Dermatophytoses in children are common pathologies worldwide caused mainly by Trichophyton rubrum. However, due to the globalization and the atypical pets that people nowadays own, some zoonotic species are also involved in these lesions.
Case reportWe present two cases of tinea faciei caused by the zoonotic mould Trichophyton erinacei in two children that owned a guinea pig and a hedgehog, respectively. Mycological diagnosis was performed inoculating skin scales on Sabouraud-glucose agar plates supplemented with chloramphenicol, with and without gentamicin, and on Sabouraud-glucose agar tubes, with and without cycloheximide. Microscopical examination in both cases and ITS region sequencing to confirm the identification (performed in one of them) were compatible with T. erinacei. Multiple treatments like corticosteroids and antibiotics were prescribed prior to the accurate diagnosis. Finally, both patients received topical and oral terbinafine, respectively, the lesions being resolved entirely.
ConclusionsZoonotic fungi must be considered in the diagnosis of skin lesions. An accurate medical record, with a guided anamnesis about possible risk factors and an ongoing and open dialogue between health professionals, are essential to improve both the management of these exotic and zoophilic dermatophytoses.
Las dermatofitosis son patologías comunes en niños y son causadas principalmente por Trichophyton rubrum. Sin embargo, debido a la globalización y a la presencia cada vez más frecuente de animales exóticos como mascotas, algunas especies zoonóticas menos habituales pueden convertirse en agentes causales.
Caso clínicoNuestro objetivo es describir dos casos de Tinea faciei causados por Trichophyton erinacei en dos niños que poseían, respectivamente, una cobaya y un erizo como mascotas. Se tomó muestra de escamas cutáneas que fueron inoculadas en placas de agar Sabouraud-glucosa suplementado con cloranfenicol, con y sin gentamicina, y en tubos de agar Sabouraud-glucosa con y sin cicloheximida. El examen microscópico fue compatible con Trichophyton erinacei, cuya identificación pudo ser confirmada por secuenciación de la región ITS en uno de los casos. Antes del correcto diagnóstico los pacientes habían recibido múltiples tratamientos (corticosteroides, antibióticos). Finalmente, los dos pacientes recibieron terbinafina tópica y oral, respectivamente, lo que llevó a la resolución completa de las lesiones.
ConclusionesLos hongos zoonóticos deben ser considerados en el diagnóstico diferencial de las lesiones cutáneas. Una historia clínica con anamnesis guiada sobre posibles factores de riesgo, junto con una comunicación multidisciplinar fluida, es indispensable para mejorar el manejo de estas dermatofitosis.
Traditionally, dogs and cats have been the most popular household pets, but this reality has completely changed in the last decades.8 Exotic animals have become trendy pets, and this fact has also modified the zoonotic pathologies that we find in our patients. We present two cases of tinea in children that own a guinea pig and a hedgehog, respectively.
Case 1: A five-year-old girl with a history of atopic dermatitis was attended due to a 3 month-itching lesion in the left malar area. Initially, topical corticosteroids were prescribed, without any improvement. Afterwards, itraconazole and a topical betamethasone-clotrimazole combined therapy were prescribed based on the fact that the family had a guinea pig at home. When itraconazole was stopped, skin lesions worsened and the patient needed again medical attention. The direct examination showed erythematous and scaly plaques with an active edge on the left cheek and periocular area. A tinea corporis was suspected and lesions healed after 8 weeks with terbinafine and topical clotrimazole treatment.
Case 2: A nine-year-old boy presented with a two-week history of itching lesions on the temple and upper left eyelid. In physical examination a well-defined erythematous plaque with active edges and marked fine desquamation, with some 1-2 millimeters pustules, was observed (Figure 1). Due to the clinical suspicion of tinea faciei the mother was asked about pets, saying that they had a hedgehog that the kid regularly touched and got close to his face. Topical terbinafine was prescribed for 4 months and lesions improved.
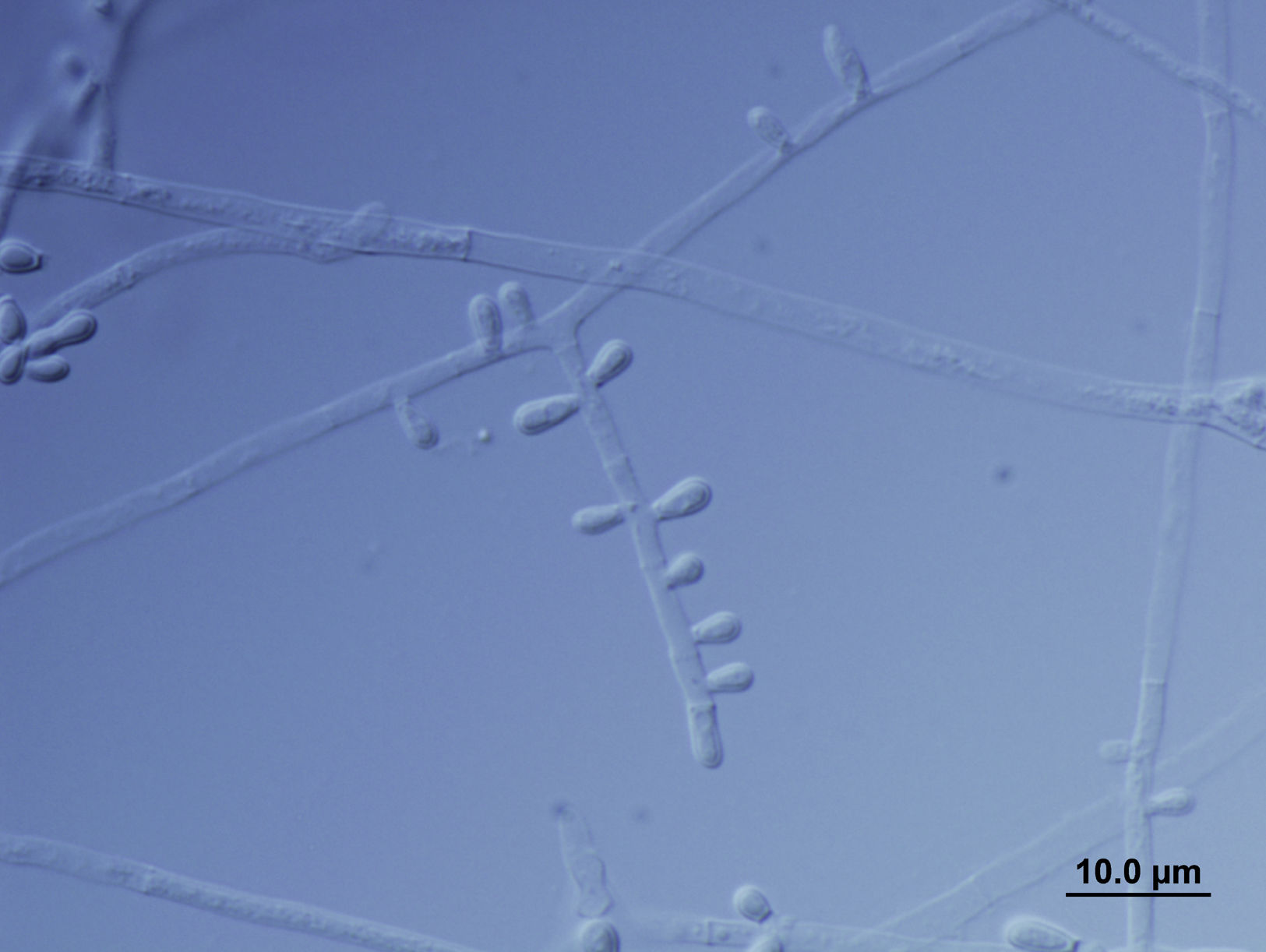
In both cases samples were inoculated on Sabouraud-glucose agar plates supplemented with chloramphenicol with and without gentamicin, and on Sabouraud glucose agar tubes with and without cycloheximide. Cultures yielded numerous white powdery colonies with yellow to brown reverse. Complementary microscopical findings were compatible with Trichophyton erinacei (Figure 2). In the second case, morphological identification was further confirmed by ITS1-5.8S-ITS2 rRNA gene sequencing. A search on the GenBank database revealed a 100% match with T. erinacei type strain ATCC 28443. This sequence was deposited at NCBI with the accession number MN807946.
Dermatophytosis is prevalent worldwide, being Trichophyton rubrum the most frequent agent involved. Due to social, cultural and globalization changes, there are less prevalent etiological agents that should be considered in clinical practice. T. erinacei is a zoophilic dermatophyte that is currently emerging as a human pathogen, causing a severe inflammatory and pruritic infection. Hedgehogs are relatively often infected or colonized by this species in our country.1 In recent years, some tinea corporis cases have been reported related to hedgehogs, mainly in Asia,2,4,7 other European countries 5,6 and only one case linked to a guinea pig in Spain.3 As far as we know, the carriage of T. erinacei is uncommon, and due to the similarity with Trichophyton benhamiae sequencing is mandatory to confirm the identification. Unfortunately, as in Duran-Valle et al. case,3 our first isolate was not sequenced. The morphological resemblance between T. benhamiae and T. erinacei makes T. erinacei a suspected etiology, but the possibility of a T. benhamiae related to guinea pigs is also plausible. A guided interview revealed that the pet cage was previously used for housing a hedgehog, explaining the guinea pig infection and patient's lesions.
A long-term combination of topical and systemic antifungal therapy is usually required to treat this infection. Both patients received oral and topical terbinafine, respectively, and lesions resolved entirely. Success rates for this therapy have reached 75 to 90% in tinea corporis.9 An accurate medical record, with a guided anamnesis about possible risk factors and an ongoing and open dialogue between microbiologists and clinicians are essential to improve both patients’ care and the management of these exotic and zoophilic dermatophytoses.
Funding informationNo funding was received for this study
We would like to thank our laboratory technicians M. Alcaide and V. Barragán for their collaboration in sample processing.