To compare the effects of premedication with intravenous paracetamol versus ketorolac, in decreasing intraoperative anaesthetic and postoperative opioid analgesics requirements in patients undergoing laparoscopic cholecystectomy.
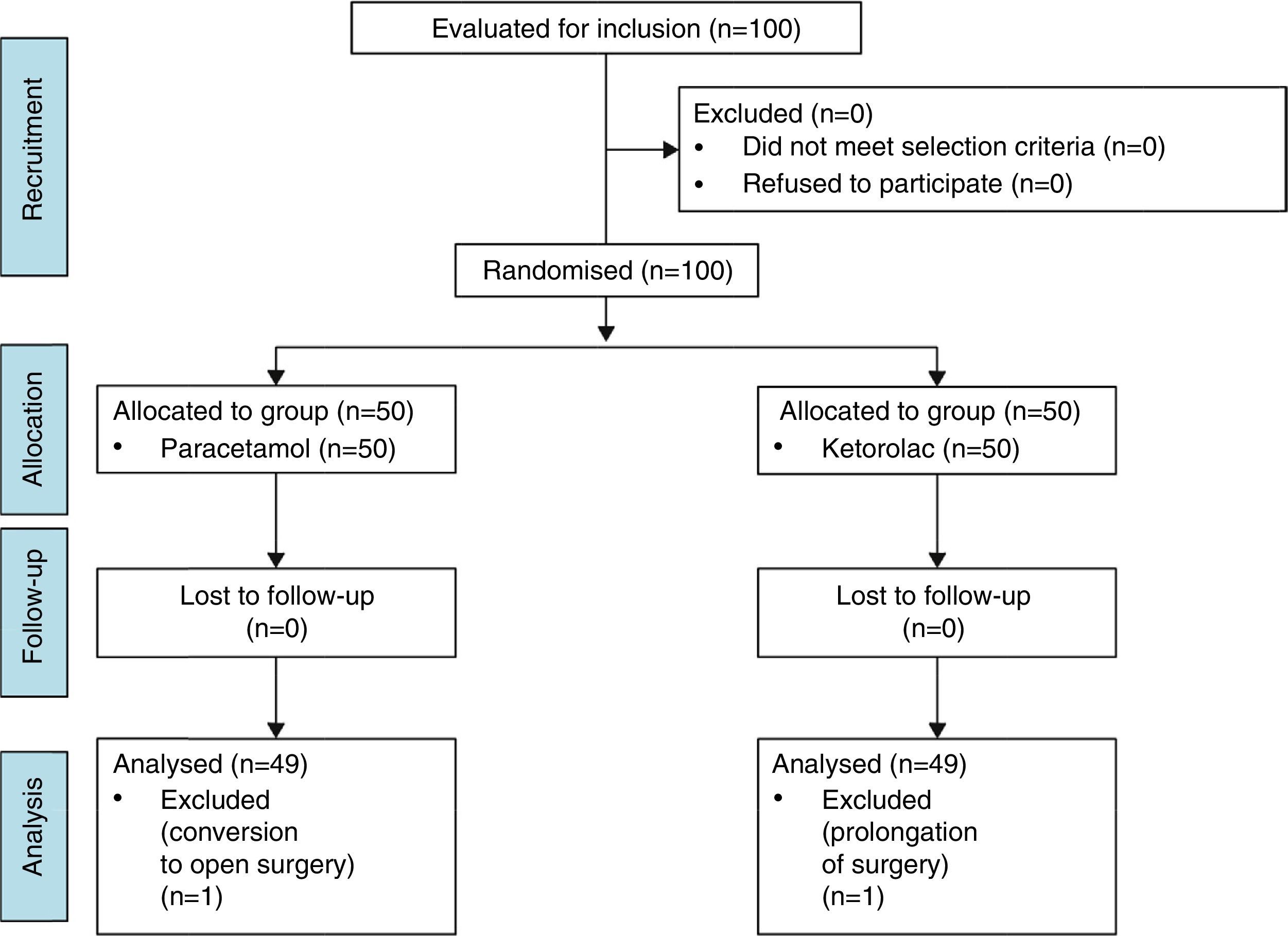
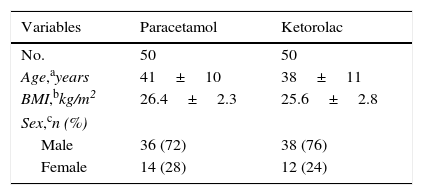
MethodAn experimental, prospective, comparative, double blind, and randomised clinical trial was conducted to determine intraoperative opioid requirements, and pain and analgesic requirements in the postoperative period in 100 healthy patients undergoing laparoscopic cholecystectomy. They were randomised into 2 groups: Group 1: pre-medicated with paracetamol 1g, and Group 2: with ketorolac 30mg (both administered intravenously 30min prior to surgery).
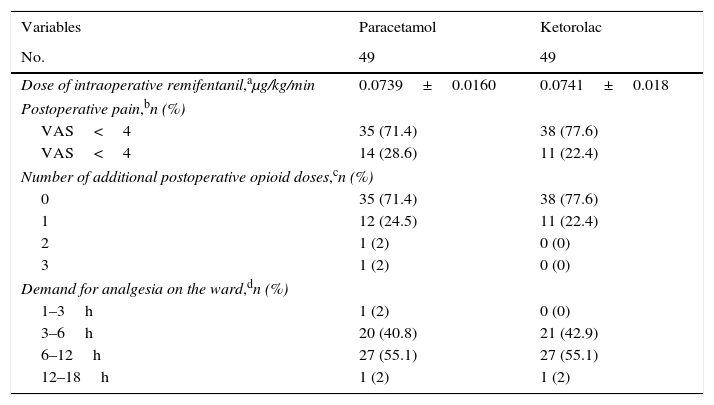
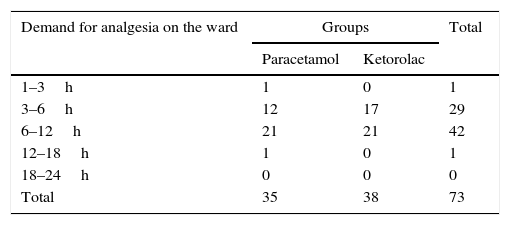
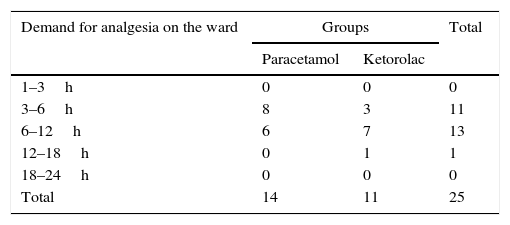
ResultsThere were no statistically significant differences between groups as regards intraoperative remifentanil use (Group 1: 0.0739±0.016μg/kg/min, Group 2: 0.0741±0.018μg/kg/min). The number of patients in Group 2 that had values of VAS>4 points (22.4%) was lower than in Group 1 (28.6%), but with no statistically significant difference. Of the patients who needed postoperative opioid rescue, most required a single rescue and application of analgesics during hospitalisation that prevailed between 3 and 12h, without any significant differences between groups. No adverse effects were observed in the study sample.
ConclusionParacetamol 1g IV given preoperatively decreased anaesthetic requirements and the need for postoperative analgesics similar to the preoperative administration of ketorolac 30mg IV.
Comparar los efectos de la premedicación con paracetamol versus ketorolaco por vía intravenosa en la disminución de los requerimientos anestésicos en el intraoperatorio y la necesidad de analgésicos opioides en el postoperatorio, en pacientes sometidos a colecistectomía laparoscópica.
MétodoEstudio con diseño experimental, prospectivo, comparativo, doble ciego y aleatorizado donde se determinaron los requerimientos opioides intraoperatorios, dolor y requerimientos analgésicos en el postoperatorio en 100 pacientes sanos sometidos a colecistectomía laparoscópica. Se seleccionaron 2 grupos; el grupo 1: se premedicó con paracetamol 1g y el grupo 2: con ketorolaco 30mg; ambos se administraron vía intravenosa 30min previo al acto quirúrgico.
ResultadosNo hubo diferencias estadísticamente significativas entre los grupos con respecto al consumo de remifentanilo intraoperatorio (grupo 1: 0,0739±0,016μg/kg/min; grupo 2: 0,0741±0,018μg/kg/min). El número de pacientes del grupo 2 que presentó valores de EVA>4 puntos (22,4%) fue menor que el del grupo 1 (28,6%), pero sin diferencia estadísticamente significativa. De los pacientes que precisaron rescate analgésico en el postoperatorio, la mayoría ameritó un único refuerzo y la solicitud de analgésicos durante la hospitalización predominó entre las 3 y 12h posteriores, sin diferencias relevantes entre ambos grupos. No se observaron efectos adversos en la muestra estudiada.
ConclusiónParacetamol 1g por vía intravenosa administrado en el preoperatorio disminuyó los requerimientos anestésicos y la necesidad de analgésicos en el postoperatorio con resultados similares a la administración preoperatoria de ketorolaco 30mg por vía intravenosa.