The goal was to evaluate the sentinel node procedure in relation to different pathways of lymphatic drainage and the areas of pelvic lymphadenectomy in patients with prostate cancer assessed by lymphoscintigraphy and SPECT/CT study.
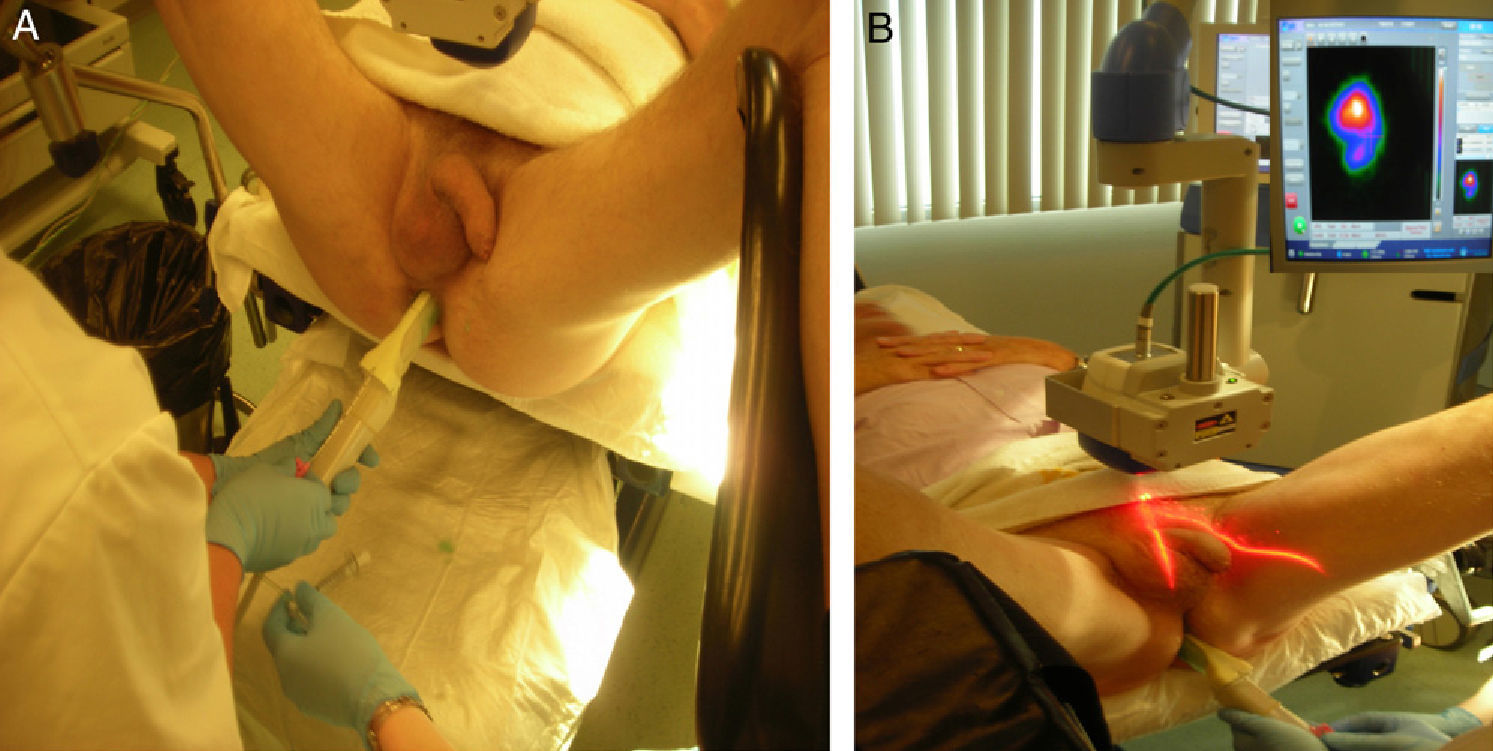
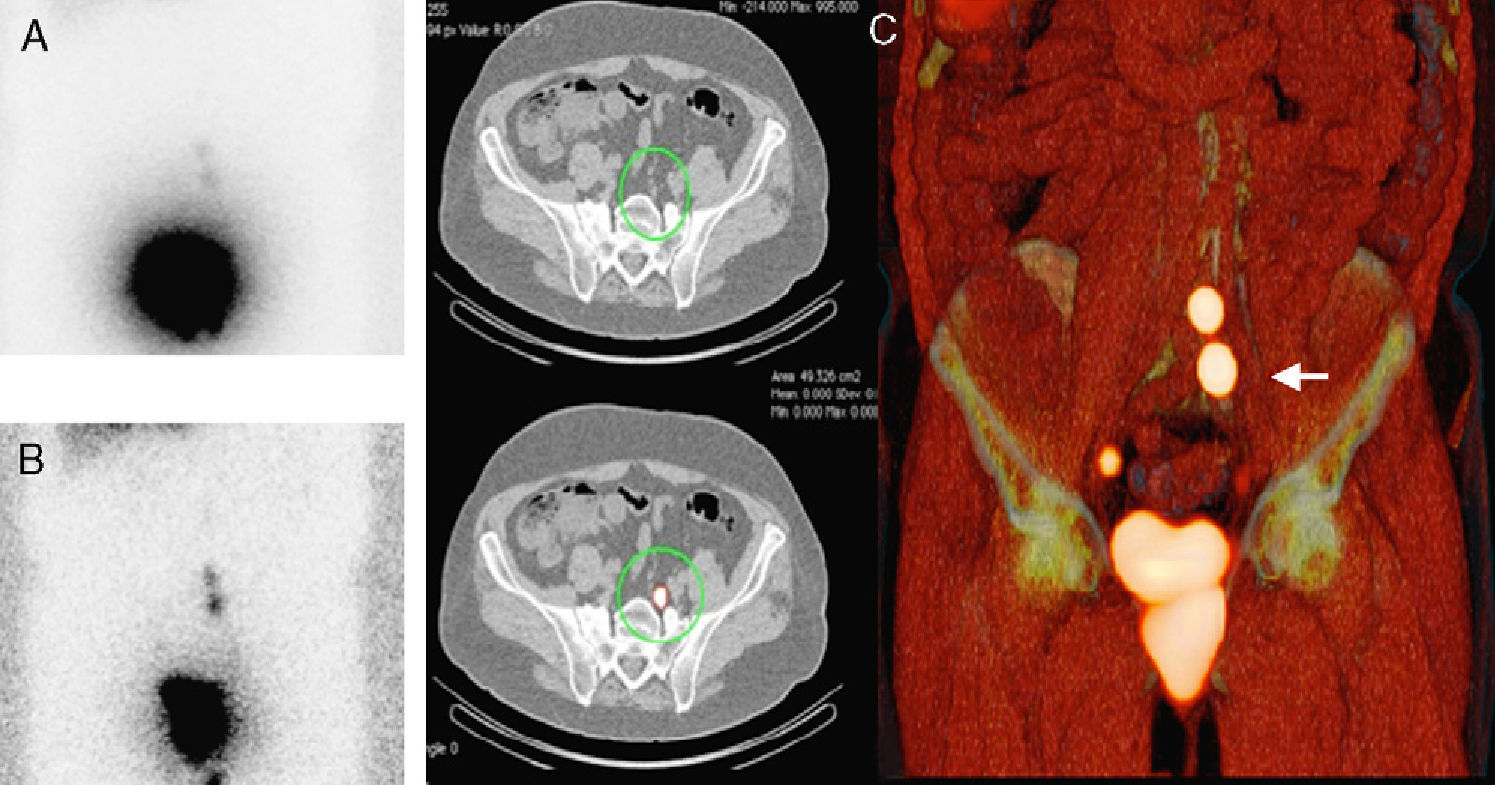
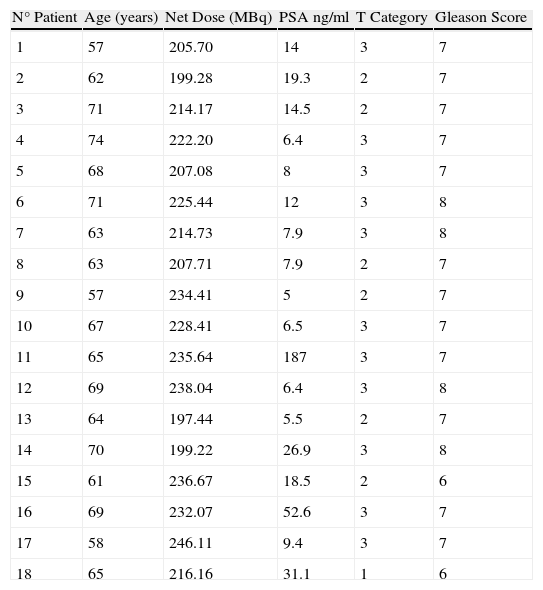
MethodsEighteen patients with prostate cancer of intermediate prognosis were injected with 240 MBq of 99mTc-nanocolloid in the peripheral zone of each quadrant of the prostate, guided by transrectal ultrasonography. Tracer administration was also controlled with a portable gamma camera to assure that there was no diffusion outside the prostate. The injection was followed by planar imaging at 15min. and 2h, performing a SPECT/CT study at 2h. with 2mm slices. On the same day, a laparoscopic sentinel node lymphadenectomy assisted by a gamma probe and a portable gamma camera was performed.
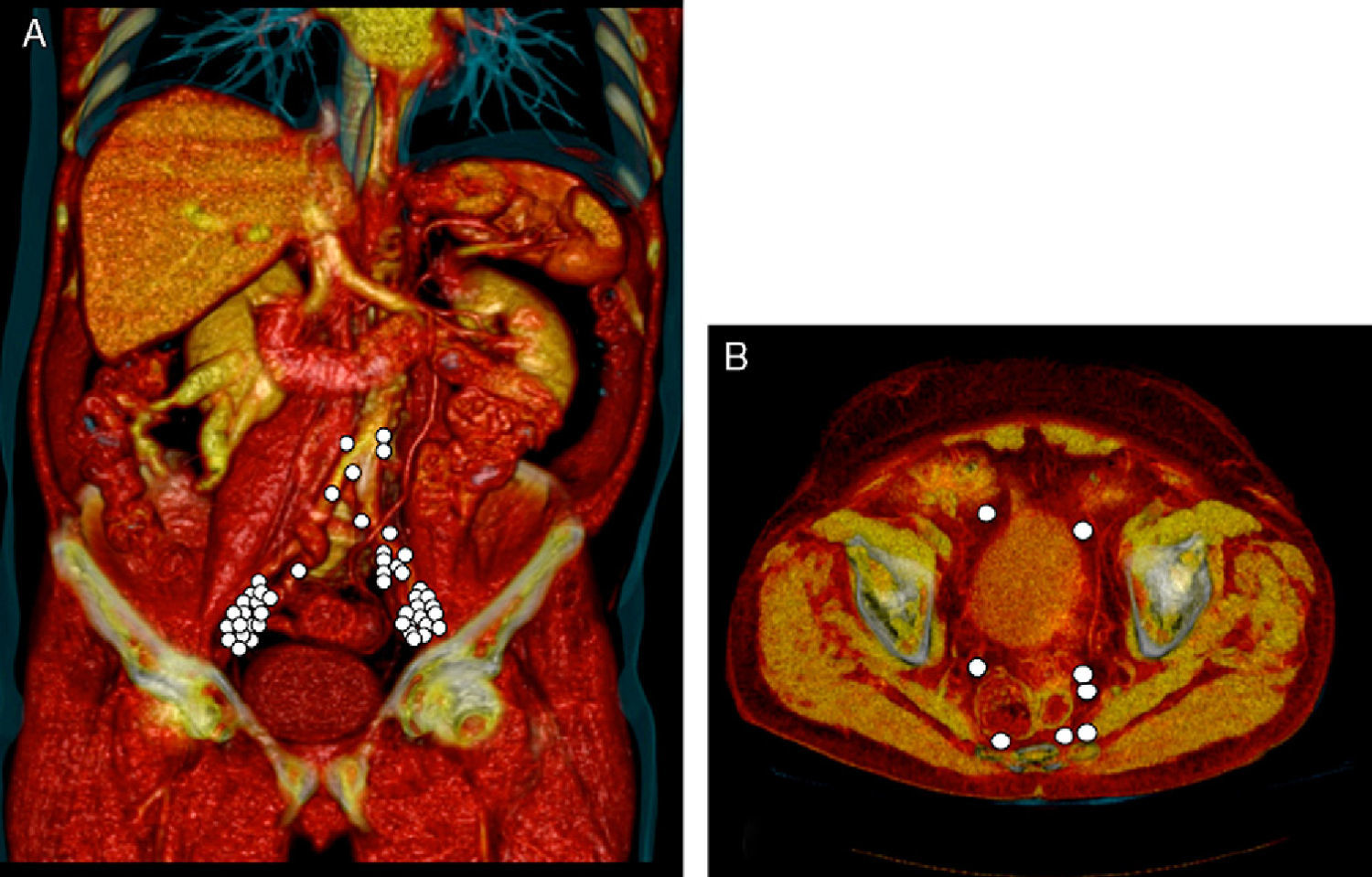
ResultsA total of 55 sentinel lymph nodes (SLNs) were visualized. In 17/18 of patients (94%) SLNs were observed outside the obturator region. Twenty SLNs (36%) were observed along the external iliac artery, 14 in the obturator fossa (25.4%), 6 in internal iliac area (11%) and 4 in common iliac region (7.2%). Three SLNs were visualized in presacral (5.4%), paraaortic (5.4%), and pararectal areas (5.4%) and two in paravesical region (3.6%). SLN metastases were found in 6 patients (33%), and in one of them, a SLN located along the common iliac artery, was the only one with metastases.
ConclusionLymphatic drainage from the prostate has high individual variability, and direct drainage outside the pelvic area is observed frequently. With the SLN procedure, SLNs outside the routine area of lymphadenectomy can also be sampled to stage the patient more accurately.
Valorar la técnica del ganglio centinela en relación con los diferentes patrones de drenaje linfático y con las áreas de linfadenectomía pélvica en pacientes con cáncer de próstata a través de la linfogammagrafía y el SPECT/TAC.
MétodoSe inyectó un total de 240 MBq de 99mTc-nanocoloide divididos en 4 dosis (una para cada cuadarante) mediante control ecográfico transrectal en 18 pacientes con cáncer de próstata con estadio superior a T2b. La inyección también fue controlada con una gammacámara portátil para asegurar que no se producía difusión del trazador fuera de la próstata. Tras la inyección, se realizaron imágenes planares a los 15min y 2h, junto a un SPECT-TAC a las 2h con cortes de 2mm. El mismo día, se realizó la técnica del ganglio centinela vía laparoscopia guiado por una sonda gamma y una gammacámara portátil.
ResultadosUn total de 55 ganglios centinelas (GC) fueron visualizados. En 17/18 de los pacientes (94%) se observaron GC fuera de la fosa obturatriz. Se apreciaron 20 GC a lo largo de la arteria ilíaca externa (36%), 14 en la fosa obturatriz (25,4%), 6 en área de la ilíaca interna (11%) y 4 en la ilíaca común (7,2%). Se localizaron también 3 GC en la región presacra (5,4%), paraórtica (5,4%), y pararrectal (5,4%) y 2 a en región paravesical (3,6%). Se observaron metástasis en el GC en 6 pacientes (33%) y, en uno de ellos, un GC localizado alrededor de la artería ilíaca común fue el único con metástasis.
ConclusiónEl drenaje linfático de la próstata presenta una gran variabilidad individual, y con frecuencia se observan drenajes fuera del área pélvica. Con la técnica del GC, los GC situados fuera del área de rutina de la linfadenectomía pélvica pueden ser extirpados, estadificándose con mayor precisión al paciente.
Article
Revista Española de Medicina Nuclear e Imagen Molecular (English Edition)