To study the influence of various factors on the health-related quality of life (HRQoL) of patients who have suffered a brain infarction (BI), with special attention to psychopathological disorders (PD).
Patients and methodsProspective observational study on 45 patients admitted due to a BI, evaluated at 4, 12 and 26 weeks of the acute event. Social and demographic data, and medical history were collected; the SF-36 scale was used for the assessment of HRQoL, and the Neuropsychiatric Inventory (NPI), MMSE, Canadian Neurological Scale, Modified Rankin Scale and other instruments for assessing psychopathological, cognitive, neurological and functional status. A linear regression analysis was performed to identify potential predictors of the SF-36 scores at 26 weeks, introducing, as independent variables, medical and psychiatric history, demographic characteristics and the functional, neuropsychological and psychopathological assessments at 4 weeks.
ResultsValid predictive models for all the SF-36 domains were obtained, in which a history of pre-morbid depression, higher scores in the NPI and Rankin Scale, and lowest in the Canadian Neurological Scale were the main predictors of a worse HRQoL in the long term. Psychopathology related caregiver's distress (assessed with the NPI) was associated with a lower score in the social function index.
ConclusionsPDs and functional status were the main determinants of HRQoL in patients with BI.
Estudiar la influencia de diversos factores en la calidad de vida relacionada con la salud (CVRS) de los pacientes tras un infarto cerebral (IC), con especial atención a los trastornos psicopatológicos (TP).
Pacientes y métodosEstudio observacional prospectivo sobre 45 pacientes ingresados por IC, evaluados a las 4, 12 y 26 semanas del evento agudo. Se recogieron antecedentes y datos sociodemográficos previos, se utilizó la escala SF-36 para la valoración de la CVRS, para la valoración psicopatológica, cognitiva, neurológica y funcional se utilizó el inventario neuropsiquiátrico (NPI), MMSE, escala de Canadá, escala de Rankin modificada y otras escalas. Para determinar los posibles factores predictivos de las puntuaciones del SF-36 a las 26 semanas se realizó un estudio de regresión lineal, introduciendo como variables independientes los antecedentes médicos y psiquiátricos, las características sociodemográficas y la evaluación funcional, neuropsicológica y psicopatológica a las 4 semanas.
ResultadosSe obtuvieron modelos predictivos válidos para todos los índices del SF-36, en los que el antecedente de depresión, las puntuaciones más altas en el NPI y la escala de Rankin, y más baja en la escala canadiense fueron los principales indicadores predictivos de una peor CVRS a largo plazo. El distrés del cuidador asociado a la psicopatología del paciente (medido a través del NPI) tuvo una influencia negativa sobre el índice de función social.
ConclusionesLos TP y la situación funcional fueron los principales determinantes de la CVRS de los pacientes tras un IC.
Health-related quality of life (HRQoL) is a key measure to assess the real impact of a disease on individuals. Cerebral stroke (CS) is an acute and severe neurological disorder that can result in sensory-motor, cognitive and psychopathological deficits that, along with the personal and social circumstances of patients, will determine their HRQoL.1
The measurement of HRQoL is complex because it is influenced by aspects such as previous experiences, expectations, beliefs and subjective perceptions. However, there is a consensus that at least 4 dimensions should be assessed: physical (physical symptoms), functional (basic and instrumental activities), psychological (cognitive and emotional function, life satisfaction, perceived health) and social (interaction of the subject with the environment).2 The Short Form 36 (SF-36)3 health survey is a generic instrument that covers all these aspects and is widely used for the study of HRQoL in stroke. In addition, its dissemination among the scientific community makes it possible to compare its results.
Previous studies have linked HRQoL of stroke patients with multiple factors, including the characteristics of the CS (location, extent or aetiology),4–6 post-stroke depression,7–9 cognitive impairment (CI)4,6–10 and the coping strategies employed by patients.11 However, in most studies the most determining factor for HRQoL is the functional status of patients.5,9,12–14
There are few studies that analyse the combined influence on HRQoL of the different areas affected after stroke (cognitive, sensory-motor, functional and psychopathological) or how to predict the long-term evolution of HRQoL from the history and clinical status of a patient.15 Regarding psychopathological disorders (PD), most studies that have addressed this issue have focused on affective disorders, mainly depression.7,8,13 While this is undoubtedly the most common PD in stroke patients, others such as apathy16 are also frequent and greatly influence post-stroke recovery. Moreover, how global psychopathological status affects HRQoL has not been studied. Finally, most HRQoL studies in stroke patients group the cases with different types of stroke, including cerebral strokes and haemorrhages, and even transient ischaemic attacks,13 despite their having different prognoses.17
The objectives of this study were to analyse the evolution of HRQoL in the 6 months following a CS, as well as to detect potential predictive indicators of HRQoL at 26 weeks after a vascular event, taking as a reference the history, location of CS and functional, cognitive and psychopathological status of each patient at 4 weeks following the stroke.
Patients and methodsParticipantsA prospective study was conducted on a sample of 45 Caucasian patients consecutively admitted at the neurology unit of our hospital for probable ischaemic stroke. Patients were evaluated at 4 different times: upon admission and at 4, 12 and 26 weeks after the event. Patients were recruited between May 2007 and December 2008 from a sample of 55 patients included in a study of PD in CS,18 of which 45 patients did not meet any of the exclusion criteria.
Inclusion/exclusion criteriaWe included all consecutive patients with CS – with or without haemorrhagic transformation – who had a caregiver in charge, agreed to participate in the study and who did not meet any of the following exclusion criteria: cerebral haemorrhage or suspicion of another process as cause of the brain lesion (tumour or other); transient ischaemic attack; state of coma or severe alteration of consciousness after 4 weeks following the stroke; death during the first 26 weeks after the stroke; absence of ischaemic vascular lesions identifiable in imaging tests 4 weeks after the stroke; emergence of a new brain lesion before 26 weeks of the stroke (recurrence of CS, cerebral haemorrhage or traumatic brain injury); history of dementia or suspected CI prior to stroke; and inability to answer the HRQoL questionnaire or conduct neuropsychological testing, in the opinion of the examiner, due to suffering severe hearing and/or visual impairment, being illiterate or suffering post-stroke CI or aphasia, both in a severe degree.
InstrumentsWe used the following assessment instruments: (a) data collection questionnaire: clinical (medical and psychiatric history), demographic and social variables; (b) cognitive assessment: Mini-Mental State Examination (MMSE),19 Frontal Assessment Battery (FAB),20 informer test21; (c) psychopathological assessment: Neuropsychiatric Inventory (NPI),22 Hamilton depression23 and anxiety24 scales; (d) functional and neurological assessment: modified Rankin scale,25 Barthel index,26 Lawton index27 and Canadian neurological scale,28 and (e) assessment of HRQoL: SF-36,3 from which scores were obtained for each of the 8 indices (physical function, physical role, pain, general health, vitality, social function, emotional role, mental health), as well as the summary scores of the physical and mental components. The score range in each of these sections went from 0 to 100, with 100 being the best. The physical component grouped scores in indices of physical function, physical role, pain and general health, whereas the mental component grouped the remaining indices.
ProceduresAt the time of admission, we assessed the inclusion and exclusion criteria and also requested informed consent from the patient or family. Within 48 h following the stroke, the caregiver was administered the data collection questionnaire, NPI, informer test (to rule out previous CI and avoid including patients with psychopathology associated to neurodegenerative diseases, which could have introduced bias in the study) and Barthel and Lawton indices. All cognitive, psychopathological and functional tests referred to in the Instruments section were applied at 4, 12 and 26 weeks of the event.
We used computed tomography or cerebral magnetic resonance to locate the CS. Strokes were defined as right cerebral hemispheric, left cerebral hemispheric or located in the brainstem-cerebellum, indicating whether they were lacunar strokes or not in the case of cerebral hemispheric strokes. The clinical diagnosis and radiological location of CS were established by a neurologist and a radiologist, respectively.
Statistical analysisData were analysed using SPSS v11.0. We conducted: (a) descriptive analysis through frequency distribution and summary statistics, (b) study of mean difference through Student's t test, (c) correlation study using the Pearson correlation coefficient and (d) multivariate analysis through linear regression analysis. Qualitative variables were recorded as dummy variables for their inclusion in the different models. We established a statistical significance level of 0.05.
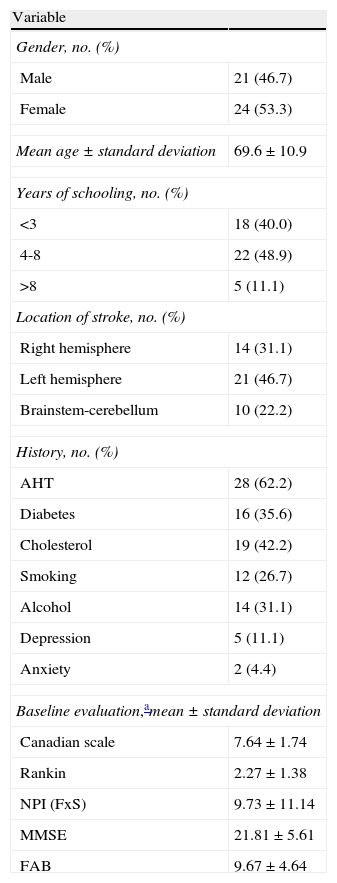
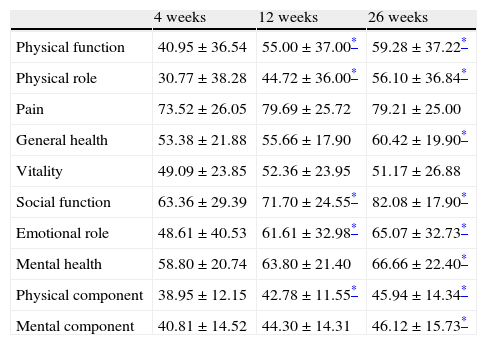
ResultsDescriptive dataTable 1 shows the descriptive data (demographic and clinical) from the sample. Table 2 shows the analysis of mean difference between the SF-36 scores at 4, 12 and 26 weeks. Taking week 4 as a reference, there was a significant improvement (P<.05) at week 12 in the indices for physical function, physical role, social function, emotional role and the physical component, and at 26 weeks in the indices for physical function, physical role, general health, social function, emotional role, mental health, physical component and mental component. When assessing the differences in mean scores between weeks 12 and 26, we found statistically significant differences (P<.05) only in the physical role, general health and social function variables.
Demographic and clinical characteristics of the sample (n=45).
| Variable | |
| Gender, no. (%) | |
| Male | 21 (46.7) |
| Female | 24 (53.3) |
| Mean age±standard deviation | 69.6±10.9 |
| Years of schooling, no. (%) | |
| <3 | 18 (40.0) |
| 4-8 | 22 (48.9) |
| >8 | 5 (11.1) |
| Location of stroke, no. (%) | |
| Right hemisphere | 14 (31.1) |
| Left hemisphere | 21 (46.7) |
| Brainstem-cerebellum | 10 (22.2) |
| History, no. (%) | |
| AHT | 28 (62.2) |
| Diabetes | 16 (35.6) |
| Cholesterol | 19 (42.2) |
| Smoking | 12 (26.7) |
| Alcohol | 14 (31.1) |
| Depression | 5 (11.1) |
| Anxiety | 2 (4.4) |
| Baseline evaluation,amean±standard deviation | |
| Canadian scale | 7.64±1.74 |
| Rankin | 2.27±1.38 |
| NPI (FxS) | 9.73±11.14 |
| MMSE | 21.81±5.61 |
| FAB | 9.67±4.64 |
AHT, arterial hypertension; FAB, frontal assessment battery; FxS, global NPI score (frequency times severity); MMSE, Mini-mental State Examination; NPI, neuropsychiatric inventory.
Scores obtained in the different domains of the SF-36 at 4, 12 and 26 weeks of stroke (n=45).
| 4 weeks | 12 weeks | 26 weeks | |
| Physical function | 40.95±36.54 | 55.00±37.00* | 59.28±37.22* |
| Physical role | 30.77±38.28 | 44.72±36.00* | 56.10±36.84* |
| Pain | 73.52±26.05 | 79.69±25.72 | 79.21±25.00 |
| General health | 53.38±21.88 | 55.66±17.90 | 60.42±19.90* |
| Vitality | 49.09±23.85 | 52.36±23.95 | 51.17±26.88 |
| Social function | 63.36±29.39 | 71.70±24.55* | 82.08±17.90* |
| Emotional role | 48.61±40.53 | 61.61±32.98* | 65.07±32.73* |
| Mental health | 58.80±20.74 | 63.80±21.40 | 66.66±22.40* |
| Physical component | 38.95±12.15 | 42.78±11.55* | 45.94±14.34* |
| Mental component | 40.81±14.52 | 44.30±14.31 | 46.12±15.73* |
Values expressed as mean score±standard deviation.
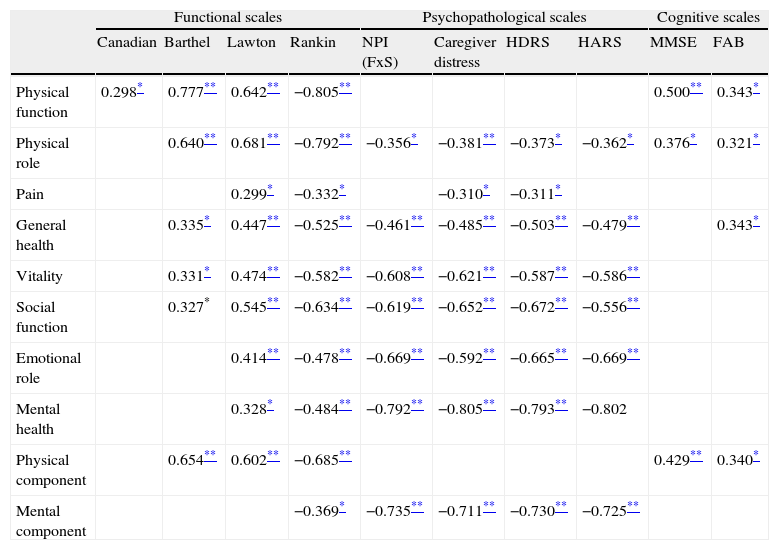
Table 3 shows the correlations at 26 weeks of the CS between the scores of the SF-36 scale and the functional, psychopathological and cognitive scales. Overall, we observed moderate or high correlation with the functional and psychopathological scales and low or moderate correlation with the cognitive scale.
Correlation between the SF-36 quality of life indices and the scores obtained in functional, psychopathological and cognitive scales (n=45).
| Functional scales | Psychopathological scales | Cognitive scales | ||||||||
| Canadian | Barthel | Lawton | Rankin | NPI (FxS) | Caregiver distress | HDRS | HARS | MMSE | FAB | |
| Physical function | 0.298* | 0.777** | 0.642** | −0.805** | 0.500** | 0.343* | ||||
| Physical role | 0.640** | 0.681** | −0.792** | −0.356* | −0.381** | −0.373* | −0.362* | 0.376* | 0.321* | |
| Pain | 0.299* | −0.332* | −0.310* | −0.311* | ||||||
| General health | 0.335* | 0.447** | −0.525** | −0.461** | −0.485** | −0.503** | −0.479** | 0.343* | ||
| Vitality | 0.331* | 0.474** | −0.582** | −0.608** | −0.621** | −0.587** | −0.586** | |||
| Social function | 0.327* | 0.545** | −0.634** | −0.619** | −0.652** | −0.672** | −0.556** | |||
| Emotional role | 0.414** | −0.478** | −0.669** | −0.592** | −0.665** | −0.669** | ||||
| Mental health | 0.328* | −0.484** | −0.792** | −0.805** | −0.793** | −0.802 | ||||
| Physical component | 0.654** | 0.602** | −0.685** | 0.429** | 0.340* | |||||
| Mental component | −0.369* | −0.735** | −0.711** | −0.730** | −0.725** | |||||
Values expressed as Pearson correlation coefficient. Non-significant values are not shown.
FAB, frontal assessment battery; FxS, global NPI score (frequency times severity); HARS, Hamilton anxiety rating scale; HDRS, Hamilton depression rating scale; MMSE, Mini-mental State Examination; NPI, neuropsychiatric inventory.
More specifically, the study of the relationship between neurological and functional scales with the different indices of the HRQoL showed high correlation of the functional scale with the HRQoL physical indices and low or moderate correlation with mental indices. The Rankin scale was significantly correlated with all SF-36 indices.
With regard to psychopathological variables, we observed moderate or high correlation with the mental and social aspects of HRQoL, and low or moderate correlation with the physical aspects. The global NPI score – frequency times severity (FxS) – and the Hamilton depression and anxiety scales were the most related variables. The subscales of depression, apathy and anxiety in the NPI also presented low to moderate correlations with the HRQoL indices (data not shown in Table 3). Similarly, we observed moderate or high correlation between caregiver distress associated with PD (NPI) and mental HRQoL indices.
Finally, the cognitive scales were correlated with a lower number of SF-36 indices. There was moderate correlation of the MMSE with the physical function scale and physical component, as well as low correlations of the FAB with the physical component and 3 of the physical indices in the SF-36 (physical function, physical role and general health). Neither scale presented a significant correlation with the mental HRQoL indices.
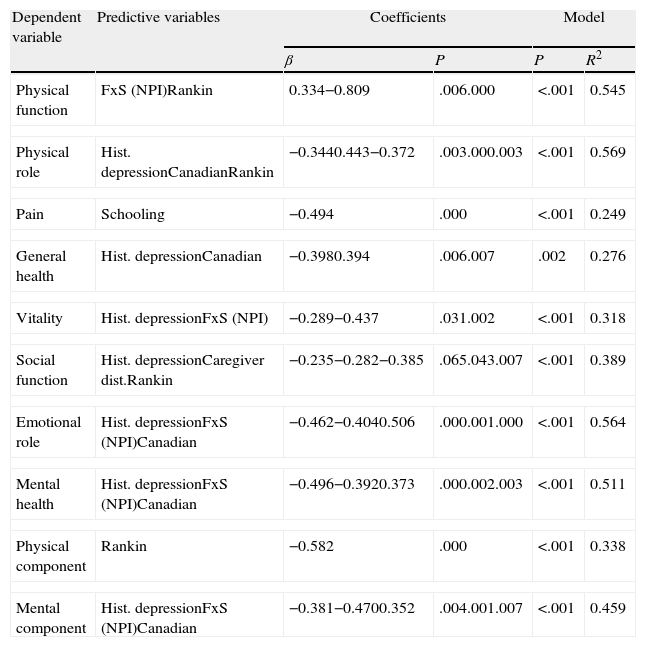
Predictive factors for quality of lifeWe used stepwise linear regression analysis to obtain predictive indicators of different HRQoL indices at 26 weeks of the CS, taking as reference the condition of each patient at 4 weeks. As dependent variables we included the SF-36 scores at 26 weeks and, as independent or predictor variables, we included: demographic background (age, gender and years of schooling), medical history (arterial hypertension, hypercholesterolaemia, diabetes, alcohol, tobacco), psychopathological history (depression, anxiety), location of the stroke, the scores obtained at 4 weeks in the MMSE, overall NPI score (FxS) and its various subscales, and the Canadian and Rankin scales.
We obtained valid predictive models for all indices and components of the SF-36 (Table 4). A history of depression was the predictor variable that appeared in the most models: physical role, general health, vitality, social function, emotional role, mental health and mental component. Other predictor variables present in several models were: the highest score on the NPI and Rankin scales, and the lowest score in the Canadian neurological scale at 4 weeks. Predictive models explained between 24% and 56% of the variance of the different variables studied. The scores of the NPI and Canadian neurological scales at 4 weeks, along with a history of depression, accounted for over 50% of the variance in the indices of mental health and emotional role, as well as 45% of the variance of the mental component at 26 weeks.
Regression models for SF-36 quality of life indices (n=45).
| Dependent variable | Predictive variables | Coefficients | Model | ||
| β | P | P | R2 | ||
| Physical function | FxS (NPI)Rankin | 0.334−0.809 | .006.000 | <.001 | 0.545 |
| Physical role | Hist. depressionCanadianRankin | −0.3440.443−0.372 | .003.000.003 | <.001 | 0.569 |
| Pain | Schooling | −0.494 | .000 | <.001 | 0.249 |
| General health | Hist. depressionCanadian | −0.3980.394 | .006.007 | .002 | 0.276 |
| Vitality | Hist. depressionFxS (NPI) | −0.289−0.437 | .031.002 | <.001 | 0.318 |
| Social function | Hist. depressionCaregiver dist.Rankin | −0.235−0.282−0.385 | .065.043.007 | <.001 | 0.389 |
| Emotional role | Hist. depressionFxS (NPI)Canadian | −0.462−0.4040.506 | .000.001.000 | <.001 | 0.564 |
| Mental health | Hist. depressionFxS (NPI)Canadian | −0.496−0.3920.373 | .000.002.003 | <.001 | 0.511 |
| Physical component | Rankin | −0.582 | .000 | <.001 | 0.338 |
| Mental component | Hist. depressionFxS (NPI)Canadian | −0.381−0.4700.352 | .004.001.007 | <.001 | 0.459 |
Caregiver dist., caregiver distress; FxS, global NPI score (frequency times severity); Hist. depression, history of depression; NPI, neuropsychiatric inventory.
In this study we analysed the evolution of different HRQoL indices after CS and evaluated the influence of the various areas of involvement (sensory-motor, cognitive, psychopathological and functional) on HRQoL. Our results confirm the importance of PD in the HRQoL of patients who have suffered CS, as well as the fact that it is possible to predict, to some extent, long-term HRQoL by observing the history of each patient and their condition at 4 weeks after the stroke. This will allow for more accurate planning of the care that these patients should receive.
The evolutionary study of HRQoL revealed a significant improvement in most scales between 4 and 26 weeks after the CS, with the exception of the pain and vitality scales. This HRQoL improvement in the first 6 months of evolution was also reported by Rønning and Stavem.15
The analysis of correlations between the different HRQoL indices studied and the neurological, functional, psychopathological and cognitive variables at 26 weeks of the CS indicated that HRQoL perception was related, firstly, to functional impairment, and secondly, to PD, especially depression and anxiety. In this respect, caregiver distress in relation to the psychopathological condition of the patient (as assessed by the NPI scale) was also important. Finally, in this study CI was the factor showing the lowest degree of correlation with HRQoL. In addition, we noted that there was a correlation between the cognitive scales and the physical indices of the SF-36, but not with the mental indices. All these aspects have also been linked in other HRQoL studies, although the order of importance of each factor varies according to different authors.1,13
Linear regression analysis obtained valid predictive models for all scales in the SF-36. Among these, neurological and functional status at 4 weeks, history of depression and post-stroke psychopathology at 4 weeks, as assessed by the NPI scale, were the main predictive indicators of HRQoL at 26 weeks of the CS.
More detailed analysis of the different predictive models revealed some especially significant findings. Firstly, the main predictive factors of a poor HRQoL perceived in relation to physical aspects at 26 weeks of the CS were a history of depression and, above all, the degree of disability at 4 weeks, with the score on the Rankin scale being the only predictor of physical component. On the other hand, HRQoL associated with mental health could be predicted by a history of depression, along with neurological status (Canadian neurological scale) and psychopathological status (FxS) at 4 weeks. In this analysis, we could not demonstrate that factors such as age, gender or CS location influenced HRQoL independently, although other authors have reported worse outcomes in patients with more advanced age,6,8 females1,4 or those with lesions in the left hemisphere.6
It is noteworthy that a history of depression was the most frequent independent factor in the predictive models (7 of 10). This datum is easily obtainable during first contact with patients through their clinical histories.
On the other hand, a higher level of education emerged as a predictor of poorer evaluation of quality of life related to pain in our patients. This finding contradicts previous literature, since this factor is generally associated with a more positive perception of HRQoL.29
Finally, caregiver distress associated with psychopathological condition (as assessed by the NPI scale) predicted a worse score on the social function component. This expresses the interference that PD represents in the relationship between patients and their family and social environment. This finding was consistent with those reported in the study by Haley et al.,30 in which affective disorders of stroke patients were considered by their caregivers as the most stressful problem for themselves, even above the level of disability or other factors.
Among the limitations of our study, we include the small number of cases in the sample and the fact that, due to the instruments selected, we could not include illiterate patients or those with severe CI or aphasia. We cannot rule out the possibility that this fact has influenced the results, especially in the absence of a relationship of HRQoL with left hemispheric location or CI. In addition, although it is a useful test for the detection of moderate to severe post-stroke CI, the MMSE may be unsuitable for the assessment of low level CI.31 Finally, another limitation of the study was not addressing other factors that may be associated with HRQoL after stroke, such as coping strategies and the degree of social support.1,6,11,32
In conclusion, according to the data obtained in this study, patients with worse functional and psychopathological status 1 month after suffering a CS have an increased risk of presenting poorer perceived HRQoL at 6 months of the stroke. The functional status influences both physical and mental aspects of HRQoL. A history of depression and post-stroke PD influence aspects of HRQoL linked with mental health and also, although to a lesser extent, with physical condition.
The results of this study were presented at the 62nd Annual Meeting of the Spanish Society of Neurology (Barcelona, 16–20 November 2010).
Please cite this article as: Castellanos Pinedo F, et al. Trastornos psicopatológicos y calidad de vida en el infarto cerebral. Neurología. 2011; 27:76–82.