Description and analysis of the relation between the proximal humerus fracture patterns and the traumatic injury of the axillary nerve.
Material and methodProspective, observational study of a consecutive case series that analysed proximal humerus fractures. Radiographic evaluation was performed, and AO (Arbeitsgemeinshaft für Osteosynsthesefragen) system was used to classify the fractures. Electromyography was used to diagnose the axillary nerve injury.
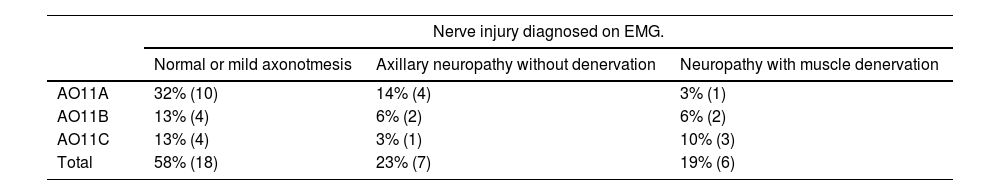
ResultsThirty-one patients on 105 who had a proximal humerus fracture met inclusion criteria. Eighty-six percent of the patients included were women and 14% men. The mean age was 71.8 years (30–96 years). Of the patients included in the study, 58% had normal or mild axonotmesis EMG, 23% had axillary nerve neuropathy without muscle denervation and 19% had injury with axillary nerve denervation. Patients who suffered complex fractures of the proximal humerus (AO11B and AO11C) had a higher risk of presenting axillary neuropathy type lesions with muscle denervation in the EMG, this relationship being statistically significant (p<0.001).
ConclusionPatients who have more risk on presenting axillary nerve neuropathy with muscle denervation in electromyography are those who present complex proximal humerus fractures AO11B and AO11C (p<0.001).
Descripción y análisis de la relación entre las fracturas de húmero proximal y la lesión traumática del nervio axilar circunflejo.
Material y métodoEstudio prospectivo y observacional de una serie de casos consecutivos de fracturas de extremo proximal de húmero. Se realizó valoración radiográfica, clasificando las fracturas según el sistema de la Arbeitsgemeinshaft für Osteosynsthesefragen, Asociación de Grupo de Trabajo para el Estudio de la Fijación Interna de las Fracturas (AO) y electromiografía (EMG) para la evaluación de la lesión del nervio axilar.
ResultadosDe 105 casos consecutivos de fracturas de húmero proximal, 31 pacientes cumplían los criterios de inclusión. Se obtuvo una muestra de 86% de mujeres y 14% hombres con edad media de 71,8 años (30-96). De los usuarios incluidos en el estudio, 58% presentó una EMG normal o leve axonotmesis, 23% neuropatía del nervio axilar sin denervación muscular y 19% lesión con denervación del nervio axilar. Aquellos que sufrieron fracturas complejas de húmero proximal (AO11B y AO11C) tuvieron más riesgo de presentar lesiones tipo neuropatía axilar con denervación muscular en la EMG, siendo esta relación estadísticamente significativa (p<0,001).
ConclusionesLos pacientes que sufren fracturas complejas de húmero proximal (AO11B y AO11C) tienen más riesgo de presentar lesiones tipo neuropatía axilar con denervación muscular en la EMG (p<0,001).
Fractures of the proximal end of the humerus account for roughly 6% of adult fractures and are the third most common in patients over the age of 60 years.1 They are common injuries in osteoporotic bone.2 The circumflex nerve is particularly vulnerable in anterior fracture-dislocations, given that its pathway is located on the underside of the capsule and can be injured or lacerated by traction.3
Few studies address the relationship between circumflex nerve injury and fractures of the proximal humerus, and most are retrospective and do not use electromyography (EMG) to assess neurological injury.4–8 Visser et al. studied 143 consecutive cases of proximal humerus fractures following low-energy trauma.9 In this work, they used Neer's classification for proximal humerus fractures and electromyography to assess nerve injury. They detected signs of EMG denervation in 96 patients (67% of the cases). Nerve injury was more frequent in displaced fractures (82%) than non-displaced fractures (59%). All the patients in the series recovered from the nerve injury and consequent loss of muscle strength.
Assuming that nerve injury can play a major role in recovering shoulder function, whether surgical or conservative management has been carried out, we designed a prospective follow-up study of fractures with EMG assessment of the state of the axillary nerve following trauma.
Moreover, we must bear in mind that the intense pain individuals with these fractures suffer is not only due to the nociceptive component of the fracture itself, but also to its common and sometimes severe nerve involvement.10,11 This results in neuropathic pain accompanying these conditions to a greater or lesser extent, which is sometimes difficult to control with standard analgesia.
The aim of this study is to assess circumflex nerve damage in fractures of the proximal end of the humerus by means of a neurophysiological study involving EMG and electroneurogram; and to establish whether there is an association between the pattern of the fracture and the degree of nerve damage.10,11
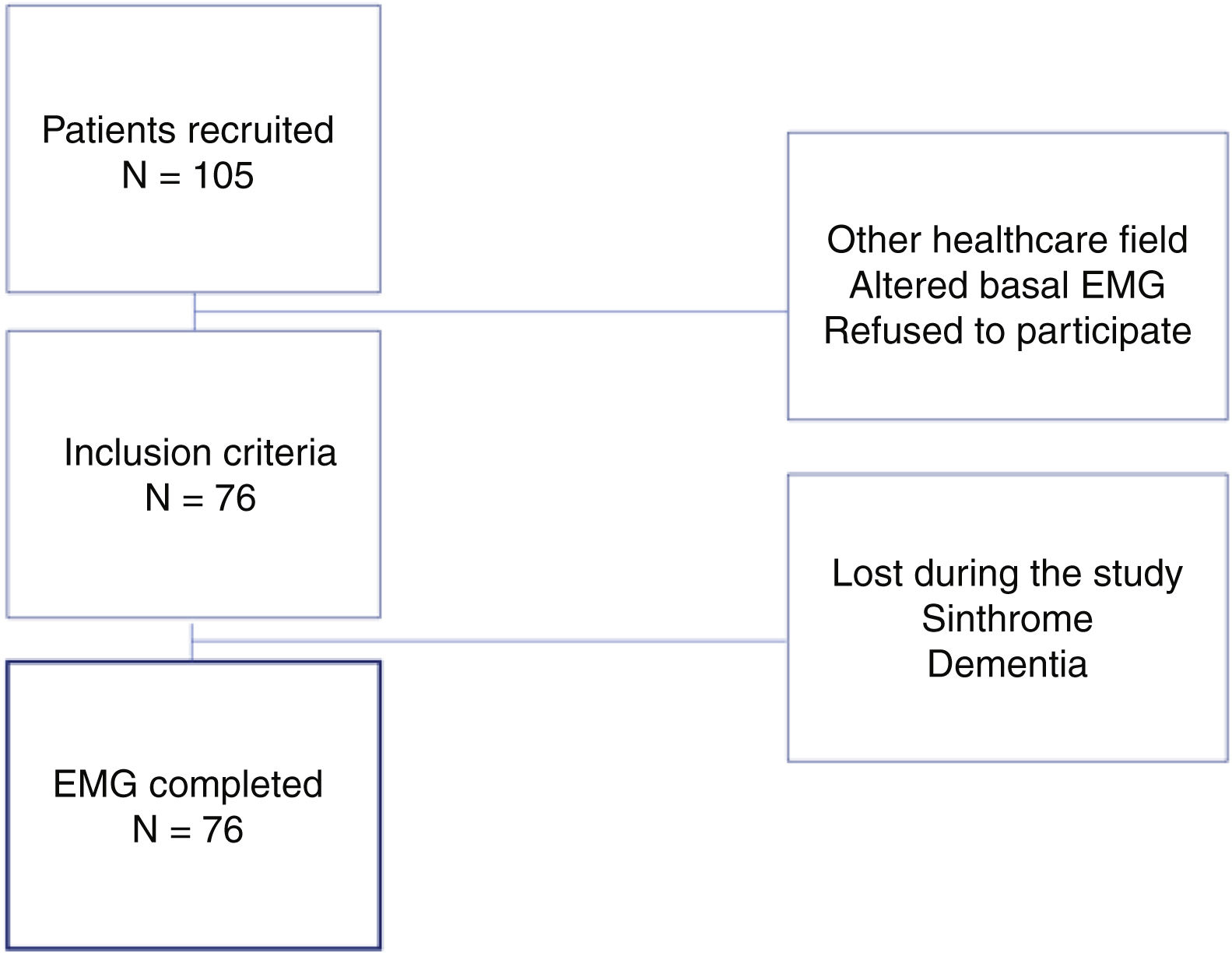
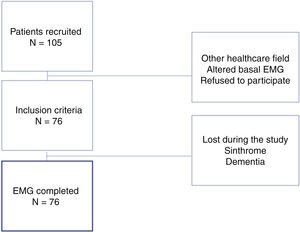
Material and methodThis is a prospective, observational study of a series of consecutive cases: patients who presented to the Emergency Department of our hospital and who were diagnosed with a fracture of the proximal end of the humerus between 1 March and 30 June 2017. The inclusion criteria for the study were: subjects aged 18 years or older, from the reference population of our healthcare district, who exhibited a fracture of the proximal humerus and who voluntarily agreed to participate in the study and to undergo a neurophysiological evaluation (an EMG and electroneurogram) as diagnostic tests in addition to conventional treatment of the fracture; i.e., conservative therapy or surgical intervention. Enrolment in the study did not affect the treatment decision (conservative or surgical); they were treated with the standard treatment that we provide during clinical care. The neurophysiological study was scheduled approximately 20 days after the fracture, as this is regarded as the optimal time for early detection of injury to this nerve with this test. This was done in those cases that received conservative treatment with immobilisation in a sling. The neurophysiological study performed consisted of both an EMG and an electroneurogram. Comparison was made with the contralateral arm as a control. In addition, in cases where axillary nerve injury was noted, the EMG and electroneurogram were repeated at one month as a control. The neurophysiologist who participated in the study is an experienced professional. Exclusion criteria comprised: diseases that could affect the baseline EMG recording (diabetes mellitus [DM], polyneuropathy, myopathy, motor neuron disease, hypothyroidism, or hyperthyroidism), anticoagulant treatments, such as acenocoumarol or warfarin, or advanced dementia as well as other diseases that may hinder the patient's cooperation during the neurophysiological study. Patients with pathological fractures were not included, nor were those who were seen at the Emergency Department of our Hospital, but were followed up at a different centre. Finally, no patients who had previously undergone shoulder surgery were included (Fig. 1).
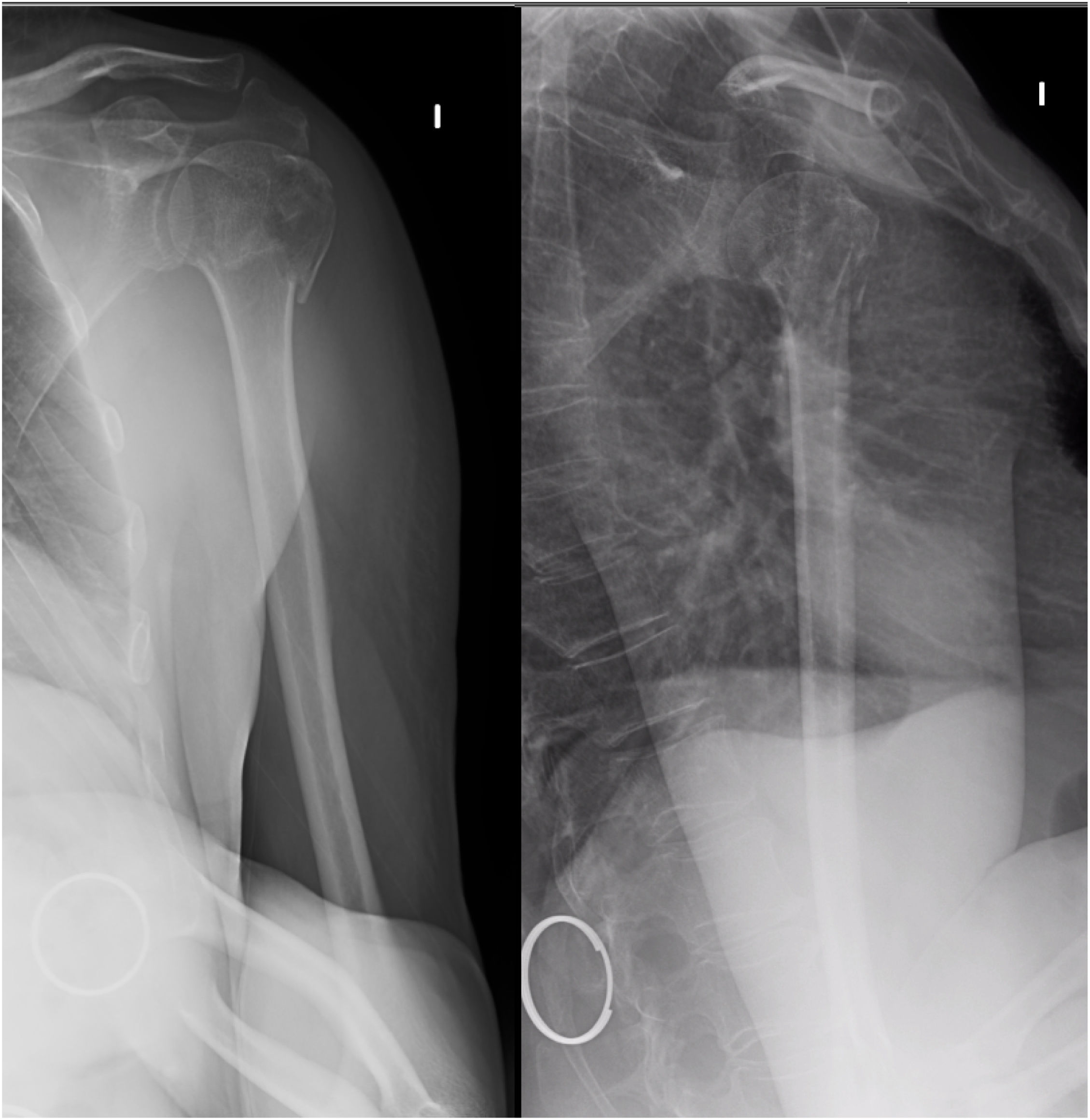
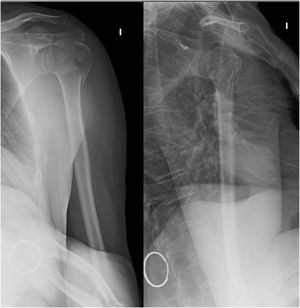
The plain x-rays of each case were reviewed. In those cases in which surgical management was chosen or those in which the plain X-ray raised doubts as to the treatment indication, a computed axial tomography (CT) scan was performed to complete the study.
In those individuals who required surgery and who were also included in the study, a neurophysiological study was performed the day prior to surgery, which is typically six to 15 days after the fall, and another control neurophysiological study was carried out afterwards (21 days after surgery). After consulting with the doctors at the Neurophysiology Department, we came to the conclusion that this was the best way to proceed in these cases, inasmuch as we believe that including surgical cases in this study is also of great interest.
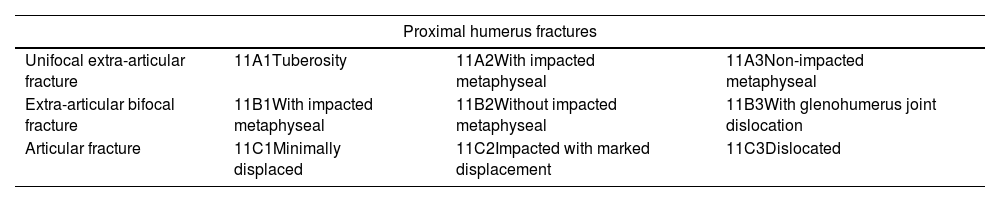
During the initial assessment, the fractures were classified according to the AO classification (Arbeitsgemeinshaft für Osteosynsthesefragen, Association of the Working Group for the Study of Internal Fracture Fixation) as type AO11A, unifocal extra-articular; AO11B, bifocal extra-articular, and AO11C, articular (Fig. 2), and then were then subclassified into the groups of this classification (Table 1).
AO classification of proximal humerus fractures.
| Proximal humerus fractures | |||
|---|---|---|---|
| Unifocal extra-articular fracture | 11A1Tuberosity | 11A2With impacted metaphyseal | 11A3Non-impacted metaphyseal |
| Extra-articular bifocal fracture | 11B1With impacted metaphyseal | 11B2Without impacted metaphyseal | 11B3With glenohumerus joint dislocation |
| Articular fracture | 11C1Minimally displaced | 11C2Impacted with marked displacement | 11C3Dislocated |
AO: Arbeitsgemeinshaft für Osteosynsthesefragen, Association of the Working Group for the Study of Internal Fracture Fixation.
Axillary nerve lesions were categorised using Seddon's classification12 into three groups: normal or mild axonotmesis, axillary neuropathy without muscle denervation, and axillary neuropathy with muscle denervation. The groups were compared on the basis of nerve involvement and fracture type.
We analysed whether there are fracture patterns that can predict nerve damage and its prognosis. We compared the relationship between complex (AO11B and C) and simpler (AO11A) fractures and the nerve damage they presented in the neurophysiological study. Additionally, nerve damage was compared in metaphyseal fractures (AO11A3 and AO11B1-3), owing to the close anatomical relationship of the nerve at this location. The statistical study was performed using Pearson's chi2 on SPSS software. The qualitative variables assessed were, on the one hand, the type of fracture according to the AO classification (Arbeitsgemeinshaft für Osteosynsthesefragen, Association for the Working Group for the Study of Internal Fixation of Fractures); on the other hand, the degree of axillary nerve injury was also evaluated (Table 2). Comparisons by fracture type and degree of injury were made in 2×2 tables. If there were not at least five cases in any of the boxes, a Fisher's exact test was performed.
Results of the EMG in the study population.
| Nerve injury diagnosed on EMG. | |||
|---|---|---|---|
| Normal or mild axonotmesis | Axillary neuropathy without denervation | Neuropathy with muscle denervation | |
| AO11A | 32% (10) | 14% (4) | 3% (1) |
| AO11B | 13% (4) | 6% (2) | 6% (2) |
| AO11C | 13% (4) | 3% (1) | 10% (3) |
| Total | 58% (18) | 23% (7) | 19% (6) |
EMG: electromyography.
Of the 105 consecutive individuals with a diagnosis of proximal humerus fracture, 31 patients who met the inclusion criteria and agreed to participate in the study underwent a neurophysiological study. The sample was 86% female (27 patients) and 14% male (four patients). The mean age was 71.8 years (30–96 years); 55% of fractures were on the right, 42% on the left, and 3% were bilateral.
Of the participants who received surgical treatment and underwent a neurophysiological study the day before surgery and a control study afterwards, no changes were seen between the results of the two EMGs in any of the cases.
As regards neurological involvement, 58% of the patients in the sample (18 cases) had a normal EMG or mild axonotmesis. Seven cases, 23%, had axillary neuropathy without muscle denervation, and of these, more than half (four cases) had metaphyseal fractures of the proximal humerus; albeit this comparison failed to achieve statistical significance (p>0.05). Of the patients, 19% (six cases) with fractures of the proximal humerus had lesions with axillary nerve denervation on the neurophysiological study. Of them, 86% (five cases) had a complex fracture of the proximal end of the humerus; i.e., an AO11B or AO11C fracture.
Patients who suffered complex fractures of the proximal humerus (AO11B and AO11C) were at higher risk of presenting axillary neuropathy-type injuries with muscle denervation on the neurophysiological examination; said relationship was statistically significant (p<0.001).
Consequently, there was a 42% incidence rate of axillary nerve injury based on EMG diagnosis in this sample.
As for the type of fracture, 48%13 of the fractures were type AO11A; 26%,8 type AO11B, and 26%,8 type AO11C (Table 2).
DiscussionCircumflex nerve injury is intimately related to fractures of the proximal humerus.14–17 A pattern emerges which is repeated on neurophysiological studies which reveals neuropathy of the axillary nerve without evidence of muscular denervation, and this involvement is seen predominantly in displaced fractures with a metaphyseal trace. This relationship is not statistically significant, although it would be worth reassessing in larger series with more subjects. Meanwhile, it seems that non-displaced fractures are not at risk of nerve damage. On the basis of this series, we can state that the increased risk of nerve injury with muscle denervation is seen in complex AO11B and AO11C type fractures (p<0.001). This may be an index of the likelihood of risk of axillary nerve injury, which is so essential in shoulder recovery. Therefore, knowing the patterns that have appeared in this study, we could prescribe a specific rehabilitation programme without the need for neurophysiological studies in this group of patients.
According to the results of the study, 19%6 of the patients with fractures of the proximal humerus exhibited injuries with axillary nerve denervation on the neurophysiological study. Of these, 86% had a complex fracture of the proximal humerus; i.e., AO11B or AO11C (p<0.001).
After the statistical study of the data, it could be asserted that subjects who suffer complex fractures of the proximal humerus (AO11B and AO11C) run a higher risk of axillary neuropathy type lesions with muscle denervation according to EMG evaluation (p<0.001).
As limitations of the study, we should point out: (1) the absence of preoperative CT in all patients to classify the fracture, although the more complex ones for which the classification could raise doubts did, in fact, have a CT. (2) The limited number of cases included. (3) The differences in the timing of the EMG study carried out between patients who underwent surgery and those who did not. (4) The interpretation of the results of the EMG study, which is highly dependent on the expertise of the person performing it.
This study seeks to advance the management and understanding of fractures of the proximal humerus. There are few studies that appraise axillary nerve injury with neurophysiological studies in fractures of the proximal humerus4–8; this study has enabled us to observe that concomitant axillary nerve damage is common, although most cases have a good prognosis, as they are injuries that resolve spontaneously in many cases. The article by Willis et al.4 reports a case of a complex fracture of the proximal end of the humerus with associated axillary nerve injury that required transposition surgery with the radial nerve in an elderly man. However, Entezari et al.5 published a series of 376 diaphyseal fractures of the humerus, of which 96 patients had nerve injury; he refers the following as predictors of nerve injury in diaphyseal fractures of the humerus: open fracture, associated vascular injury, high-energy trauma, and involvement of the middle or distal third as opposed to the proximal third of the humerus. Finally, Jeon et al.6 published a 26-case series of individuals undergoing deltopectoral plate osteosynthesis for a fracture of the proximal humerus or diaphysis of the humerus who underwent EMG three to four weeks following surgery. Although the series published by Jeon et al.6 exhibits a variety of pathologies, both proximal humerus fractures and diaphyseal fractures of the distal, middle, and proximal third of the humerus, 31% of the subjects presented with axillary nerve neuropathy without denervation. This result is consistent with those presented in this series, with 23% of our patients presenting with axillary nerve neuropathy without denervation.
Diagnosis of these injuries in the clinic is complex, owing to the pain, and it is difficult to assess the motor strength of the deltoid in a recent proximal humerus fracture. We must therefore suspect possible associated neurological involvement in complex fractures of the proximal humerus (types AO11B and AO11C). This could lead to improved therapeutic management of the patient.
Level of evidenceLevel of evidence III.
FundingThis research has not received any specific support from public sector agencies, the commercial sector, or non-profit organisations.
Conflict of interestsThe authors have no conflict of interests to declare.
Right to privacy and informed consentThe authors have obtained informed consent from the patients and/or subjects referred to in the article. This document is held by the corresponding author.
Ethics committee approvalThe study was approved by the Ethics Committee of Medicines of the Principality of Asturias; CEImPA: 2023.026.