Diabetes in elderly people is one of the main problems for our Public Health System today. Aging is causing a marked increase in the pandemic of diabetes and its prevalence in Spain for men and women older than 75 years-old is greater than 20%.1 We know that the therapeutic strategies and targets should be individualized in these patients but scientific evidence to support the most appropriate treatment is scarce.2–3 Metformin is the first-line agent and recent studies have indicated that it may be used safely in patients with estimated glomerular filtration rate (eGFR) ≥30ml/min/1.73m2. However, metformin is contraindicated in patients with advanced renal insufficiency. Sulfonylureas are associated with hypoglycemia and should be used with caution in patients with increased susceptibility.4–5 Ruiz-Tamallo et al. observed that a significant proportion of patients with eGFR <30ml/min/1.73m2 were on metformin or sulfonylureas treatment.6 The aim of our study was to know if the use of metformin and sulfonylureas were lower in patients ≥75 years-old with eGFR <45ml/min/1.73m2 and determine the prevalence of patients ≥75 years-old who are in treatment with metformin or sulfonylureas that have had eGFR <30ml/min/1.73m2 or without eGFR within the last year.
From January 2017 to April 2017, we identified in our pharmacological prescription program, 1183 patients ≥75 years-old who were taking pharmacological treatment for diabetes (insulin and no insulin). These patients live among the three basic health areas located in the southeast of Castilla-La Mancha which attend a total of 41992 inhabitants. 70.4% of them were treated with metformin and 14% with sulfonylureas (13 patients were on gliblenclamide treatment). We analyzed a randomly selected sample of 295 patients (calculated to have enough statistical power) and the following variables were collected: age (years), sex (male or female), pharmacological treatment for diabetes (metformin, sulfonylureas, glinides, thiazolidinediones, DPP-4 inhibitors, GLP-1 receptor agonist, SGLT-2 inhibitors and insulin), and the last blood analysis with A1c and eGFR in the previous year.
Data were analyzed with the use of G-Stat 2.0 software. Qualitative variables were expressed as an absolute and relative frequency. Quantitative variables were expressed as a mean and standard deviation (SD). The Chi-square test was used to compare proportions of use of metformin or sulfonylureas between two groups (eGFR <45ml/min/1.73m2 vs. eGFR ≥45ml/min/1.73m2). A p value <0.05 was considered statistically significant.
The mean age was 82.7 years (SD: 5.1) and 106 patients (35.9%) were 85 years of age or older. 173 patients (58.6%) were women. 220 patients (74.6%) were on metformin, 39 (13.2%) on sulfonylureas, 18 (6.1%) on glinides and 99 (33.6%) on DPP-4 inhibitors. Only 1 patient was treated with GLP-1 receptor agonist and 9 with SGLT-2 inhibitors. 45 patients (15.2%) were on basal insulin analogs and 18 (6.1%) on premixed insulin. Only 3 patients were treated with intermediate acting insulin (Human NPH or NPL insulin) and only 5 with basal-acting insulin more rapid-acting insulin.
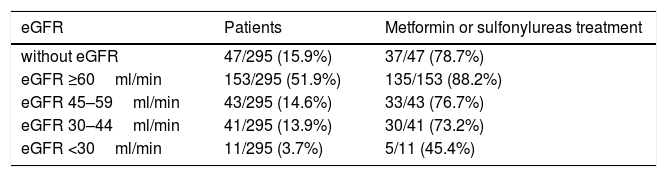
The mean A1c was 7.1% (SD: 1.2) but only 190 patients (64.4%) had this result in the last year. 47 patients (15.9%) did not have eGFR during the last year and 11 (3.7%) had eGFR <30ml/min/1.73m2. 153 patients (51.9%) had eGFR ≥60ml/min/1.73m2, 43 (14.6%) between 45 and 59ml/min/1.73m2 and 41 (13.9%) between 30 and 44ml/min/1.73m2 (Table 1). Thirty five patients with eGFR <45ml/min/1.73m2 (67.3%) were treated with metformin or sulfonylureas vs. 168 patients with eGFR ≥45ml/min/1.73m2 (85.7%) (p: 0.0079). Forty two patients treated with metformin or sulfonylureas (17.5%; IC 95%, 12.9–22.9%) had eGFR <30ml/min/1.73m2 or did not have eGFR during the last year.
Estimated glomerular filtration rate (eGFR) and metformin or sulfonylureas treatment.
| eGFR | Patients | Metformin or sulfonylureas treatment |
|---|---|---|
| without eGFR | 47/295 (15.9%) | 37/47 (78.7%) |
| eGFR ≥60ml/min | 153/295 (51.9%) | 135/153 (88.2%) |
| eGFR 45–59ml/min | 43/295 (14.6%) | 33/43 (76.7%) |
| eGFR 30–44ml/min | 41/295 (13.9%) | 30/41 (73.2%) |
| eGFR <30ml/min | 11/295 (3.7%) | 5/11 (45.4%) |
Selection of a limited sample of the total elegible population and restriction to a small spanish region were the main limitations of our study. However, others have shown similar results in other geographical areas with larger populations.
In conclusion, the use of metformin and sulfonylureas were lower in patients with eGFR <45ml/min/1.73m2 vs. patients with eGFR ≥45ml/min/1.73m2 but 17.5% of patients ≥75 years-old treated with metformin or sulfonylureas had eGFR <30ml/min/1.73m2 or did not have eGFR during the last year. It is necessary to monitor and help physicians to avoid inappropriate prescription specially in older people.
We thank Anjali Sood, medicine student at Jacobs School of Medicine and Biomedical Science (University at Buffalo) for critically reading the manuscript.