This systematic review was aimed to understand the management of endodontic–periodontic lesion.
MethodsPubmed and Wiley online searches were conducted to identify articles published in dental journals until April 2018. Manual searches of published full-text articles and related reviews were performed afterwards.
ResultA total 16 studies were selected for inclusion, with 22 patients as subjects. All studies showed the decreased probing depth (PD) after treatment or healing of the lesion. All studies included were case report with treatment using root canal treatment (RCT) alone or RCT combination with bone graft or RCT with platelet rich fibrin (PRF).
ConclusionTreatment using root canal treatment (RCT) combination with bone graft was mostly used than the other treatment option in endo-perio lesion.
There are a relationship between endodontic and periodontal structures. Clinically, this relationship promotes the spread of infection, resulting in typical manifestations of endo-perio lesions. These lesions often remain free of symptoms for long periods, until it starts acute symptoms of inflammation and/or increased pain.1 The differential diagnosis of endodontic and periodontal diseases can be challenged but a correct diagnosis has a vital importance so that appropriate treatment can be provided.2
The endo-perio lesions have been characterized by the involvement of pulp and periodontal disease in the same tooth. Infection in pulp tissue may lead to secondary infection or periodontal tissue breakdown. In contrary, severe periodontal disease may initiate or exacerbate inflammatory changes in pulp tissue.3 There are some difficulties in endo-perio lesions treatment, especially when a severe loss of periodontal attachment and osseous structure occurs.4
Classification of endodontic–periodontic lesions:
- a.
Primary pulpal infection, lead to chronic periradicular periodontitis by which a periapical radiolucency (PARL) can develop and migrate cervically.
- b.
Primary periodontal infection, lead to extensive breakdown of alveolar crest bone that migrates from cervical area to the apex.
- c.
Both primary pulpal and primary periodontal infection, occur simultaneously in an “independent” endodontic–periodontic lesion, exhibiting the characteristics of both.
- d.
Primary pulpal and primary periodontal infections. occur extensively in “combined” endo-perio lesion.5
To have the success treatment of endo-perio lesions, it is helpful to understand the pathogenesis as well as the clinical and radiographic manifestations of endo-perio lesions.1 Several examinations help the diagnosis between endodontic and periodontal disease:
- a.
Vitality test: In endodontic disease, the tooth is non-vital; in periodontal disease, the tooth is vital in most cases.
- b.
Plaque/calculus: In endodontic disease, plaque or calculus may present, but they are not the primary cause of the disease; in periodontal disease, plaque or calculus is the primary cause.
- c.
Pocket/probing depth: In endodontic disease, a single and narrow pocket may present; in periodontal disease, generalized periodontal pockets may present and they are located relatively wide and coronally.
- d.
Radiographics: bone loss in endodontic disease is localized and mostly in the apical area; in periodontal disease, bone resorption is more generalized and mostly seen at the crestal bone.6
This systematic review was written according to the guidelines of PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) for reporting studies evaluating healthcare interventions. PICO question (population, intervention, control, outcome) of the present systematic review was:
P: patient with endo-perio lesion
I: endo-perio treatment
C: treated with RCT and flap operation+bone graft
O: the mostly used treatment and the best result based on probing depth
Search strategyInitial Pubmed and Wiley search of the English language literature was performed to establish a study protocol. These searches were conducted to identify articles published in dental journals until april 2018 focusing on study endo-perio treatment. The keywords used were “periodontics–endodontics lesion” AND “endo-perio treatment”. The search limits applied to the electronic search were the Article types, search period. Manual searches of published full-text articles and related reviews were performed afterwards. There are 34 studies have shown on this matter in Pubmed, and 160 studies in Wiley, with only 16 studies met the inclusion criteria. Specific keywords were used to identify the appropriate studies needs, and followed the characteristics of PICO question.
Eligibility criteriaThe inclusion criteria were:
- •
English language article
- •
Full text article
- •
Any case report published until april 2018
- •
The studies reported endodontic and periodontics lession
- •
The studies included case report or case studies
The exclusion criteria were:
- •
Animal studies
- •
Systematic review and meta-analysis studies.
- •
The studies did not report the probing depth
Specific keywords were used by two participating authors resulted the selection of the papers based on reading of abstract and full-texts. Independently, the two investigators selected the paper based on inclusion criteria formerly set. After that, all abstracts and full-texts were downloaded and individually evaluated. The eligibility criteria were used to identify the articles that will be used for this systematic review.
Extraction of dataThe data were retrieved by two reviewers that regarding following parameters: authors; year of publication; number of patients; technique; and objective. All full-texts which met the inclusion criteria were read independently by two reviewers and evaluated to formulate this systematic review.
ResultThe database search yielded 194 references, including 34 from PubMed and 160 from Wiley. After removing duplicates references, there were 189 studies remained. The titles and abstracts were reviewed afterward. The full-texts then be reviewed by the investigators and yielded 10 articles which met the inclusion criteria. The flowchart of article selection is shown in Fig. 1 with selected articles from initial yield of 194 studies by electronic literature search (Fig. 1).
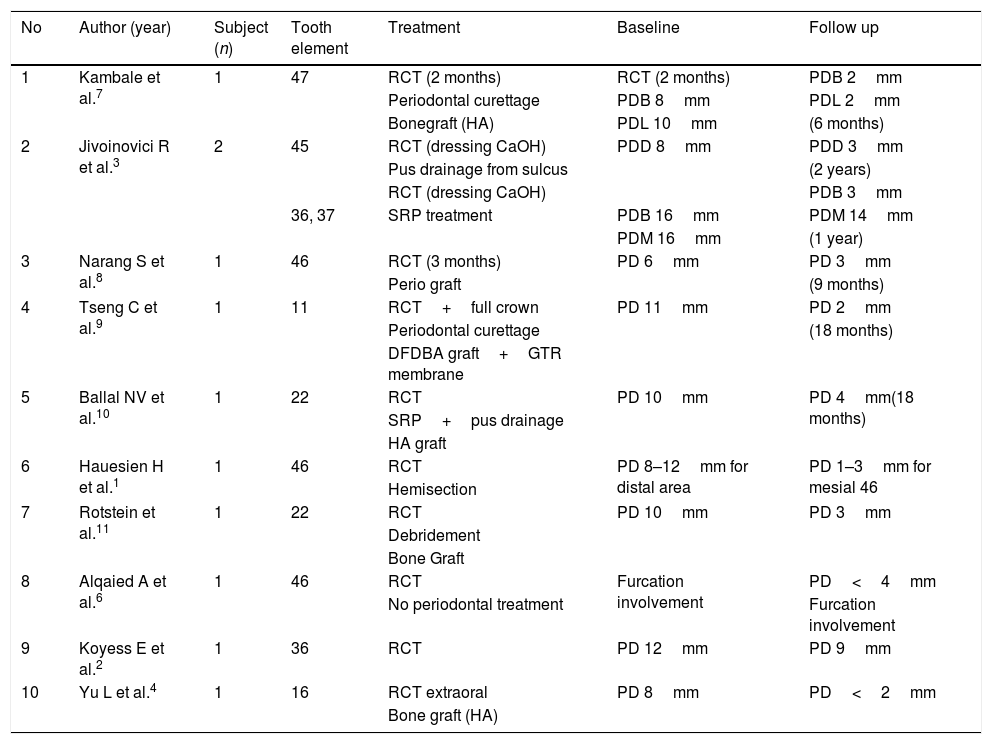
All articles were selected for full-text review. A total 10 studies were selected for inclusion, with 22 patients as subjects. All the studies showed decreased probing depth (PD) after treatment or healing of the lesion. All studies included were case report with treatment using RCT alone or RCT combination with bone graft or RCT with PRF (Table 1).
Pocket depth measurement in endo-perio lesion treatment.
| No | Author (year) | Subject (n) | Tooth element | Treatment | Baseline | Follow up |
|---|---|---|---|---|---|---|
| 1 | Kambale et al.7 | 1 | 47 | RCT (2 months) | RCT (2 months) | PDB 2mm |
| Periodontal curettage | PDB 8mm | PDL 2mm | ||||
| Bonegraft (HA) | PDL 10mm | (6 months) | ||||
| 2 | Jivoinovici R et al.3 | 2 | 45 | RCT (dressing CaOH) | PDD 8mm | PDD 3mm |
| Pus drainage from sulcus | (2 years) | |||||
| RCT (dressing CaOH) | PDB 3mm | |||||
| 36, 37 | SRP treatment | PDB 16mm | PDM 14mm | |||
| PDM 16mm | (1 year) | |||||
| 3 | Narang S et al.8 | 1 | 46 | RCT (3 months) | PD 6mm | PD 3mm |
| Perio graft | (9 months) | |||||
| 4 | Tseng C et al.9 | 1 | 11 | RCT+full crown | PD 11mm | PD 2mm |
| Periodontal curettage | (18 months) | |||||
| DFDBA graft+GTR membrane | ||||||
| 5 | Ballal NV et al.10 | 1 | 22 | RCT | PD 10mm | PD 4mm(18 months) |
| SRP+pus drainage | ||||||
| HA graft | ||||||
| 6 | Hauesien H et al.1 | 1 | 46 | RCT | PD 8–12mm for distal area | PD 1–3mm for mesial 46 |
| Hemisection | ||||||
| 7 | Rotstein et al.11 | 1 | 22 | RCT | PD 10mm | PD 3mm |
| Debridement | ||||||
| Bone Graft | ||||||
| 8 | Alqaied A et al.6 | 1 | 46 | RCT | Furcation involvement | PD<4mm |
| No periodontal treatment | Furcation involvement | |||||
| 9 | Koyess E et al.2 | 1 | 36 | RCT | PD 12mm | PD 9mm |
| 10 | Yu L et al.4 | 1 | 16 | RCT extraoral | PD 8mm | PD<2mm |
| Bone graft (HA) |
When the pulp becomes necrotic, there is a direct inflammatory response by the periodontal ligament at the apical foramen or accessory canals. Many of these are similar pathogens encountered in periodontal infections. On the other hand, the effect of periodontal disease on the pulp is degenerative in nature including an increase in calcifications, fibrosis and collagen resorption.11 Inadequacy of the coronal seal leading to microleakage can be one of the reasons for the failure of the root canal treatment. Teeth that has undergone periodontal surgery had a more favorable healing response with the gain of connective tissue attachment when occlusal trauma was relieved.10
The primary endodontic disease with secondary periodontal involvement should first be treated with an endodontic therapy. Prognosis depend on the severity of periodontal involvement, periodontal treatment and patient response. The differential diagnosis is difficult when a sinus tract, originating from the endodontic lesion may drain along periodontal ligament. Therefore, a primary endodontic lesion draining from attachment apparatus should be initially treated by an endodontic therapy.3
Endodontic treatment is highly predictable and has high successful rate when appropriately performed. If majority of bony support has been lost from periodontitis, regardless of predictability of endodontic therapy, tooth may have hopeless prognosis. Regeneration, root resection and hemisection are indicated as a part of strategic treatment of multirooted teeth.8
The etiology and diagnosis of dental abscesses are based on patient history as well as clinical and radiographic findings. Vitality testing can detect changes of sensation caused by pulpal inflammation and necrosis. If there is evidence of pulpal disease and the possibility of associated periodontal bone loss, the endodontic treatment should be completed first and then the patient should be reevaluated. In many cases, apparent periodontal pathology, including bone loss, suppuration, and pocket depth resolves if there has been a pulpal lesion that has been successfully treated endodontically. Residual periodontal problems can be treated after completion of successful endodontic treatment, and in many cases, successful regeneration of periodontal defects is possible in endodontically treated teeth.9
Bone grafting materials can be broadly classified into natural and synthetic types. Natural bone grafts include autogenous bone, allograft, and xenograft, while the synthetic types are commonly known as alloplastic materials.12 Hydroxyapaptite (HA) has been used as a bone replacement material for many years and that has been demonstrated that HA has excellent biocompatibility, high osteogenic potential and anti-infection capacity.2
Hydroxyapatite (HA) was found to be a useful material in the reconstruction of periodontal defects, due to its ability to dissolve, break down, and allow new bone formation and remodeling required to attain optimal mechanical strength without interference2. It took one month for epithelial attachment to establish and complete bone formation will occur six month after periodontal surgery.7,13
An accurate diagnosis is mandatory for the successfully treated endo-perio lesions. This diagnosis must cover both endodontic and periodontal component of the lesion. If the primary aspect cannot be evaluated, endodontic treatment should be given precedence, followed by a wait-and-see approach until a decision for any additional endosurgical and/or periodontal procedure can be focussed.1
ConclusionTreatment using Root Canal Treatment (RCT) combination with bone graft was mostly used than other treatment option in endodontic–periodontic lesion.
Conflict of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the International Conference on Women and Societal Perspective on Quality of Life (WOSQUAL-2019). Full-text and the content of it is under responsibility of authors of the article.