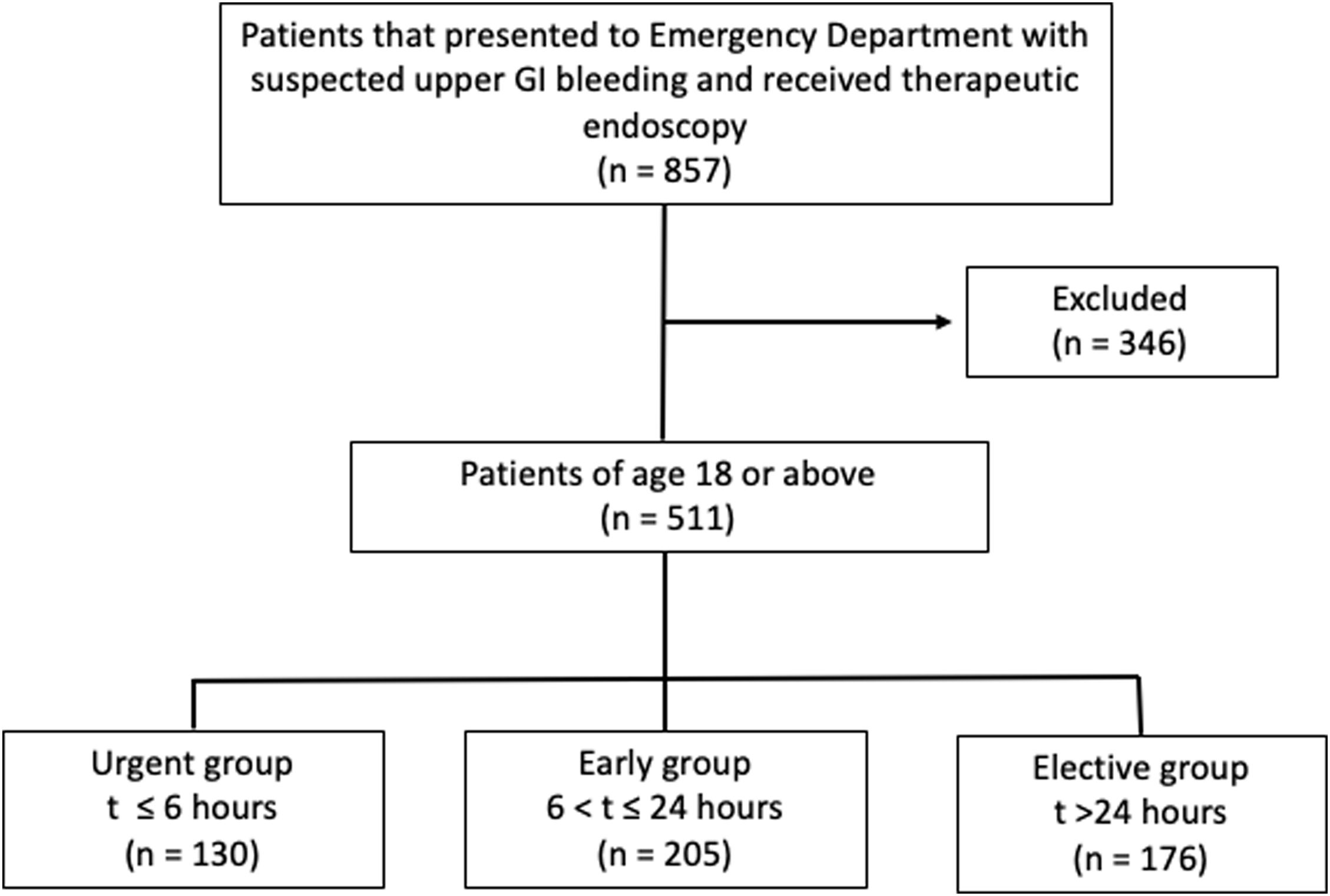
Patients and methodsWe conducted a retrospective, international, multicenter cohort study. High-risk patients (Glasgow–Blatchford score >7 points) with AUGIB, who underwent therapeutic endoscopy between September and December 2023 (n=511), were recruited. Patients were classified into three groups based on endoscopic timing: urgent (t≤6h), early (6<t≤24h) and elective (t>24h). Using descriptive statistics and logistic regression analyses, we identified the optimal timing for endoscopy and analyzed its association with 30-day outcomes, adjusting for confounding factors.
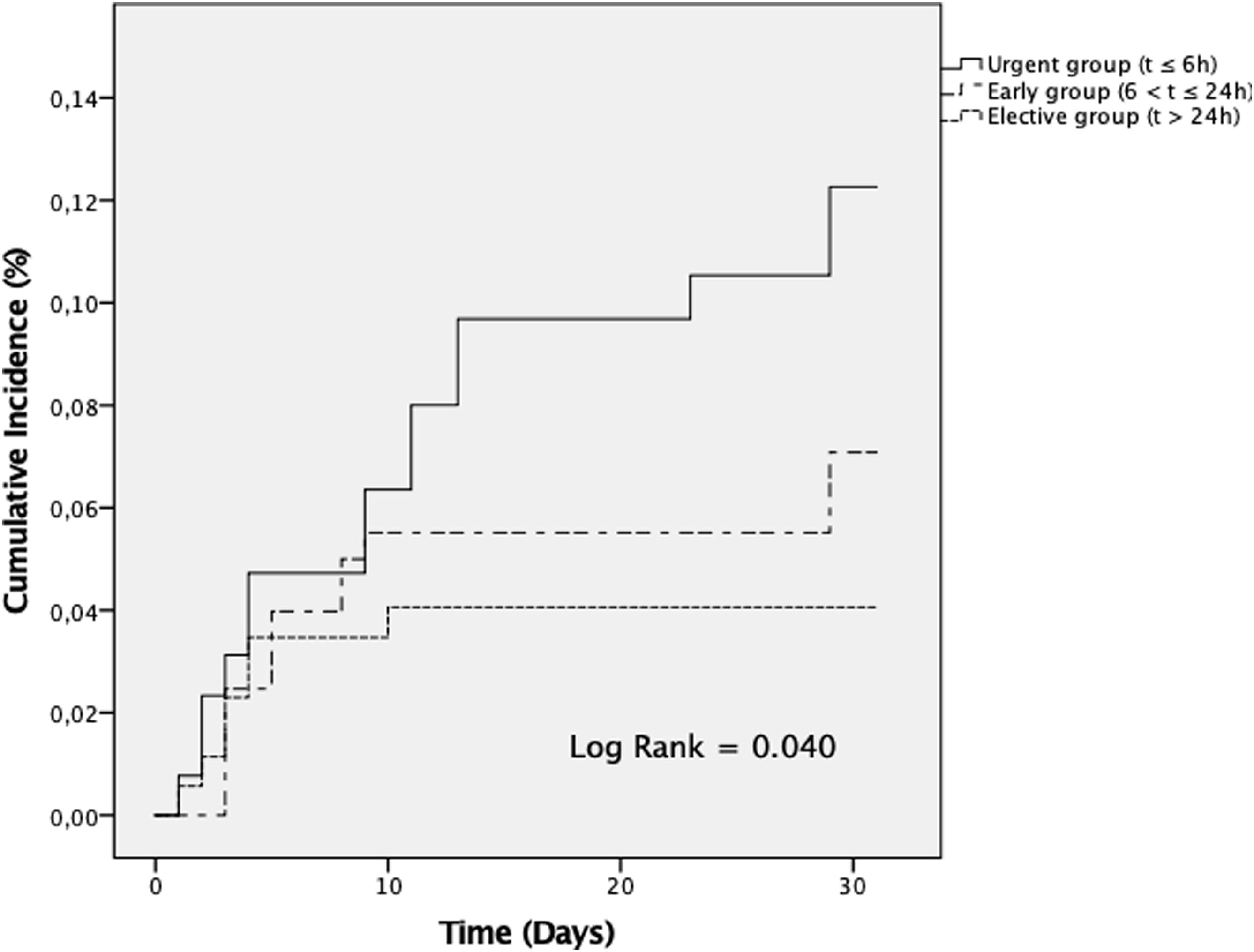
ResultsThe results showed that urgent timing (n=130) was associated with worse outcomes compared to early (n=205) and elective (n=176) endoscopy, including higher 30-day all-cause mortality (p=0.047), increased rates of repeat endoscopy (p=0.034), higher 30-day transfusion rates (p=0.021), and longer lengths of stay (p=0.038). These findings were particularly consistent among patients admitted with non-variceal bleeding. In the multivariate analysis, urgent endoscopy (OR 2.47, 1.28–4.57), Charlson index (OR 1.39, 1.01–1.93), systolic blood pressure <90mmHg (OR 3.66, 1.44–9.31), tachycardia (OR 1.02, 1.01–1.05), and malignancy (OR 1.68, 1.37–7.73) were identified as worse prognostic factors.
ConclusionsHigh-risk patients with AUGIB who underwent urgent endoscopy exhibited worse outcomes, particularly those patients with non-variceal bleeding. Comorbidities, shock, urgent endoscopy and malignancy were identified as predictors of 30-day mortality. These findings highlight the importance of prior resuscitation, pharmacotherapy, and early endoscopy.
El momento óptimo para realizar la endoscopia en los pacientes de alto riesgo con hemorragia digestiva alta aguda (HDAA) sigue siendo incierto. El objetivo fue evaluar el impacto del momento de la endoscopia en los pacientes de alto riesgo con HDAA.
Pacientes y métodosSe llevó a cabo un estudio de cohorte retrospectivo, internacional y multicéntrico. Se reclutaron pacientes de alto riesgo (Score Glasgow-Blatchford >7 puntos) con HDAA que se sometieron a una endoscopia terapéutica entre septiembre-diciembre 2023 (n=511). El tiempo a la endoscopia se clasificó: urgente (t≤6h), precoz (6<t≤24h) y electiva (t>24h).
ResultadosLa endoscopía urgente (n=130) se asoció a un mayor impacto frente la endoscopía precoz (n=205) y electiva (n=176), incluyendo una mayor mortalidad (p=0,047), tasas de endoscopía second-look (p=0,034) y de transfusión a 30 días (p=0,021), y una mayor estancia hospitalaria (p=0,038). Estos hallazgos fueron particularmente consistentes en los pacientes con hemorragia no variceal. En el análisis multivariante, la endoscopía urgente (OR: 2,47; 1,28-4,57), el índice de Charlson (OR: 1,39; 1,01-1,93), la presión arterial sistólica <90mmHg (OR: 3,66; 1,44-9,31), la taquicardia (OR: 1,02; 1,01-1,05) y la etiología maligna (OR: 1,68; 1,37-7,73) fueron identificados como factores de mal pronóstico.
ConclusionesLos pacientes de alto riesgo de HDAA que fueron sometidos a una endoscopía urgente presentaron peores resultados, especialmente aquellos con sangrado no variceal. Las comorbilidades asociadas, el shock, la endoscopía urgente y la etiología maligna fueron predictores de mortalidad a corto plazo. Estos hallazgos resaltan la importancia de la reanimación, la farmacoterapia y la endoscopía precoz.