The disease caused by Sars-Cov-2 (Covid-19) has become a worldwide pandemic and consequently a public health problem. Multiple complications associated with Covid-19 have been described, including coagulation abnormalities. Although the infection is known to induce a prothrombotic state, hemorrhagic complications have also been reported in patients with Covid-19, especially in anticoagulated patients. We present two cases of spontaneous pulmonary hematoma in patients with Covid-19 undergoing anticoagulant treatment. We aim to describe this complication, which although uncommon, should be taken into account in anticoagulated patients with Covid-19.
La enfermedad causada por SARS-CoV-2 (Covid-19) se ha convertido en una pandemia mundial y en consecuencia en un problema de salud pública. Se han descrito múltiples complicaciones asociadas a la COVID-19, entre ellas alteraciones de la coagulación. Si bien es conocido que la infección induce un estado protrombótico, también se han descrito complicaciones hemorrágicas en estos pacientes, sobre todo en pacientes anticoagulados. Presentamos dos casos de hematoma pulmonar espontáneo en pacientes con neumonía COVID-19 y terapia anticoagulante. Nuestro objetivo es describir esta complicación, que, aunque poco frecuente, conviene tener en cuenta en pacientes anticoagulados y con COVID-19 concomitante.
COVID-19, the disease caused by SARS-CoV-2, has become a worldwide public health concern. Associated complications include coagulation abnormalities—both thrombotic states and bleeding. Spontaneous pulmonary haematomas are very rare. We have found just one article that has reported a patient who had COVID-19 pneumonia and was undergoing anticoagulant therapy when they developed a haemothorax and an ipsilateral spontaneous pulmonary haematoma.1 In this report, we present two cases of spontaneous pulmonary haematoma in patients with COVID-19 pneumonia undergoing anticoagulant therapy.
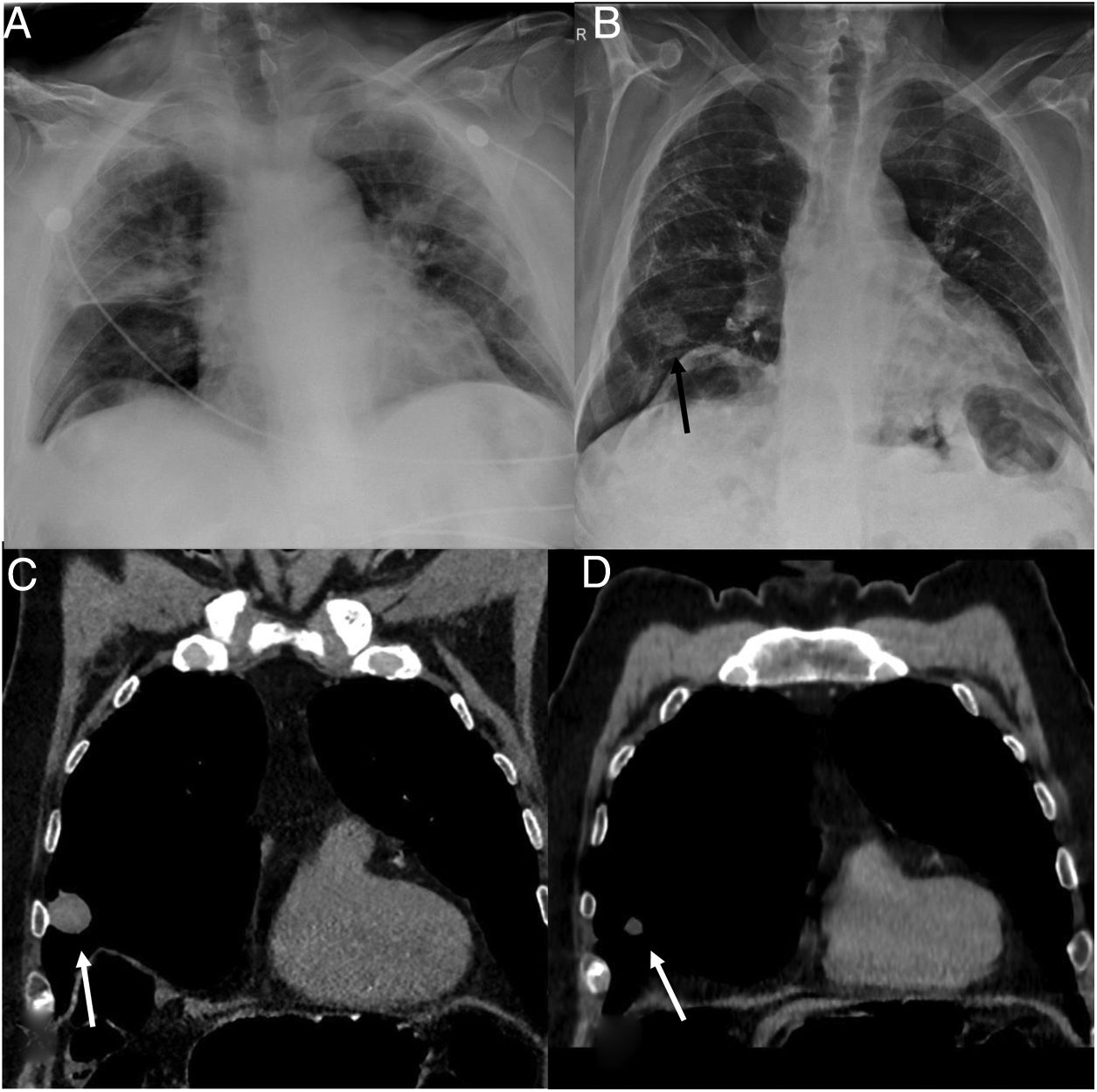
Case reportsIn the first case, a 72-year-old man with a history of hypertension, dyslipidaemia and coronary heart disease was admitted for bilateral COVID-19 pneumonia. A chest radiograph carried out on admission (Fig. 1A) showed bilateral peripheral alveolar involvement. Laboratory tests showed an elevated ferritin level at 439.9 ng/mL, a CRP of 13.11 mg/dl and a D-dimer of 970 ng/mL. The patient presented clinical worsening with increased shortness of breath and a greater need for oxygen (mask with FiO2 of 50%). Treatment commenced with ceftriaxone, azithromycin and corticotherapy with dexamethasone over 10 days and clinical improvement was noted. Given the patient's history of coronary heart disease and the associated elevated thrombotic risk, anticoagulant therapy was initiated using an intermediate dose of enoxaparin (0.5 mg/kg/12 h) in accordance with our hospital’s protocol for patients with COVID-19 pneumonia. The follow-up radiograph taken one week later showed improvement in terms of the bilateral alveolar involvement, and the appearance of a nodule in the right lung (Fig. 1B). Further investigation using a non-contrast chest CT scan (Fig. 1C) revealed a hyperdense 30 mm nodule in the middle lobe (45 HU). We were able to compare this with a chest CT scan from 2017 that showed no focal lesions in the middle lobe. At the time the nodule was detected, the patient had no infectious symptoms in addition to the respiratory insufficiency he was suffering due to COVID-19. Laboratory tests revealed an elevated prothrombin time with a ratio of 1.32 (normal values 0.7–1.2), and the white blood cell count within the normal range. Due to its dense appearance in imaging and its sudden onset in an anticoagulated patient with no clinical and/or laboratory data to suggest a secondary infection, the most likely diagnosis—despite its rarity—is a pulmonary haematoma.
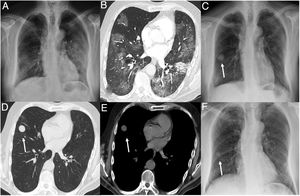
A) Chest radiograph showing bilateral alveolar involvement in relation to COVID-19 pneumonia. (B) Chest radiograph showing improvement of alveolar involvement and the appearance of a pulmonary nodule in the middle lobe (arrow). C) Coronal computed tomography (CT) reconstruction on the mediastinal window setting showing a hyperdense nodule in the middle lobe (arrow). D) Coronal CT reconstruction on the mediastinal window setting of the same patient five months later, with a reduced pulmonary nodule both in size and density (3 HU) (arrow).
Clinical and radiological follow-up was continued, and at five months the nodule had reduced in both size and density (3 HU), indicating that the haematoma was in the process of resolution (Fig. 1D).
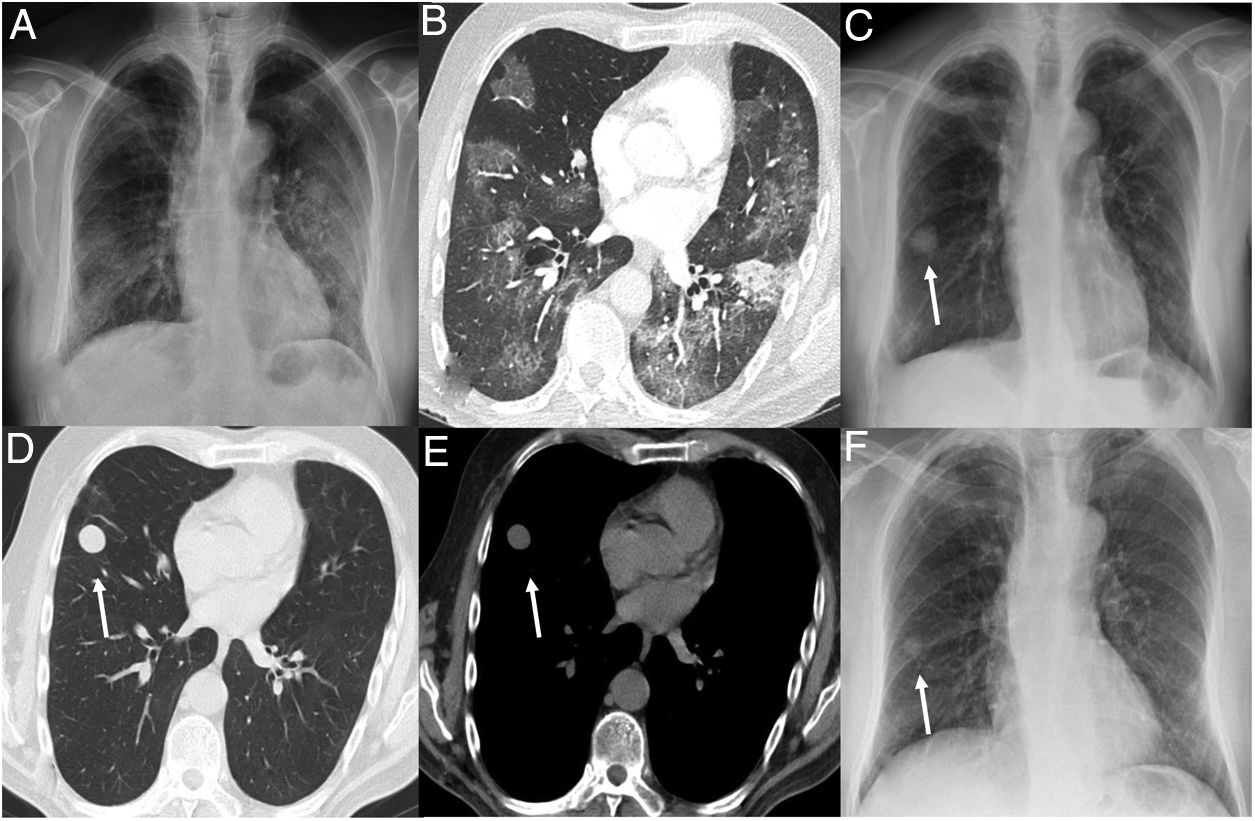
In the second case, a 70-year-old male with no relevant medical history was admitted to our hospital for bilateral COVID-19 pneumonia with severe respiratory insufficiency. The chest radiograph taken on admission (Fig. 2A) shows bilateral alveolar involvement that is predominantly peripheral, and the laboratory tests revealed an elevated ferritin level of 8966 ng/mL and a CRP of 13.40 mg/dl. The patient presented clinical worsening, and the follow-up blood test showed an elevated D-dimer of 15,399 ng/mL. Given the suspicion of pulmonary thromboembolism, a CT angiography of the chest was requested, which showed pulmonary opacities (Fig. 2B) and confirmed pulmonary thromboembolism. Given these findings, anticoagulant therapy was initiated with a full dose of enoxaparin. During hospitalisation, the patient was also administered hydroxychloroquine, azithromycin, ceftriaxone, Kaletra®, tocilizumab and three boluses of methylprednisolone. The patient progressed favourably and was discharged with Sintrom® anticoagulant therapy. One month after discharge, follow-up laboratory tests and a radiograph were performed. The radiograph indicated the appearance of a pulmonary nodule (Fig. 2C) which had not been present in the previous radiographs, nor in the initial CT angiography (Fig. 2A and B). The patient presented no infectious symptoms and the laboratory tests showed normal values in the blood count, CRP and prothrombin time. A chest CT scan showed a well-defined, hypodense (5 HU) nodule measuring 20 mm in the middle lobe (Fig. 2D and E). Clinical and radiological follow-up was conducted, and a steady reduction in the nodule was observed in the follow-up radiograph at 6 months (Fig. 2F). This case involved the sudden onset of a pulmonary nodule despite there being no pre-existing lesions according to the initial CT scan (Fig. 2B) in a patient undergoing anticoagulant treatment, which then went on to spontaneously reduce in size. Therefore, all factors considered, the most likely diagnosis is pulmonary haematoma. The hypodensity of the haematoma in this case can be explained by the fact it was detected in the subacute phase, already in process of resolution.
A) Chest radiograph showing bilateral faint opacities and consolidation in relation to COVID-19 pneumonia. B) Axial computed tomography (CT) image in lung window setting showing bilateral ground-glass opacities and focal consolidation in the left lower lobe. C) Follow-up radiograph one month after hospital discharge showing a smooth-edged nodule in the middle lobe (arrow). D and E) Axial CT images in lung and mediastinal window settings respectively, showing a hypodense pulmonary nodule (5 HU) in the middle lobe (arrow). F) Chest radiograph after six months indicating the reduced size of the pulmonary nodule (arrow).
Pulmonary haematomas are collections of blood in the alveolar and interstitial spaces.2 They are most commonly caused by chest trauma which results in a ruptured pulmonary vessel with subsequent bleeding.2 Spontaneous haematomas are very rare and may be induced by anticoagulant therapy, thrombocytopenia or disorders affecting the connective tissue such as Ehlers-Danlos syndrome.3,4 They generally occur because of bleeding from previous lesions in the lung parenchyma, such as bullae, emphysema, cysts or pneumatocele, or may be secondary to angionecrosis and the erosion of lesional walls with subsequent bleeding.4–6 Spontaneous pulmonary haematomas with no pre-existing pulmonary lesion, as in our two cases, are extremely rare.2
Pulmonary haematomas are usually asymptomatic and are diagnosed as a result of incidental findings on imaging tests. When symptoms are present, they are usually accompanied by haemoptysis.3,7
On CT, a pulmonary haematoma in its acute phase appears as a hyperdense nodule or mass with well-defined margins which decreases in size and density over time,8 thus explaining the hypodensity of the haematoma in our second case. Magnetic Resonance Imaging (MRI) can be useful in ambiguous cases to differentiate between a haematoma and a pulmonary neoplasm, as haematomas in the acute stage are hyperintense on T1-weighted images and there is no contrast enhancement.8
As these lesions resolve spontaneously within weeks or months, treatment is usually conservative if there are no complications.3
Treatment in both asymptomatic patients consisted of clinical-radiological monitoring, which revealed a progressive reduction of the haematomas in the follow-up radiographs.
In conclusion, although spontaneous pulmonary haematomas are very rare, two cases have been reported in our hospital in anticoagulated COVID-19 patients. In the new COVID era, the sudden onset of a pulmonary nodule in an anticoagulated COVID-19 patient should prompt us to consider this entity.
Authors- 1
Research coordinators: CL
- 2
Development of study concept: CI, EC
- 3
Study design: CL
- 4
Data collection: CL
- 5
Data analysis and interpretation: CL, EC, AG, MA
- 6
Statistical processing: CL
- 7
Literature search: CL
- 8
Article authors: CL
- 9
Critical review of the manuscript with intellectually relevant contributions: CL, EC, AG, MA
- 10
Approval of the final version: CL, EC, AG, MA
The authors declare that they have no conflicts of interest.