The prevalence of dementia is growing in Spain, and so is the number of caregivers who are considering the institutionalization of their relatives. The purpose of this study is to identify which variables are associated with caregivers’ desire for institutionalization of their dementia relatives.
Patients and methodsInformal caregivers of 243 individuals suffering from dementia were interviewed. Predisposing variables (sociodemographic and contextual variables), stressors (dementia-related and caregiving-related aspects), appraisals (of circumstances and caregivers’ role), resources (personal and community-based resources) and the desire to institutionalize were evaluated.
ResultsOver half of the caregivers (52.6%) indicated that they had some desire to institutionalize their relatives with dementia. Stepwise regression analysis revealed that caregivers’ consideration to institutionalize was associated with being a male caregiver, not being the spouse of the dementia patient, and with a higher consideration and higher use of community-based formal resources (short-term nursing home use, adult day care centres and psycho-stimulation).
ConclusionsAssessing and using formal resources outside their homes help caregivers overcome barriers that keep them from considering the institutionalization of their relatives. The difficulty in considering institutionalizing their relatives is more evident among spouses, who have stronger attachments with the dementia patients, especially among females, who probably feel obliged to continue developing caregiver roles because of their gender.
El número de personas con demencia en España es cada vez mayor y también aumenta la cantidad de cuidadores que consideran la institucionalización de sus familiares. El objetivo de este estudio es analizar las variables asociadas al deseo por parte del cuidador de institucionalizar a su familiar mayor con demencia.
Pacientes y métodosSe entrevistó a 243 cuidadores familiares de personas con demencia. Fueron evaluadas variables predisponentes (sociodemográficas y contextuales), estresores (relacionados con la demencia y el cuidado), valoración (de la situación y del rol de cuidador), recursos (personales y comunitarios) y el deseo de institucionalización.
ResultadosMás de la mitad de los cuidadores (52,6%) manifestó en alguna medida estar considerando la institucionalización del familiar con demencia. Un análisis de regresión múltiple por pasos muestra que ser varón, tener un parentesco con el enfermo distinto del de cónyuge, así como haber valorado y utilizado en mayor grado los recursos formales comunitarios (residencia esporádica, centro de día y psicoestimulación) se asocian a una mayor consideración de institucionalización en los cuidadores.
ConclusionesLa valoración y posterior utilización de recursos formales fuera del hogar parece servir para romper las barreras que impiden que los cuidadores valoren ingresar a su familiar en una residencia. La dificultad para plantearse la institucionalización es más evidente en los cónyuges, que tienen unos vínculos más fuertes con la persona con demencia, y especialmente en las cuidadoras, quienes probablemente se sienten más obligadas a continuar con el cuidado por su condición de mujeres.
Dementia is one of the most common and troublesome disorders among the elderly. It affects not only those who suffer it, but also the whole family environment. It is well known that caring for a relative with dementia is associated with negative consequences for caregivers1 and this often leads to the realisation that the situation can no longer continue, leaving institutionalisation as the best alternative. There are increasingly more dementia patients attended at residential environments, the figure in our area being currently estimated at 33% of all residence users.2 Up to 20% of people with dementia are institutionalised in the first year after diagnosis, 50% at 5 years and about 90% at 8 years.3 Different reviews3,4 indicate that the desire for institutionalisation on the part of the caregiver (in other words, firmly considering institutionalisation) is a key predictor of admission of dementia patients. Numerous studies5–7 have shown that it is the best independent predictor of future institutionalisation of the relative.
The institutionalisation of a relative with dementia is not an improvised decision; on the contrary, it is often the result of long reflection and consultation.5 In the same way that the care of people with dementia in their homes is not the best option in all situations, neither is the institutionalisation of all patients. In any case, institutionalisation is generally considered as a last resort, especially when this possibility is contemplated by spouses.8,9
An interesting quantitative and qualitative study conducted in the Region of Madrid10 reported that residences were generally rejected or considered as a last option because families believed that institutionalisation of a relative with dementia represented abandonment or failure. In fact, although caregivers considered that the rotation of the patient through different households could have inappropriate consequences for the patient, this was preferable to institutionalisation. Furthermore, female caregivers were those who felt most guilty when discussing the possibility of institutionalising family members with dementia.
The stress interaction model has been used successfully to explain the specific experience of stress suffered by carers of people with dementia, as well as to analyse the factors that determine the desire to institutionalise these patients.3,11 This model considers predisposing variables (socio-demographic data), stressors (associated with dementia and care), assessment variables (involving status and role as a caregiver) and resources (personal and community resources). According to different authors, these variables should be extended to include the possible influence of cultural variables in the decision to institutionalise relatives.7,9 One of the cultural variables that has received most attention in the literature on caregivers is familism. This term refers to the belief in the family as having more value than the single individual, assuming that loyalty to the family should be maintained, supporting it and, if necessary, sacrificing personal interests for its sake.12
Several studies have considered different variables related to the desire to institutionalise a family member with dementia. However, these studies are especially scarce in our country10,13 and present several limitations, such as the absence of a specific theoretical framework and the little attention paid to the role of formal services that the caregiver knows, uses and values. In fact, when formal services used are assessed as predictors of the desire for institutionalisation, this is only done considering the total number of these services used,6–8,11,13 regardless of the frequency of their use, the desire to use them or the knowledge about them. Furthermore, although cultural variables such as familism have recently been taken into account in the analysis of caregiver stress,14 these values have not been considered in the assessment of the institutionalisation process of people with dementia.15
The aim of this study was to determine which variables predict the desire for institutionalisation in the Region of Madrid, avoiding the above limitations, so as to know under what conditions people begin to end their role as caregivers of relatives with dementia at home.
Patients and methodsSubjectsWe conducted interviews with 243 caregivers of people with dementia in the Region of Madrid who were linked to social services (social service centres, day care centres), healthcare services (health centres, hospitals) or family associations. In order to participate in the study, these caregivers had to dedicate at least 1 hour per day to the care of their relative with dementia for a period of at least 3 months.
VariablesPredisposing variablesWe analysed socio-demographic factors: age, gender, marital status, educational level and relationship of the caregiver.
In addition, we also assessed familism as a contextual variable using the familism scale.14 This scale assesses the perceived obligation to provide material and emotional support to family members, the perception of family members as reliable providers of help and support to solve problems, and the family as an attitudinal and behavioural reference.
StressorsWe analysed stressors related with dementia: level of dependence, as assessed by the Barthel index,16 and frequency of problematic and memory behaviours associated with dementia, as assessed by the “Revised list of memory and behavioural problems” (LPMC-R).17
We also evaluated stressors related with care, among which we included the health of caregivers as proposed in the model by Luppa et al.3 We analysed daily hours devoted to care and period of time caring (assessed by ad hoc questions), leisure activities and satisfaction associated with them (assessed with the scale measuring satisfaction with leisure time17), depression (assessed with the CES-D scale18), anxiety (assessed with the POMS scale19) and anger (assessed with the STAXI-2 scale20).
EvaluationWe evaluated factors associated with the assessment that caregivers made of their situation: burden assessed with the Zarit scale21 and discomfort related to problematic behaviours assessed with the LPMC-R scale.17
We also evaluated factors associated with the caregivers’ own assessment of their performance as such: dysfunctional thoughts (assessed using a questionnaire on dysfunctional thoughts on care22) and self-efficacy to request help, to manage problematic behaviours and to control negative thoughts (assessed by the self-efficacy in care scale23).
Available resourcesWe analysed personal resources: social support assessed with the psychosocial support questionnaire,24 as well as the specific social support by religious groups with the religious community support questionnaire.25
We also assessed the community resources available using the scale of knowledge, use and valuation of resources.17 This scale assesses how much the caregiver knows, appreciates and uses a variety of support services offered by the community. We evaluated the knowledge, appreciation and/or sporadic use of residences (temporary, occasional or overnight stay), as well as resources outside the home for the person with dementia (day care centre, psychostimulation), resources within the home for the person with dementia (home help service, remote assistance and financial aid) and the therapeutic resources for the caregiver (psychological support and self-help groups).
Desire for institutionalisationWe used a scale to assess the desire for institutionalisation,6,26 which indicated whether the caregivers had mentioned institutionalisation to family and friends or with professionals, if they had obtained information on a possible residence, or if they had contacted, visited, taken their relatives to or applied for admission at a residence. The scale has 7 dichotomous questions (yes/no answers) and the range of total scores is between 0 and 7. In the present study, it showed an adequate internal consistency (Cronbach's alpha=0.85).
Data analysisWe performed stepwise regression analysis to identify predictors of the desire for institutionalisation by caregivers among the study variables. In the first step of the analysis, we introduced the predisposing variables. In the second, we introduced stressor variables along with the significant variables from the first step. In the third step, we introduced the assessment variables along with significant variables from the previous steps. In the fourth and final step, we introduced caregiver resources along with the significant variables from the preceding steps.
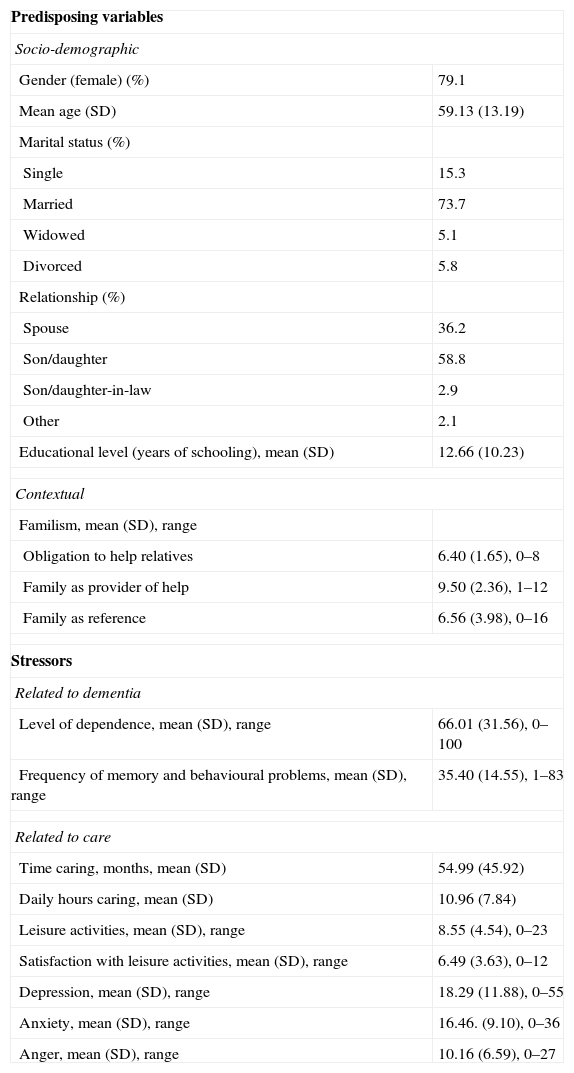
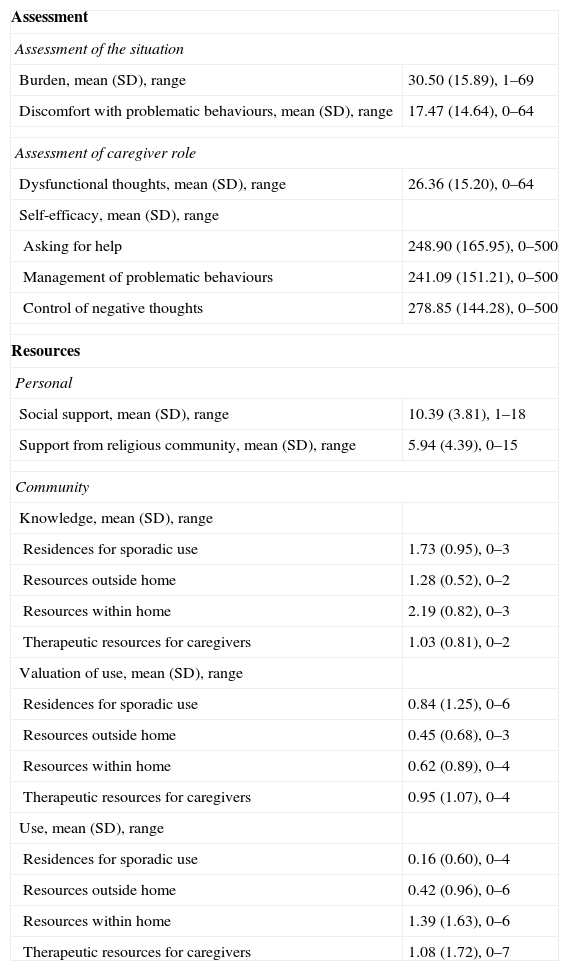
ResultsThe 243 caregivers in the sample, whose characteristics are shown in Tables 1 and 2, had a mean score of 1.78 (DT=2.15) in their desire to institutionalise. Data from this study indicated that 52.6% had considered institutionalising their relatives on some level (talking with friends, visiting a nursing home, etc.).
Predisposing (socio-demographic and contextual) variables and stressors in caregivers of persons with dementia (n=243).
| Predisposing variables | |
| Socio-demographic | |
| Gender (female) (%) | 79.1 |
| Mean age (SD) | 59.13 (13.19) |
| Marital status (%) | |
| Single | 15.3 |
| Married | 73.7 |
| Widowed | 5.1 |
| Divorced | 5.8 |
| Relationship (%) | |
| Spouse | 36.2 |
| Son/daughter | 58.8 |
| Son/daughter-in-law | 2.9 |
| Other | 2.1 |
| Educational level (years of schooling), mean (SD) | 12.66 (10.23) |
| Contextual | |
| Familism, mean (SD), range | |
| Obligation to help relatives | 6.40 (1.65), 0–8 |
| Family as provider of help | 9.50 (2.36), 1–12 |
| Family as reference | 6.56 (3.98), 0–16 |
| Stressors | |
| Related to dementia | |
| Level of dependence, mean (SD), range | 66.01 (31.56), 0–100 |
| Frequency of memory and behavioural problems, mean (SD), range | 35.40 (14.55), 1–83 |
| Related to care | |
| Time caring, months, mean (SD) | 54.99 (45.92) |
| Daily hours caring, mean (SD) | 10.96 (7.84) |
| Leisure activities, mean (SD), range | 8.55 (4.54), 0–23 |
| Satisfaction with leisure activities, mean (SD), range | 6.49 (3.63), 0–12 |
| Depression, mean (SD), range | 18.29 (11.88), 0–55 |
| Anxiety, mean (SD), range | 16.46. (9.10), 0–36 |
| Anger, mean (SD), range | 10.16 (6.59), 0–27 |
Assessment variables and variables from resources of caregivers of persons with dementia (n=243).
| Assessment | |
| Assessment of the situation | |
| Burden, mean (SD), range | 30.50 (15.89), 1–69 |
| Discomfort with problematic behaviours, mean (SD), range | 17.47 (14.64), 0–64 |
| Assessment of caregiver role | |
| Dysfunctional thoughts, mean (SD), range | 26.36 (15.20), 0–64 |
| Self-efficacy, mean (SD), range | |
| Asking for help | 248.90 (165.95), 0–500 |
| Management of problematic behaviours | 241.09 (151.21), 0–500 |
| Control of negative thoughts | 278.85 (144.28), 0–500 |
| Resources | |
| Personal | |
| Social support, mean (SD), range | 10.39 (3.81), 1–18 |
| Support from religious community, mean (SD), range | 5.94 (4.39), 0–15 |
| Community | |
| Knowledge, mean (SD), range | |
| Residences for sporadic use | 1.73 (0.95), 0–3 |
| Resources outside home | 1.28 (0.52), 0–2 |
| Resources within home | 2.19 (0.82), 0–3 |
| Therapeutic resources for caregivers | 1.03 (0.81), 0–2 |
| Valuation of use, mean (SD), range | |
| Residences for sporadic use | 0.84 (1.25), 0–6 |
| Resources outside home | 0.45 (0.68), 0–3 |
| Resources within home | 0.62 (0.89), 0–4 |
| Therapeutic resources for caregivers | 0.95 (1.07), 0–4 |
| Use, mean (SD), range | |
| Residences for sporadic use | 0.16 (0.60), 0–4 |
| Resources outside home | 0.42 (0.96), 0–6 |
| Resources within home | 1.39 (1.63), 0–6 |
| Therapeutic resources for caregivers | 1.08 (1.72), 0–7 |
Of the total sample of caregivers assessed, nearly half (47.5%) had spoken with family or friends about institutionalisation, 30.6% had consulted with professionals, 26.4% had the names of some prospective residences, 18.6% had called a residence, 24% had visited a residence themselves, 12% had taken their relative to visit a residence and 17.8% had applied for admission in writing.
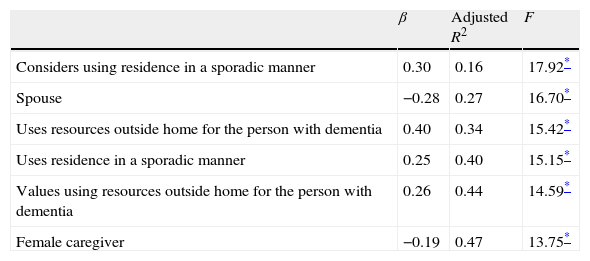
The results of regression analysis designed to assess the variables contributing to the desire for institutionalisation (Table 3) indicated that being male, having a kinship other than spouse with the patient and having evaluated and made sporadic use of both residences and other formal resources (day centres and psychostimulation) accounted for 47% of the variance of the final desire to institutionalise a relative with dementia.
Stepwise multiple regression of desire for institutionalisation.
| β | Adjusted R2 | F | |
| Considers using residence in a sporadic manner | 0.30 | 0.16 | 17.92* |
| Spouse | −0.28 | 0.27 | 16.70* |
| Uses resources outside home for the person with dementia | 0.40 | 0.34 | 15.42* |
| Uses residence in a sporadic manner | 0.25 | 0.40 | 15.15* |
| Values using resources outside home for the person with dementia | 0.26 | 0.44 | 14.59* |
| Female caregiver | −0.19 | 0.47 | 13.75* |
The institutionalisation of a relative is a complicated situation for the whole family and should not be considered an easy decision or a specific or accidental event, but rather as a process in which caregivers weigh the benefits and drawbacks of a very difficult decision to make. The present study suggests that the caregivers of people with dementia most likely to consider the possibility of institutionalising their relatives are male, not married to the patient, and when they have considered the possibility of using other formal resources, or indeed have already begun to use them.
Surprisingly, the stressor factors included in the study did not play a relevant role in the desire for institutionalisation. It appears that the institutionalisation of the person with dementia might be decided regardless of the time period they have been cared for, the daily hours devoted to care, their level of dependence or behavioural or memory problems, or the effects that this has on the health of caregivers. Not even important elements in the desire for institutionalisation, such as incontinence or need for assistance in various activities of daily living (as measured by the Barthel index) or behavioural and memory disorders (as measured by the LPMC-R), which manifest the level of severity of dementia, were associated with the desire for institutionalisation. None of these stressor elements was significantly associated with the desire for institutionalisation in this study. In fact, as found in other studies,7 institutionalisation can be decided relatively early in the course of the disease. In this situation, caregivers do not dedicate much time to care and do not suffer from numerous problems, but already contemplate institutionalising their relatives before it becomes even more difficult. In this sense, neither the subjective assessment of the situation nor the personal resources of the caregiver appear to play an important role in the desire for institutionalisation. Thus, it seems that contemplating the institutionalisation of a relative is not directly related to the stress suffered by caregivers or to fundamental mediating variables, such as the subjective assessment of these stressors.
In addition, our study result revealed that, contrary to the hypothesis, familism is not associated with the desire for institutionalisation. It does not seem that, within our sociocultural context, caregivers with greater familism refuse to contemplate the possibility of institutionalising a relative to a greater extent. It appears that familism affects other elements of the caregiver stress process, rather than the consequences of care, such as the desire for institutionalisation.12 In fact, a study conducted with Korean caregivers found that greater emphasis placed on their cultural values associated with caring and respect for elders was not associated with less use of formal services.27 The absence of a direct relationship between familism and the desire for institutionalisation could also be due to the fact that these cultural values exert an indirect influence (mediator or moderator) on institutionalisation, rather than a direct influence, such as that analysed in this study.
In previous studies, caregiver gender was not associated with the desire for institutionalisation but did predict true institutionalisation of people with dementia.4,8 Perhaps females tend to recognise less the desire to institutionalise their relatives, experience greater social pressure, feel more obligated to continue to provide care regardless of all other considerations and only turn to institutionalisation as a last resort. Morycz9 and Rivera et al10 suggest that women feel guilty about merely considering that they are unable to care for their relatives, which would explain their reluctance to consider institutionalisation.
Something similar happens in the case of spouses, who generally have a stronger bond with the person with dementia than other relatives. Spouses feel a strong obligation to continue to care, regardless of other factors that could be taken into consideration such as the effect of this care on their own health, social and family life or the health of patients themselves. The mere fact of contemplating institutionalising a spouse with dementia can be interpreted by caregivers as a failure and neglect of their duties, thus preventing this alternative from even being considered.28
Therefore, we can hypothesise that both females and males are reluctant to consider the institutionalisation of their spouses; that for these caregivers admitting the patient to a residence is either not an option or would be the last resort, probably due to considering it a failure in their marital obligations.
The more the use of formal resources outside the home is valued, the greater the desire for institutionalisation. Recognising the possibility of needing formal help that involves moving the relative outside the home facilitates consideration of the possibility of institutionalisation. Once the “barrier” of thinking that the caregiver can do everything has been overcome and it is believed that there are other possibilities outside the home, then all possible alternatives are contemplated, including institutionalisation.
Apart from having a positive opinion of institutions, making use these formal resources outside the home is also associated with an increased desire to institutionalise. Once the benefits of formal services have been experienced and initial fears have been allayed, it becomes easier for caregivers to consider permanent care for their relatives outside their homes as appropriate.4 Very often, formal services are used in crisis situations, as a resource while waiting to access a residence. In fact, the use of these formal resources can accelerate the institutionalisation of relatives, when a professional considers home care to be unsustainable and recommends admission into a residence.8 If caregivers wait too long to use formal services, delaying their use until there is no other choice, such services then become a transition to institutionalisation rather than a respite service.3
Several limitations should be taken into account when interpreting the results of this study. Firstly, the results are from caregivers who have been approached mainly through social services or health centres and, therefore, cannot be extrapolated to caregivers who are not in contact with such centres. Secondly, as a cross-sectional study, no causal inference can be contemplated in the relationships found. Longitudinal studies would be required to analyse more precisely the factors that explain the intention of institutionalising relatives. It should also be noted that the percentages of explained variance are not very high. However, 47% of variance explained with the variables in this study is higher than the variance explained in previous studies, ranging between 19% and 38%.6,7,9
After presenting the main contributions and limitations of the study, we consider it important to emphasise, in line with other authors,8,9 the idea that interventions aimed at caregivers should not focus primarily on preventing the institutionalisation of people with dementia. Sometimes, institutionalisation is the best solution for both patients and their families. Interventions taking into special consideration spouses of caregivers could help them to contemplate admission into residences when this seems appropriate. Thus, institutionalisation would seem appropriate for those individuals who suffer more advanced stages of dementia. On the one hand, their care at home is stressful and often deteriorates the physical and emotional well-being of both caregivers and patients. On the other hand, it puts at risk the viability of care for the relatives being served.
FinancingThe preparation of this study was partially funded by the Ministries of Education and Science (SEJ2006-02489/PSIC) and Science and Innovation (PSI2009-08132/PSIC).
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: López J, et al. Factores asociados a la consideración de ingresar a un familiar con demencia en una residencia. Neurología. 2011;27:83–9.