The aim of this study was to assess the incidence of obstetric and neonatal complications in pregnant women with “normal” thyroid-stimulating hormone (TSH) levels in the first trimester (group A) and to compare them with those with “slightly elevated” TSH (SET) levels treated with levothyroxine (group B2) or not treated (group B1).
MethodsA total of 2375 women who had been performed laboratory tests in their first trimester of pregnancy were detected at our hospital between April 2015 and August 2017. Of these, 469 patients with SET were prospectively detected and randomized to groups B1 (227) and B2 (242). They were monitored prospectively until 6 months after delivery. Data of the control group (n=1906, group A) were retrospectively reviewed. A total of 1745 women were analyzed. Variables assessed included demographic and clinical characteristics and complications of pregnancy and delivery.
ResultsA, B1, and B2 had similar clinical characteristics. There were no statistically significant differences in complications between the three groups during pregnancy, except in that natural deliveries were more common in group A as compared to group B1 (76.8% vs. 68.7%, p 0.017) and group B2 (66.3%), p<0.002). There were more induced deliveries in groups B1 (35.8%), and B2 (36.2%) than in group A (18.4%), p<0.01. Although the recommended TSH level was achieved in the second and third trimesters, no benefit could be found of treatment of SET.
ConclusionAlthough there were less natural deliveries and more induced deliveries in patients with SET, treatment with levothyroxine could not reverse this situation, despite achievement of levels considered appropriate in the second and third trimester.
El propósito de este estudio fue investigar la incidencia de complicaciones obstétricas y neonatales en mujeres embarazadas con una tirotropina (TSH) «normal» en el primer trimestre (grupo A) y compararlas con aquellas con una TSH «discretamente elevada» (SET) tratadas con levotiroxina (grupo B2) o no (grupo B1).
MétodosDos mil trescientos setenta y cinco gestantes con analítica en el primer trimestre fueron detectadas en nuestro hospital entre abril de 2015 y agosto de 2017. Cuatrocientos sesenta y nueve pacientes con SET se detectaron prospectivamente y randomizaron a los grupos B1 (227) y B2 (242). Se siguieron prospectivamente hasta 6 meses posparto. Los datos del grupo control (n=1.906, grupo A) se revisaron retrospectivamente. Se analizaron 1.745 pacientes. Las variables incluyeron características demográficas, clínicas y complicaciones de la gestación y el parto.
ResultadosA, B1 y B2 eran comparables en sus características clínicas. Los partos eutócicos fueron más frecuentes en el grupo A que en el B1 (76,8 vs. 68,7%, p0,017) y B2 (66,3%, p<0,002). Hubo más partos inducidos en los grupos B1 (35,8%) y B2 (36,2%) que en A (18,4%), p<0,01. Aunque se alcanzó el nivel de TSH recomendado en el segundo y tercer trimestres, no pudimos encontrar ningún beneficio en el tratamiento de SET.
ConclusiónAunque hemos encontrado menos partos eutócicos y más partos inducidos en las gestantes con SET, el tratamiento con levotiroxina no pudo revertirlo, pese a alcanzar un valor considerado apropiado en el segundo y tercer trimestre.
Subclinical hypothyroidism has been considered to impair the normal metabolism and to increase complications in pregnancy, neurological development of fetus and delivery, but not all the authors agree.
There is not a “normal” TSH value (referring to the value from which there can be deleterious effects) because it depends on the population clinical characteristics, weeks of gestation and iodine status.1,2
Previous Guidelines recommended having reference values for each population at each trimester of gestation because of this variability. If not available, a TSH value higher or equal to 2.5mcU/mL was recommended as the level to initiate treatment with levothyroxine not only in the American Guidelines3,4 but also in the Spanish Guide of 2009.5
Different reference values have been published depending not only on the population but on the laboratory method.6,7
The adverse effects and need of treatment of isolated hypothyroxinemia8,9 and positive antithyroid antibodies is also a theme of debate.10 A 2013 review concluded that treatment could not always be recommended with enough evidence.11
A slight elevation of TSH (SET), also called subclinical hypothyroidism in pregnancy (between 2.5 and 4.9mcU/mL) has been found to be associated to abortion risk induced delivery, preterm birth and cesarean sections.12–14
In women with positive antithyroid antibodies treatment with even TSH levels as low as higher than 1mcU/mL has been alleged to diminish the abortion rate.12 But not all the authors agree. In a Spanish recent work, pregnant women with positive antibodies have a slightly more elevated TSH level but without more complications.15
A 2016 meta-analysis defined subclinical hypothyroidism in a very similar way to our defined “slight elevation of TSH (SET)” finding a higher risk of abortion, abruption placentae, premature membranes rupture and neonatal death.13
A 2017 meta-analysis found also a higher risk of preterm deliveries in women with hypothyroidism whether clinical or subclinical.14
Despite a high variability in these results, the American Thyroid Guidelines published in 2011 recommended treatment with levothyroxine in SET in those populations with reference TSH values not available.4
In the different studies published from then, 3–30% of pregnant women would have a SET in their antenatal screening.16
This approach has been implemented in the public and private medical practice with an increased number of “patients” referred to the Endocrinology consultation implying not only a medical overload but a concern in pregnant women.
Treatment of subclinical hypothyroidism has been associated to a risk of small for gestational age and cognitive impairment in some cases.17
Although there is no medical disagreement considering TSH values higher than the upper limit of normality with fT4 normal for treatment there is still an important controversy in SET, differing their management and approach between medical centers and doctors due to the lack of randomized clinical controlled trials. The level of TSH to start treatment in pregnancy is so, still subject of debate.18 In non-pregnant populations, treatment of subclinical hypothyroidism with levothyroxine is not risk free.19,20 Besides, some authors,21 but no others,22 have found more adverse events in treated women mainly preterm delivery, gestational diabetes and pre-eclampsia recommending caution when considering treatment.
When the first American Guidelines were published in 2011, and owed to the difference between our TSH percentiles in the antenatal screening and the proposed values for treatment, we designed a prospective study with the objectives of evaluating the incidence of obstetric and neonatal complications in our population with normal TSH (0.14–2.49mcU/mL), to assess if there were differences in the complication rate between them and pregnancies with SET (2.5–4.5mcU/mL) and to clarify if treatment with levothyroxine could modified them.
Material and methodsHypothesisOur main hypothesis is that levothyroxine treatment in pregnant women with a slightly elevated TSH (SET) (TSH between 2.5 and 4.9mcU/mL) is not beneficial in our pregnant population (group B2 vs. B1). Our secondary hypothesis is that women with SET non treated (group B1) have no more complications than control women with a TSH in the antenatal screening between 0.14 and 2.5mcU/mL (group A).
DesignIt is an ambispective study with two parts:
- –
A prospective randomized cohorts study including those patients with SET not treated (group B1) and treated (group B2).
- –
A retrospective cohorts study of those patients with a TSH between 0.14 and 2.49mcU/mL in the antenatal screening (group A).
Inclusion criteria: pregnant women with their first trimester TSH antenatal screening performed in the Hospital Severo Ochoa between January the 1st 2015 and August the 31st 2017.
Exclusion criteria: previous treatment with levothyroxine, overt hypothyroidism, voluntary pregnancy termination, twin pregnancies, recurrent abortion (more than 2 previous abortions) and subclinical hypothyroidism (TSH≥5mcU/mL and normal free thyroxine (fT4)).
Study protocol: a biochemistry doctor reviewed weekly all the antenatal screening performed in the selected period and selected those with a TSH between 2.5 and 4.9mcU/mL (97.5th percentile in our pregnant population) and analyzed their thyroid peroxidase antibodies (TPOAb). Analyses in our hospital are usually requested by the obstetrician in the first visit and scheduled between 7 and 13th week of gestation. Patients were randomized by the Endocrinology Department Secretary to any of two groups, each of them visited by the same doctor during the whole study, being group B1 and B2 non-treated and treated respectively. Patients in both groups signed an informed consent and were followed prospectively with visits scheduled in the second, third trimester and 3–6 months after delivery. Treatment was started with levothyroxine in group B2 at an initial dose of 0.5mcg/kg of body weight and adjusted as needed in the following visits to reach a TSH level below 3 in the second and third trimester of gestation as proposed by guidelines. In a second phase, data of all pregnant women with an antenatal TSH screening in the same period of time between 0.14 and 2.5mcU/mL, were reviewed retrospectively using the computer data to investigate their TSH antenatal level, obstetric visits and delivery reports. The Hospital Informatics Service obtained these data to guarantee the confidentiality as required. The Hospital Severo Ochoa Ethics Review Board approved both phases of the study.
Variables: age, gestational age at first visit, medical (specifically referred to thyroid pathologies and smoking habit) and obstetric (number of gestations including this and previous abortions) antecedents, ethnicity, thyrotropin (TSH) and free thyroxin (fT4) in the first trimester, TPOAb (antithyroid peroxidase antibodies) in the first trimester and TSH and fT4 in the second and third trimester in groups B1 and B2. All of them were measured using automated immunoassays with chemiluminescence detection (Advia Centaur Xp Siemens). Weight, body mass index and weight increment during gestation in every visit in groups B1 and B2. Data were collected for group A if they were present in the obstetric reports, arterial hypertension and pre-eclampsia in the third trimester, oligohydramnios and/or polyhydramnios, gestational diabetes mellitus defined as both positive (O'Sullivan test and Carpenter y Coustan criteria in the 100g glucose overload), abortion, gestational age at birth in weeks, labor characteristics: spontaneous vs. induced and the cause of induction classified as premature membrane rupture, pre-eclampsia or hypertension, delayed intrauterine growth, maternal interest (iterative cesarean section, previous placenta, etc.) or fetal interest (oligohydramnios, chronologically prolonged gestation, etc.); eutocic (vaginal delivery being instrumental or not) or cesarean section and cause of cesarean section divided in birth dystocia (no labor progression, cephalic pelvic disproportion, etc.), fetal suffering, elective cesarean section (breech birth, previous placenta, etc.) and delayed intrauterine growth. Birth weight in grams and admission in Neonates Unit and its cause classified as maternal, respiratory distress, prematurity, reanimation (any short of ventilation required) and others (swallowing problems, gastroesophageal reflux, etc.)
Statistics: descriptive analyses: percentages for qualitative and mean and standard deviation for quantitative variables respectively. Bivariate analyses: Chi-square test for qualitative and the Student's t for quantitative variables. For those variables that did not comply with the Kolmogorov–Smirnoff test of normality or those with non-homogeneous variances according to the Levine test, we used the non-parametric Mann–Whitney test.
p<0.05 was the considered level of statistical significance. The Microsoft Excel 2013 program and the SPSS 22.0 computer package were used.
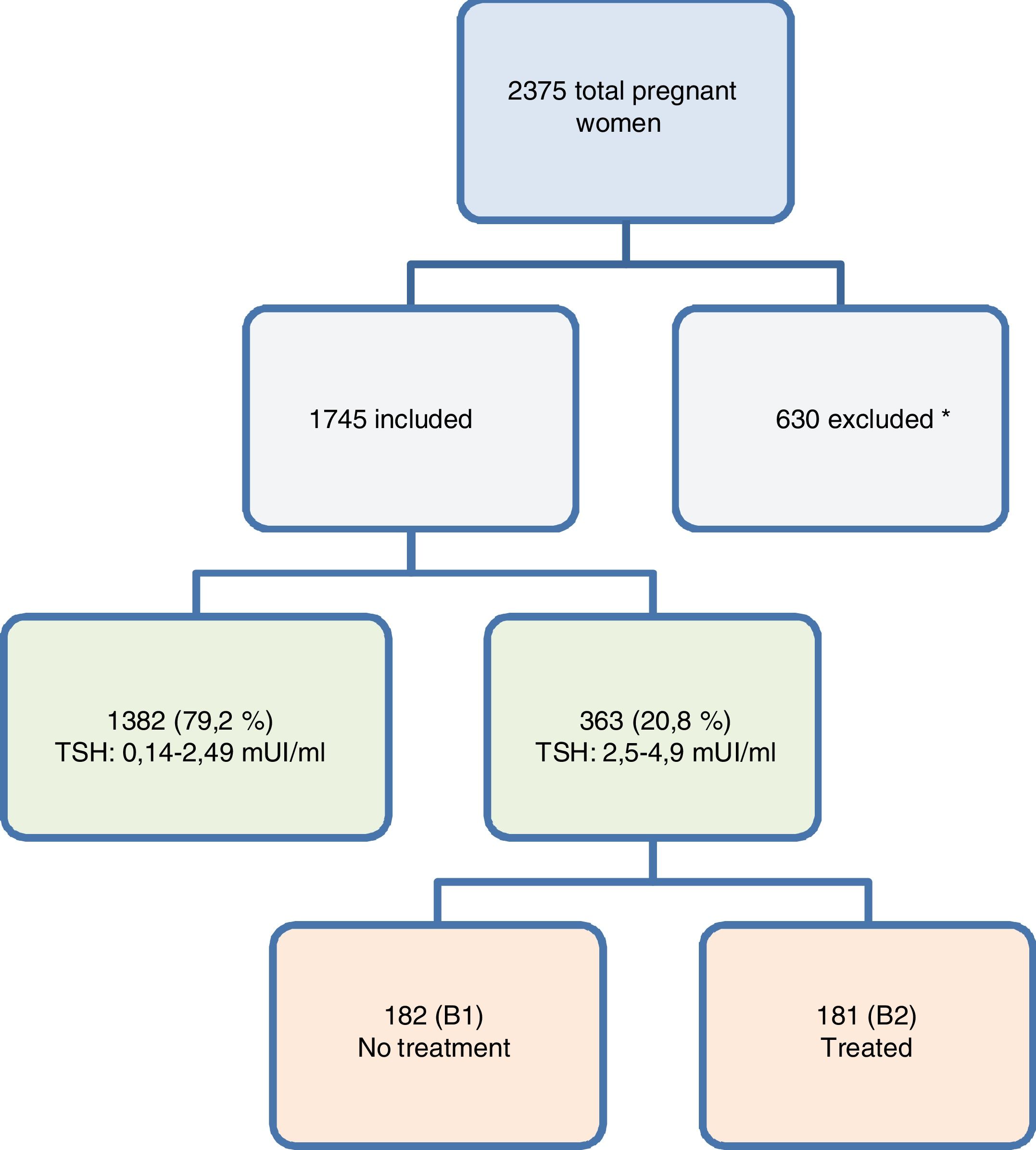
ResultsDuring the study period 2375 pregnancies were followed in our Hospital being 469 (19.74%) randomized to group B1 (n: 227, 48.4%) and 242 to group B2 (51.6%) p<0.09 and followed prospectively. The remaining 1906 patients had their TSH value and their obstetrical reports reviewed retrospectively using computerized data.
630 (26.5% of the total) were excluded for the analyses: 524 belonging to the group A (13.8%) and 106 to group B (22.6%) (45 to group B1 (19.8%) and 61 to group B2 (25.2%)) see Fig. 1.
* Exclusion causes were: 207 (32.8%) lacking their antenatal TSH screening in the Hospital computers, 108 (17.1%) were previously treated, 102 (16.1%) were lost in the follow-up, 36 (5.7%) had subclinical hyperthyroidism, 32 (5.07) had not been randomized, 31 (4.9%) had overt hypothyroidism, 28 (4.4%) had >2 previous abortions, 26 were twin pregnancies, 26 (4.4%) had overt hyperthyroidism, 25 (3.9%) did not comply with the study protocol, 7 (1.1%) had a voluntary pregnancy interruption and 2 (0.31%) had an spontaneous abortion before being randomized.
There were no statistically significant differences in exclusion motives between A, B1 and B2 groups (p=0. 29). Finally, 1745 pregnant women entered this study:
Group A (TSH: 0.14–2.49mcU/mL): 1382 (79.2%).
Group B (TSH: 2.5–4.9mcU/mL): 363 (20.8%). B1 (non-treated): 182 (10.4%) and B2 (treated): 181 (10.4%).
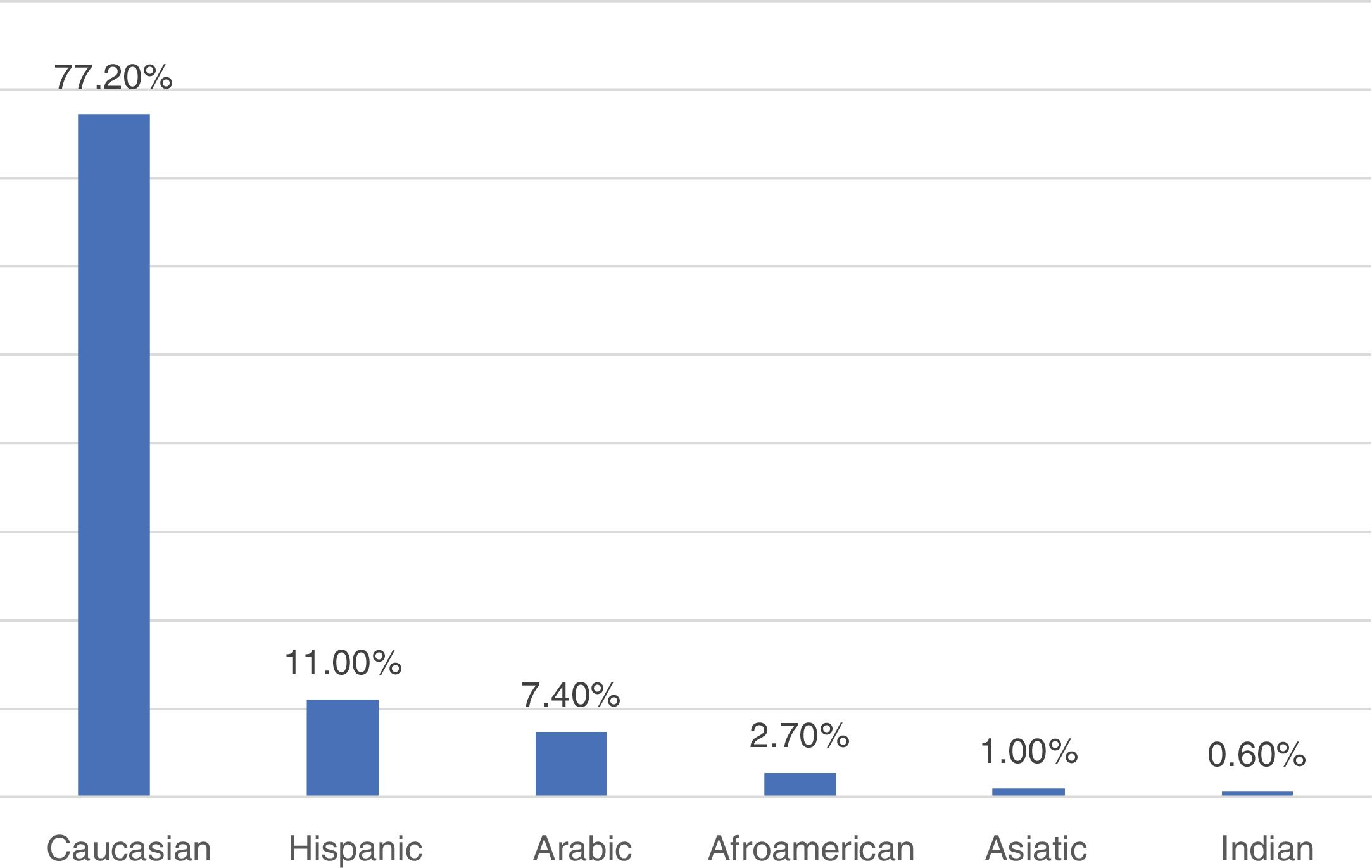
The ethnic distribution is shown in Fig. 2 not being the three groups statistically different (p=0.578). The age of our population was 32±5 years (14–48). The first visit took place in the 12.55±2 weeks. Median TSH in the first trimester was 1.91±1.61mcU/mL. Our population's 97.5th percentile of TSH as determined by this study was 4.9mcU/mL.
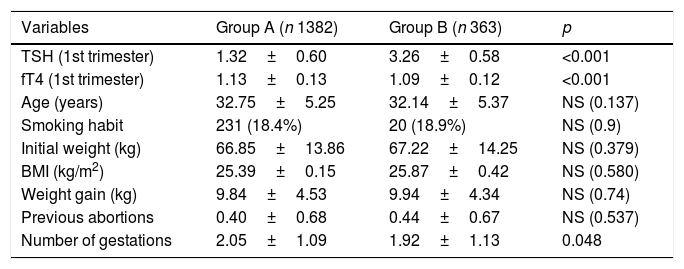
Comparative analyses of groups A and BData are shown in Table 1. There were no statistically significant differences with respect to age, smoking habit, initial weight, body mass index, weight gain or previous abortions.
General and demographic characteristics of women included in the study comparing those with a TSH<2.5 vs. those with a TSH≥2.5 and <4.9mUI/mL.
| Variables | Group A (n 1382) | Group B (n 363) | p |
|---|---|---|---|
| TSH (1st trimester) | 1.32±0.60 | 3.26±0.58 | <0.001 |
| fT4 (1st trimester) | 1.13±0.13 | 1.09±0.12 | <0.001 |
| Age (years) | 32.75±5.25 | 32.14±5.37 | NS (0.137) |
| Smoking habit | 231 (18.4%) | 20 (18.9%) | NS (0.9) |
| Initial weight (kg) | 66.85±13.86 | 67.22±14.25 | NS (0.379) |
| BMI (kg/m2) | 25.39±0.15 | 25.87±0.42 | NS (0.580) |
| Weight gain (kg) | 9.84±4.53 | 9.94±4.34 | NS (0.74) |
| Previous abortions | 0.40±0.68 | 0.44±0.67 | NS (0.537) |
| Number of gestations | 2.05±1.09 | 1.92±1.13 | 0.048 |
Quantitative data are expressed in mean±standard deviation and qualitative data in percentage.
Women with a higher TSH had fewer previous gestations as the only significant difference between both groups.
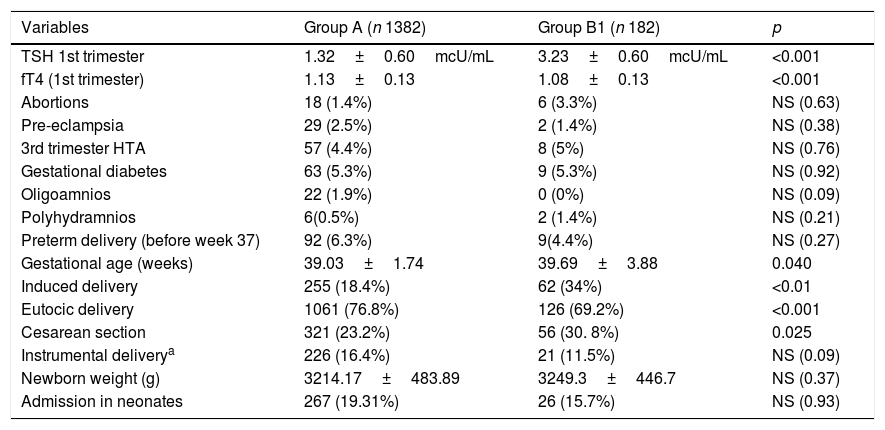
Comparative analyses of groups A and B1Data are shown in Table 2. There were no statistically significant differences between both groups with respect to age, smoking habit, previous thyroid pathology, initial weight, body mass index, weight gain, previous abortions, number of gestations, abortions, pre-eclampsia, hypertension in the 3rd trimester, gestational diabetes, oligohydramnios, polyhydramnios, preterm delivery, cause of induction of delivery (being the most frequent in both groups the fetal interest), cause of cesarean section, instrumental deliveries, newborn weight nor admission in neonates or its cause. There were statistically significant differences in gestational age (not being clinically relevant), as well as in the induced delivery and the cesarean sections being both more frequent in the SET group as it will be discussed lately.
Comparative maternal and fetal prognosis between those pregnant women with a TSH<2.5mUI/mL and those with a TSH≥2.5 and ≤4.9mUI/mL not being treated.
| Variables | Group A (n 1382) | Group B1 (n 182) | p |
|---|---|---|---|
| TSH 1st trimester | 1.32±0.60mcU/mL | 3.23±0.60mcU/mL | <0.001 |
| fT4 (1st trimester) | 1.13±0.13 | 1.08±0.13 | <0.001 |
| Abortions | 18 (1.4%) | 6 (3.3%) | NS (0.63) |
| Pre-eclampsia | 29 (2.5%) | 2 (1.4%) | NS (0.38) |
| 3rd trimester HTA | 57 (4.4%) | 8 (5%) | NS (0.76) |
| Gestational diabetes | 63 (5.3%) | 9 (5.3%) | NS (0.92) |
| Oligoamnios | 22 (1.9%) | 0 (0%) | NS (0.09) |
| Polyhydramnios | 6(0.5%) | 2 (1.4%) | NS (0.21) |
| Preterm delivery (before week 37) | 92 (6.3%) | 9(4.4%) | NS (0.27) |
| Gestational age (weeks) | 39.03±1.74 | 39.69±3.88 | 0.040 |
| Induced delivery | 255 (18.4%) | 62 (34%) | <0.01 |
| Eutocic delivery | 1061 (76.8%) | 126 (69.2%) | <0.001 |
| Cesarean section | 321 (23.2%) | 56 (30. 8%) | 0.025 |
| Instrumental deliverya | 226 (16.4%) | 21 (11.5%) | NS (0.09) |
| Newborn weight (g) | 3214.17±483.89 | 3249.3±446.7 | NS (0.37) |
| Admission in neonates | 267 (19.31%) | 26 (15.7%) | NS (0.93) |
HTA: arterial hypertension. Quantitative data are expressed in mean±standard deviation and qualitative data in percentage.
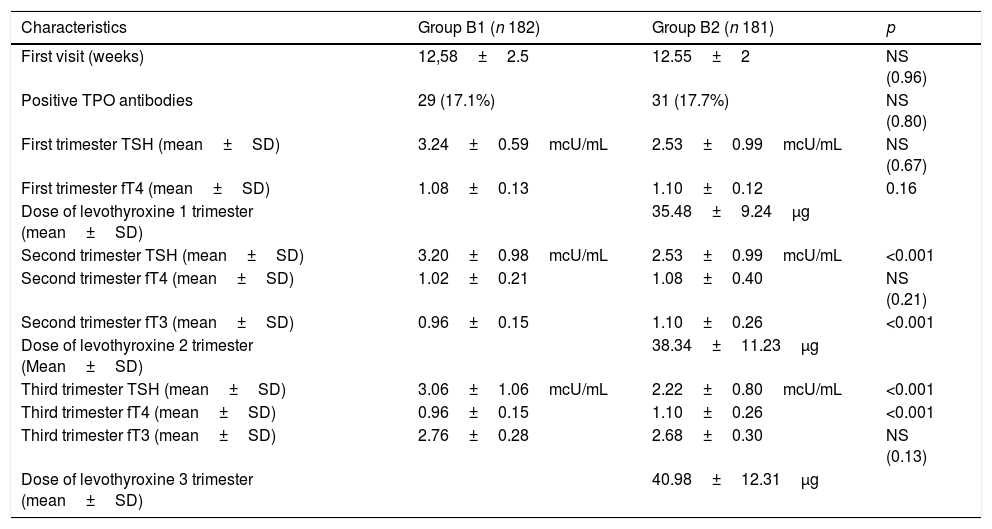
Data are shown in Table 3. A significant different TSH value was achieved with treatment in the second and third trimester.
Analytical characteristics and treatment of groups B1 and B2.
| Characteristics | Group B1 (n 182) | Group B2 (n 181) | p |
|---|---|---|---|
| First visit (weeks) | 12,58±2.5 | 12.55±2 | NS (0.96) |
| Positive TPO antibodies | 29 (17.1%) | 31 (17.7%) | NS (0.80) |
| First trimester TSH (mean±SD) | 3.24±0.59mcU/mL | 2.53±0.99mcU/mL | NS (0.67) |
| First trimester fT4 (mean±SD) | 1.08±0.13 | 1.10±0.12 | 0.16 |
| Dose of levothyroxine 1 trimester (mean±SD) | 35.48±9.24μg | ||
| Second trimester TSH (mean±SD) | 3.20±0.98mcU/mL | 2.53±0.99mcU/mL | <0.001 |
| Second trimester fT4 (mean±SD) | 1.02±0.21 | 1.08±0.40 | NS (0.21) |
| Second trimester fT3 (mean±SD) | 0.96±0.15 | 1.10±0.26 | <0.001 |
| Dose of levothyroxine 2 trimester (Mean±SD) | 38.34±11.23μg | ||
| Third trimester TSH (mean±SD) | 3.06±1.06mcU/mL | 2.22±0.80mcU/mL | <0.001 |
| Third trimester fT4 (mean±SD) | 0.96±0.15 | 1.10±0.26 | <0.001 |
| Third trimester fT3 (mean±SD) | 2.76±0.28 | 2.68±0.30 | NS (0.13) |
| Dose of levothyroxine 3 trimester (mean±SD) | 40.98±12.31μg |
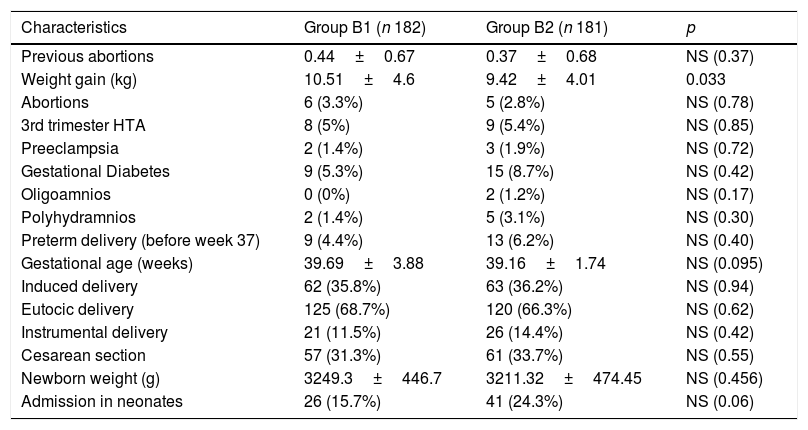
Data are shown in Table 4. There were no statistically significant differences with respect to age, smoking habit, previous thyroid pathology, initial weight, body mass index or any other basal demographic characteristics.
Comparative maternal and fetal prognoses between both groups, treated and not treated.
| Characteristics | Group B1 (n 182) | Group B2 (n 181) | p |
|---|---|---|---|
| Previous abortions | 0.44±0.67 | 0.37±0.68 | NS (0.37) |
| Weight gain (kg) | 10.51±4.6 | 9.42±4.01 | 0.033 |
| Abortions | 6 (3.3%) | 5 (2.8%) | NS (0.78) |
| 3rd trimester HTA | 8 (5%) | 9 (5.4%) | NS (0.85) |
| Preeclampsia | 2 (1.4%) | 3 (1.9%) | NS (0.72) |
| Gestational Diabetes | 9 (5.3%) | 15 (8.7%) | NS (0.42) |
| Oligoamnios | 0 (0%) | 2 (1.2%) | NS (0.17) |
| Polyhydramnios | 2 (1.4%) | 5 (3.1%) | NS (0.30) |
| Preterm delivery (before week 37) | 9 (4.4%) | 13 (6.2%) | NS (0.40) |
| Gestational age (weeks) | 39.69±3.88 | 39.16±1.74 | NS (0.095) |
| Induced delivery | 62 (35.8%) | 63 (36.2%) | NS (0.94) |
| Eutocic delivery | 125 (68.7%) | 120 (66.3%) | NS (0.62) |
| Instrumental delivery | 21 (11.5%) | 26 (14.4%) | NS (0.42) |
| Cesarean section | 57 (31.3%) | 61 (33.7%) | NS (0.55) |
| Newborn weight (g) | 3249.3±446.7 | 3211.32±474.45 | NS (0.456) |
| Admission in neonates | 26 (15.7%) | 41 (24.3%) | NS (0.06) |
The only statistically significant difference found is the weight gain being lower in the treated group.
DiscussionCompared to other studies of pregnancy complications related to a similar TSH range in the antenatal screening, our population was slightly thinner and had a lower TSH than others, perhaps explaining a lower gestational diabetes and pre-eclampsia rate in our study.19
We studied and compared a group of patients with a slightly elevated TSH (SET) (≥2.5 and <5mcU/mL, group B) with a group of pregnant women with a TSH<2.5mcU/mL in the antenatal screening (control group A). Our study took place in a clinical day to day context. Patients had their antenatal screening analysis after the first visit with the obstetrician. So the week of screening was not scheduled in advanced because we planned the study to reproduce the real life conditions. When an altered TSH was detected by the laboratory doctor, the patient was appointed to an endocrinologist visit as soon as possible, usually not more than a week after having the blood test results.
Although there were not more previous abortions in group B, there had been more previous pregnancies in the control group (A). We could only speculate that it is easier to become pregnant in our population with a slightly lower TSH.
Non treated patients with SET (B1) had more induced and less eutocic births than the control group (A), but we cannot explain the reason because there are no differences in the analyzed causes of induction, being the main cause a fetal interest.
We found also a higher variability in the gestational age at birth without more preterm deliveries contrary to a recent meta-analysis.14 Nevertheless, these results are in agreement with the strategies for preterm delivery that do not include thyroid dysfunction as a risk factor.23
We could not find a significant different proportion of abortions, preterm delivery, gestational diabetes and hypertensive conditions between groups B1 and A. This is in agreement with recent reviews raising doubts about the need for universal treatment.10,16
We could not show a negative effect of positive thyroid antibodies in our patients but we only measure thyroid peroxidase antibodies (anti-TPO) in patients with SET.
We cannot conclude anything about the effect of free thyroxin in pregnancy because following current clinical practice in our hospital, it is only determined when TSH is altered.
Treatment of SET in the antenatal screening remains controversial nowadays. In our study we randomized patients to be treated or not and followed prospectively to try to clarify this point.
We could not find any benefit of treatment with levothyroxine starting in the 12th week of gestation. In spite of achieving a TSH level with treatment in the second and third trimester in the range proposed by the Guidelines,24 we have not found statistically significant differences with respect to abortion, cesarean sections, gestational diabetes, hypertension, preeclampsia, polyhydramnios, oligohydramnios, instrumental delivery or other pregnancy complications.
Both groups differed statistically only in an increase of one kilogram of body weight higher in the non-treated patients and there were no clinical complications related to treatment during the study.
Different outcomes have been published depending on the gestational week and the treatment duration required to reach the targeted TSH level25 so we can only conclude that in our current clinical practice we cannot recommend treatment for SET.
Due to all these different and contradictory results, some authors have proposed to treat it in an individualized way, considering pregnant women susceptible of treatment if symptoms or goiter are present and avoiding overtreatment.16
In 2017 the new Guidelines and Recommendations have changed the proposed level for treatment to a TSH higher than 4mcU/mL in negative antithyroid antibodies pregnant women lacking their own reference values.4
Our study had a retrospectively followed control group, avoiding clinical interference with the pregnancy evolution. The main strength of this work was the prospective follow-up and randomization of all the susceptible pregnant women with a SET in the antenatal screening in our Hospital in a period of time. Its main limitation is that we had all clinical and delivery data related to the control group as referred in the Obstetric reports differing according to the physician attending the consultation or delivery. Data were scarce in the obstetric reports for some data as increase of weight in pregnancy so the number of patients was not adequate to reach a conclusion. Another possibly arguable factor is the low thyroxine dose used in our study22 but nevertheless we achieved the Guidelines recommended level of TSH in the second and third trimester. The late beginning of treatment could be the reason for not being able to reach a significant difference in the abortion rates but we planned our study in a clinical day to day basis.
ConclusionsIn our Endocrinology practice, pregnant women with a TSH in the antenatal screening between 2.5 and 4.9mcU/mL have more induced births and less frequent eutocic deliveries.
We cannot recommend the treatment in the 12th week of our patients with the actual objective of TSH in the second and third trimester because we are unable to get any benefit although we have no adverse events either.
We need a study determining the autoimmunity universally before reaching any conclusion respect to the convenience of treatment in patients with positive thyroid antibodies.
Conflict of interestThe authors declare that we have not received funding for the realization of this work or any conflict of interest
Susana Arribas Dominguez: Secretary of the Service and in charge of the randomization of patients.
Belén Martínez Mondéjar: Preventive Medicine Service. HSO.
Isabel Martínez: Librarian Hospital, Severo Ochoa.