There is a lack of quantitative measures of the quality of alveolar trabecular bone, an important factor in implantology. This study aimed to develop a method of objectively assessing the quality of trabecular bone by means of image processing and structural analysis of multidetector computed tomography images and to establish differences between tooth types and tooth presence/absence.
Materials and methodsWe analysed 20 patients who underwent multidetector computed tomography to evaluate mandibular bone and tooth positioning. Image analysis included automatic segmentation of the mandible, obtainment of sections perpendicular to the dental arch, and structural analysis of the trabecular bone in each section. We calculated the ratio between the volume of bone and the total volume of the section, the thickness, the trabecular number, and the mean attenuation in Hounsfield units. We analysed the differences among different tooth types (incisors, canines, premolars, and molars) and between present and absent teeth.
ResultsWe found statistically significant differences between different tooth types and between sections in which teeth were present or absent. Incisors had a greater ratio of trabecular bone; the ratio of trabecular bone progressively decreased from the incisors to the canines, premolars, and molars. The ratio of trabecular bone was greater in sections in which teeth were absent than in those in which teeth were present.
ConclusionsThe method allows to quantify the structural properties of alveolar bone from multidetector computed tomography images. Our results provide an objective picture of the bone substrate that can be useful for planning and following up dental implant procedures.
Existe una carencia de métricas cuantitativas de la calidad del hueso trabecular alveolar, factor determinante en implantología. El objetivo de este estudio es desarrollar una metodología con tomografía computarizada multidetector para objetivar la calidad del hueso trabecular y establecer diferencias entre los distintos tipos y el estado de las piezas dentarias mediante procesado de imágenes y análisis estructural.
Materiales y métodosSe analizan 20 pacientes con exploración de tomografía computarizada multidetector dental para la valoración del hueso mandibular y posiciones dentales. El análisis de las imágenes incluyó la segmentación automática de la mandíbula, obtención de secciones perpendiculares a la arcada dentaria y análisis estructural del hueso trabecular de cada sección. Se obtuvieron la ratio entre volumen de hueso y volumen total de la sección, el grosor, la separación y el número trabecular, y la atenuación promedio en unidades Hounsfield. Se analizaron diferencias entre tipos de diente (incisivos, caninos, premolares y molares) y entre estados de las piezas dentarias (ausente o presente).
ResultadosSe obtuvieron diferencias estadísticamente significativas entre los tipos y estados de las piezas. Por tipo, los incisivos mostraron mayor ratio de hueso trabecular, con disminución progresiva para caninos, premolares y molares. Por estado, las secciones pertenecientes a dientes ausentes presentaron mayor ratio de hueso que con el diente presente.
ConclusionesLa metodología desarrollada permite cuantificar las propiedades estructurales del hueso alveolar a partir de imágenes de tomografía computarizada multidetector. Los resultados obtenidos objetivan el estado del sustrato óseo de cara a la planificación y seguimiento de la colocación de implantes dentales.
The use of dental implants as fixtures to support tooth restoration in cases of tooth loss or absent teeth is a treatment applied in routine practice where radiology plays an essential role.1 However, in spite of the now generalised use of this type of treatment and the increasing use of immediate load implants, there is a lack of quantitative metrics to help predict the prognosis of the implants according to the quality of the recipient bed, which is a determining factor for stability.2–5 Consequently, the elements that define bone quality (mechanical properties, microarchitecture, degree of mineralisation, composition, remodelling capacity and osseointegration time required) are interpreted according to individual experience or using subjective scales,6,7 which in some cases determines the type of implant and prosthodontic restoration without a sufficient amount of objectivity.8
The surgical techniques used in current implantology are increasingly complex and require precise information for planning interventions and predicting the outcome of the implant, especially when immediate-loading implants are being used.9,10 Computed tomography (CT), either multidetector (MDCT) or cone beam (CBCT), combined with advanced image-processing techniques and computational mechanical simulation, opens up new avenues of application which are of great assistance for structural and biomechanical assessment of mandibular behaviour prior to any surgical procedure.11
In recent years, great advances have been made in CBCT in the field of dental radiology, and it now provides image quality similar to MDCT, but with a much lower radiation dose. This study focuses on MDCT images due to the availability in our centre, but the computational analysis methods and the quantitative parameters which can be obtained are also extractable from CBCT images.
Although there are some commercial diagnostic programmes based on the reading and visualisation of CT images and the planning of implants, such as Simplant (Dentsply Sirona, USA) or Med 3 D (med3D GmbH, Germany), there are no decision-support tools that provide detailed and objective information on the structural state of the recipient bed.
Correct segmentation of the structures of the mandible makes it possible to analyse and quantify its different properties, thereby enabling us to determine the quantity and quality of the bone. In addition, a three-dimensional virtual model can be generated in order to perform accurate, reliable biomechanical simulations. Last of all, we can also obtain stereolithographic geometry that is directly exportable to 3D printers which facilitates subsequent surgical interventions.12,13
Our hypothesis is that the mandibular alveolar bone can be characterised with the combination of MDCT acquisitions and medical imaging post-processing techniques based on segmentation, filtering and structural analysis of bone tissue. This information will then serve as a basis for further mechanical simulations of the bone and will potentially be of use for decision making and planning in dental implantology.
Our aim is to develop a new methodology combining image processing techniques and structural analysis to objectify the quality of trabecular bone and establish the differences between the different types of teeth and whether they are present or absent.
Material and methodsPatientsWe retrospectively reviewed the MDCT scans performed in 2017 at our centre in which assessment of the mandibular bone and teeth position was requested. We obtained an initial sample of 30 patients with dental MDCT images. We excluded patients whose images had metallic artefacts which were obviously going to cause difficulties for adequate recognition of the anatomical structures to be segmented. Ultimately, 20 patients were included in the study (40±17 years, 7 men and 13 women).
All the patients gave written consent for the use of their images, which were made duly anonymous in the study. The study was approved by our institution's Independent Ethics Committee.
Image acquisitionThe examinations were carried out using a 64-slice multidetector system (Brilliance, Philips Healthcare, Best, The Netherlands). The acquisition protocol used a voltage of 120kV and an intensity of 60mA, with a spatial resolution of the reconstructed image of 0.3mm×0.3mm×0.3mm.
Analysis of the imagesThe post-processing methodology for the images included three steps: segmentation of the jaw, orthopantomographic angular projection and structural analysis of the bone. Each of these steps is described below. All the image analysis was performed using the Matlab program (R2017a, The Mathworks Inc., USA).
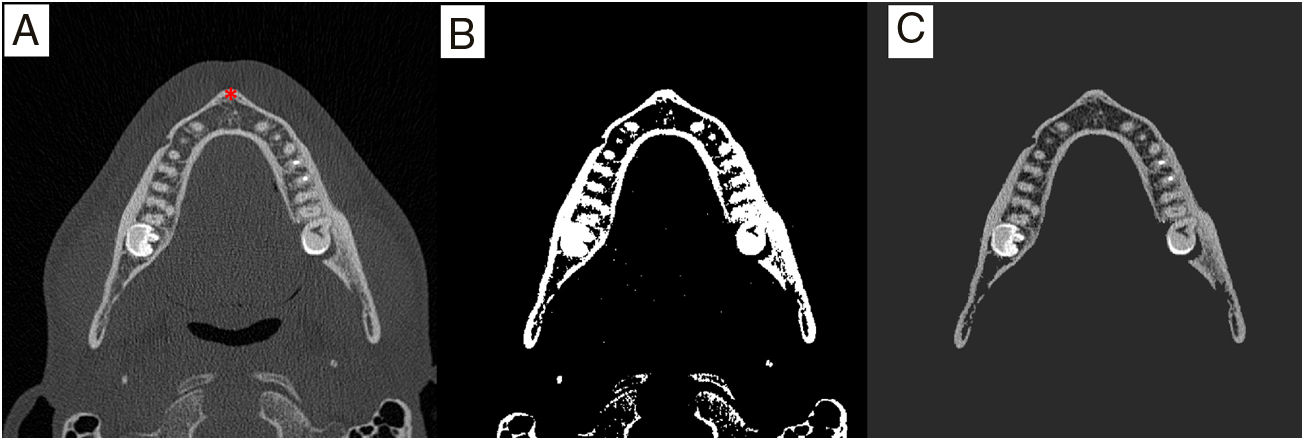
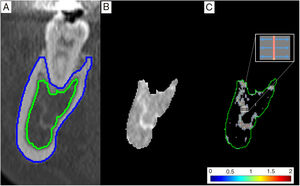
Segmentation of the mandibleBone segmentation was performed by merging several different methods of image processing (Fig. 1). First, thresholding was applied using Otsu's histogram-based method,14 from which two masks were obtained, one associated with high densities (bone, teeth and implant if any) and another at low densities (soft tissue and air).
Next the 3D region growing method15 was applied, taking the cortical bone of the mandible as initial seed. With this method, connected structures which have similar attenuation values can be segmented and a binary mask obtained. Various morphological filling, dilation and erosion operations were performed on the mask in order to include the cancellous alveolar bone.
Angular orthopantomographic viewThe orthopantomographic view is a multiplanar reconstruction which provides a maximum intensity projection of the dental arch on a two-dimensional plane.
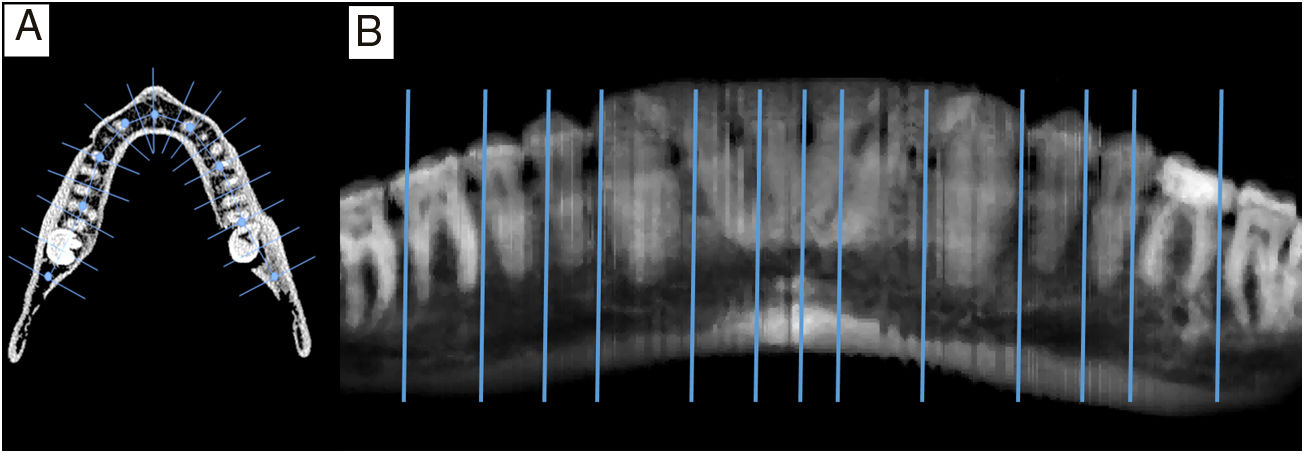
To make this projection, a spline curve was defined from several control points following the curvature of the dental arch. A series of planes perpendicular to the curve of the arch was then obtained automatically, cutting the mandible at each of the points of the spline, with a thickness of 0.3mm and a space between planes of 1mm. Last of all, an image was obtained projecting the maximum intensity of each of the perpendicular planes onto a two-dimensional image (Fig. 2).
Orthopantomographic angular reconstruction. (A) Definition of the spline-type line with nine reference points and example of some perpendicular sections. (B) Angular reconstruction as a maximum intensity projection of the sections perpendicular to the curve of the arch. Also shown is an example of reference lines that separate the sections of bone associated with each tooth space.
To perform the structural analysis of the trabecular alveolar bone, the compact cortical bone and teeth, previously segmented as high density masks, were excluded.
Next, both the original images and the orthopantomographic view were used to identify and manually establish the starting slices for each tooth (Fig. 2). These starting slices defined small individual volumes (sets of slices) of alveolar bone associated with each tooth space, which facilitated individual analysis and grouping by type and status. Each tooth was numbered following the universal dental numbering system (17–32) and coded as incisor, canine, premolar or molar. The following were defined as possible statuses: tooth present, tooth absent or implant.
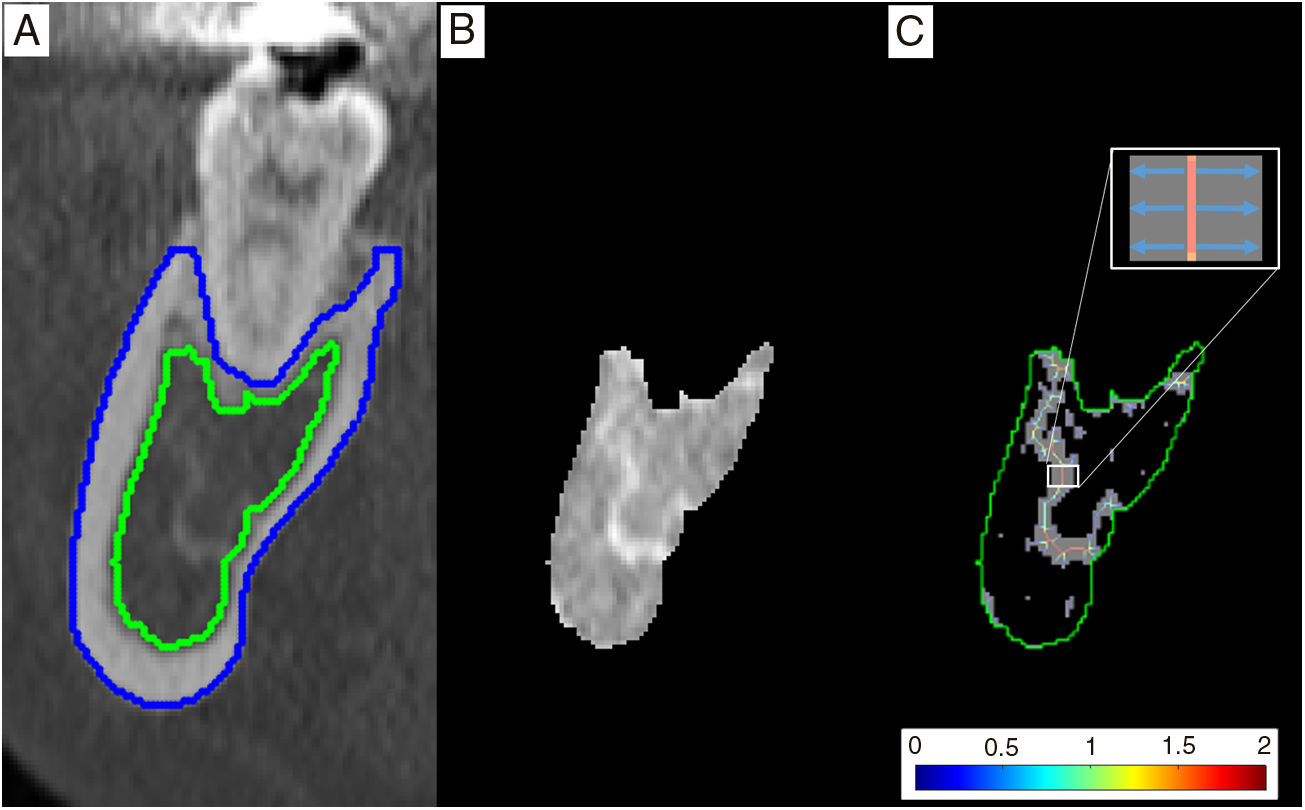
For each slice of alveolar bone a new Otsu thresholding calculation was applied, allowing us to obtain a binary image of the bone trabeculae (Fig. 3).
Trabecular analysis. (A) Section of the mandible perpendicular to the line of the arch, in which the segmentation of the cortex (blue) and cancellous bone (green) of the mandible can be seen. (B) Section containing only cancellous bone. (C) Binarised image showing the trabecular bone (grey) with the structural line of the skeleton overlaid, colour-coded according to the trabecular thickness (in millimetres). The detail indicates that for each central point of the skeleton the distance to the edge of the trabecula is measured. The trabecular separation is obtained analogously, taking the structural line of the bone marrow, i.e. the image complementary to that of the trabecular bone.
Additionally, to ensure an implant dentistry-orientated approach, the position of the dental canal was also defined in order to analyse the volume above the canal separately.
We calculated the following parameters and their means for each set of slices representative of a tooth space (entire and above the canal):
- •
Bone-volume-to-total-volume (BVTV) percentage.
- •
Mean trabecular thickness (TbTh).
- •
Mean trabecular separation (TbSp).
- •
Trabecular number (TbN) defined as BVTV/TbTh.
- •
Mean value for the bone in Hounsfield units (TbHU).
To assess the differences between groups of teeth (incisors, canines, premolars and molars) an ANOVA was performed with a Bonferroni post hoc test for homogeneity of variances. Absent teeth and implants were excluded from this analysis.
The study of the differences between tooth statuses (present, absent or implant) was also performed with ANOVA and Bonferroni post hoc tests for homogeneity of variances. In this case, independent analyses were performed for each of the four groups of teeth.
All the statistical tests were performed for the two sets studied: entire alveolar volumes and above-the-canal volumes. A p value <0.05 was considered statistically significant. The statistical analysis used the SPSS software program (v22, IBM, USA).
ResultsWe studied a total of 291 volumes associated with tooth spaces. Of these, 80 corresponded to incisors (73 teeth present and 7 absent), 40 to canines (all present), 80 to premolars (69 present, 8 absent and 3 implants) and 91 to molars (78 present, 9 absent and 4 implants). In view of the small number of cases, the values associated with implant spaces were excluded from the comparative statistical tests.
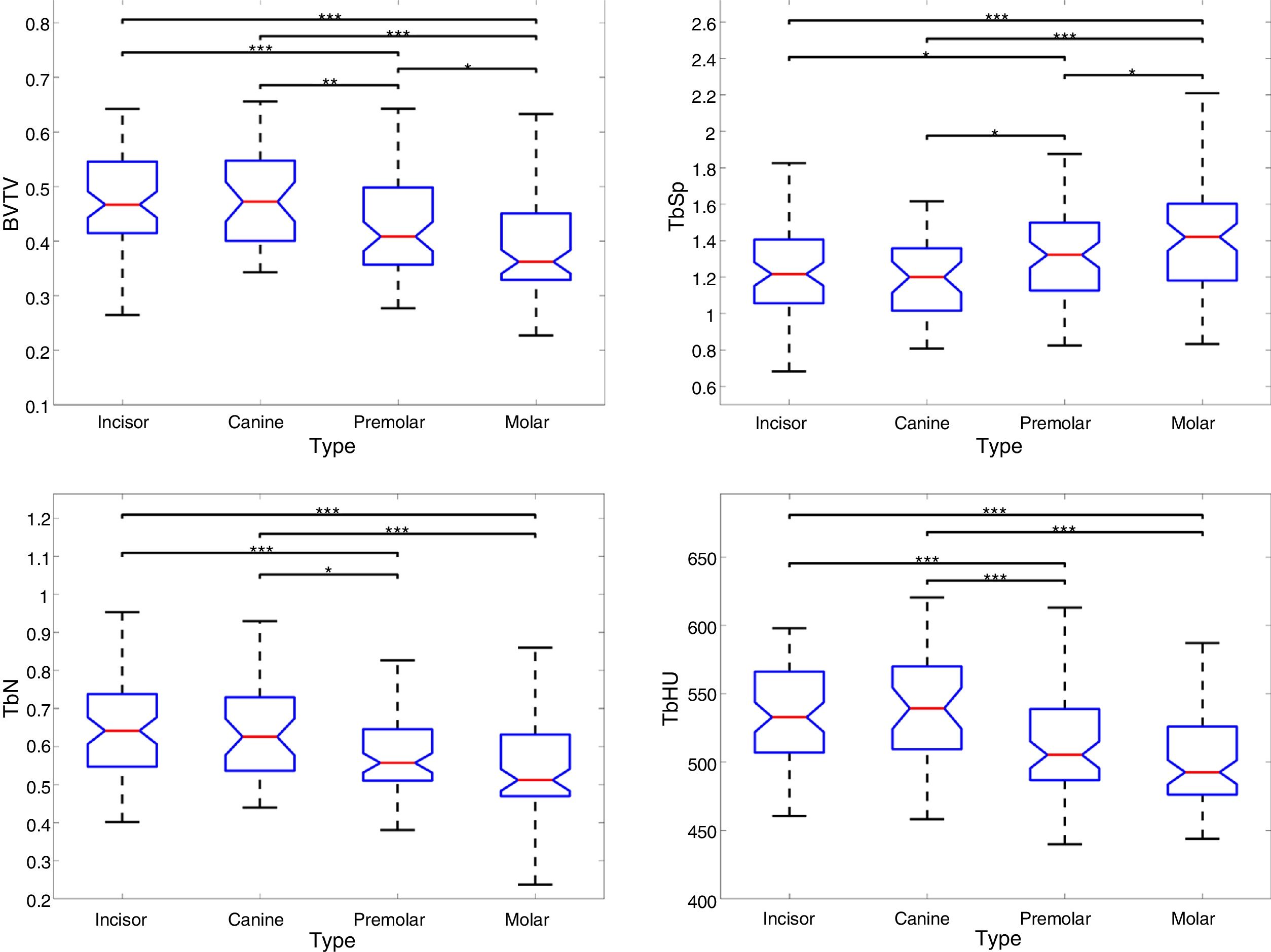
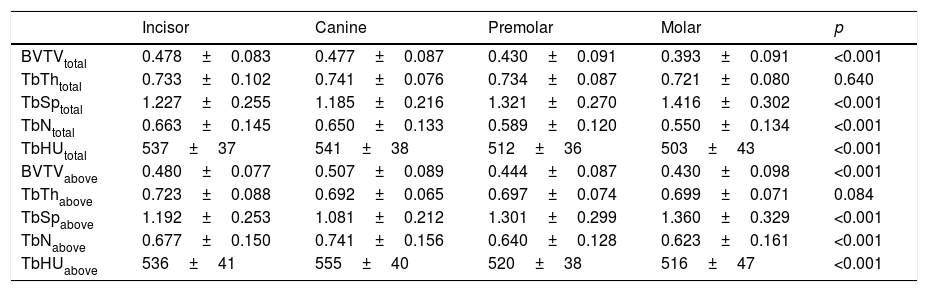
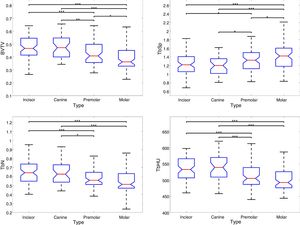
The analysis by tooth type revealed statistically significant differences for the bone-volume-to-total-volume (BVTV) ratio, trabecular separation (TbSp), trabecular number (TbN) and average HU value (TbHU), both for the entire volumes and above-the-canal volumes (Table 1 and Fig. 4). No significant differences were found for trabecular thickness (TbTh). In general, the observed differences were of small magnitude and showed a linear variation from interior to exterior, with incisors and canines having higher bone density (higher bone volume ratios, greater trabecular number, higher mean HU and lower trabecular separation values) than premolars and molars.
Results of the parameters studied for each tooth group (considering only those in which the teeth were present) for the total alveolar volume and for the portion of alveolar volume above the dental canal.
| Incisor | Canine | Premolar | Molar | p | |
|---|---|---|---|---|---|
| BVTVtotal | 0.478±0.083 | 0.477±0.087 | 0.430±0.091 | 0.393±0.091 | <0.001 |
| TbThtotal | 0.733±0.102 | 0.741±0.076 | 0.734±0.087 | 0.721±0.080 | 0.640 |
| TbSptotal | 1.227±0.255 | 1.185±0.216 | 1.321±0.270 | 1.416±0.302 | <0.001 |
| TbNtotal | 0.663±0.145 | 0.650±0.133 | 0.589±0.120 | 0.550±0.134 | <0.001 |
| TbHUtotal | 537±37 | 541±38 | 512±36 | 503±43 | <0.001 |
| BVTVabove | 0.480±0.077 | 0.507±0.089 | 0.444±0.087 | 0.430±0.098 | <0.001 |
| TbThabove | 0.723±0.088 | 0.692±0.065 | 0.697±0.074 | 0.699±0.071 | 0.084 |
| TbSpabove | 1.192±0.253 | 1.081±0.212 | 1.301±0.299 | 1.360±0.329 | <0.001 |
| TbNabove | 0.677±0.150 | 0.741±0.156 | 0.640±0.128 | 0.623±0.161 | <0.001 |
| TbHUabove | 536±41 | 555±40 | 520±38 | 516±47 | <0.001 |
BVTV: bone volume-to-total volume ratio (as a decimal fraction); TbTh: mean trabecular thickness (mm); TbSp: mean trabecular separation (mm); TbN: trabecular number (mm−1); TbHU: mean Hounsfield unit (HU) value. The values are expressed as mean±standard deviation.
Box diagrams showing the differences between tooth groups for each of the parameters studied. For simplicity, only the results for the entire alveolar volume are shown, as the results for the portion of volume above the canal are similar.
BVTV: bone volume-to-total volume ratio (as a decimal fraction); TbSp: mean trabecular separation (mm); TbN: trabecular number (mm-1); TbHU: mean Hounsfield unit (HU) value. The number of asterisks indicates statistical significance below 0.05 (*), 0.01 (**) and 0.001 (***).
Comparing entire volumes and above-the-canal volumes, the results showed no statistically significant differences, so the analysis of differences by tooth status was performed only for entire volumes of trabecular bone.
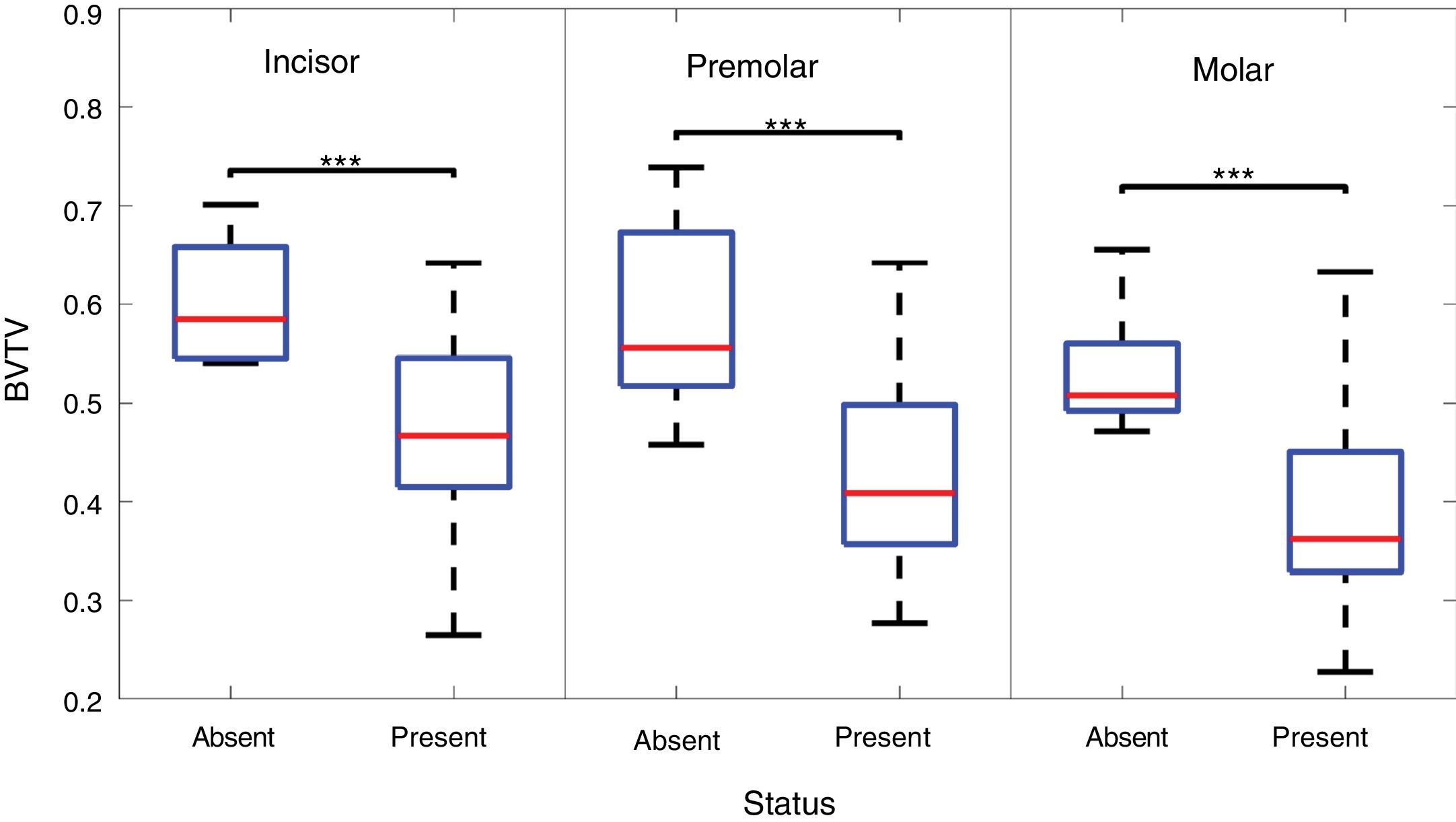
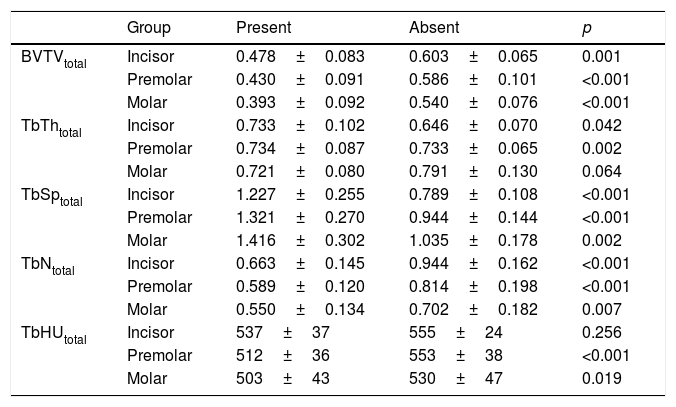
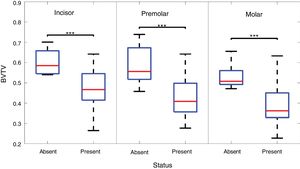
By tooth status, the relative bone volume associated with teeth which were present was lower than in the case of absent teeth (Table 2 and Fig. 5). A similar pattern was found for the other parameters. We should point out that in the canine group all the teeth were present in all cases, so canines were not included in the analysis.
Results of the parameters studied according to the presence or absence of each tooth for each group of teeth for the total alveolar volume. The canine group is excluded for not having absent teeth.
| Group | Present | Absent | p | |
|---|---|---|---|---|
| BVTVtotal | Incisor | 0.478±0.083 | 0.603±0.065 | 0.001 |
| Premolar | 0.430±0.091 | 0.586±0.101 | <0.001 | |
| Molar | 0.393±0.092 | 0.540±0.076 | <0.001 | |
| TbThtotal | Incisor | 0.733±0.102 | 0.646±0.070 | 0.042 |
| Premolar | 0.734±0.087 | 0.733±0.065 | 0.002 | |
| Molar | 0.721±0.080 | 0.791±0.130 | 0.064 | |
| TbSptotal | Incisor | 1.227±0.255 | 0.789±0.108 | <0.001 |
| Premolar | 1.321±0.270 | 0.944±0.144 | <0.001 | |
| Molar | 1.416±0.302 | 1.035±0.178 | 0.002 | |
| TbNtotal | Incisor | 0.663±0.145 | 0.944±0.162 | <0.001 |
| Premolar | 0.589±0.120 | 0.814±0.198 | <0.001 | |
| Molar | 0.550±0.134 | 0.702±0.182 | 0.007 | |
| TbHUtotal | Incisor | 537±37 | 555±24 | 0.256 |
| Premolar | 512±36 | 553±38 | <0.001 | |
| Molar | 503±43 | 530±47 | 0.019 |
BVTV: bone volume-to-total volume ratio (as a decimal fraction); TbTh: mean trabecular thickness (mm); TbSp: mean trabecular separation (mm); TbN: trabecular number (mm−1); TbHU: mean Hounsfield unit (HU) value. The values are expressed as mean±standard deviation.
Box diagrams showing the differences between tooth status for incisors, premolars and molars. The bone-volume-to-total-volume (BVTV) ratio alone is shown as a representative parameter. The number of asterisks indicates statistical significance below 0.05 (*), 0.01 (**) and 0.001 (***).
There were no statistically significant differences between men and women.
DiscussionIn this study we developed a new complete method for the processing of dental MDCT images which allows us to segment, analyse and objectify the state of the trabecular alveolar bone structure in the lower jaw. Differences have been established between different tooth types (incisors, canines, premolars and molars) and statuses (present or absent) for the parameters bone-volume-to-total-volume ratio, trabecular thickness and density, trabecular number and mean HU value. The results showed that incisors and canines had a higher bone density, considered as the ratio of trabecular bone, than premolars and molars. Moreover, the alveolar bone of absent teeth also showed a higher trabecular density than when the tooth was present. These results represent an advance in the quantitative approach to bone assessment, which has traditionally been based on the application of qualitative scales.6,7
Computed microtomography (micro-CT) is a CT technique which allows the study of small animals or ex vivo tissue samples with very high spatial resolution (in the order of microns). Taking it as a histomorphometric reference pattern, the results for the relative bone volume obtained in this study are in the range of those obtained in cadaver mandibles.16–18 When compared with these studies, however, our thickness and trabecular separation values are higher, in fact approximately double. These differences may be due to partial volume in the MDCT, as the resolution of the studies with micro-CT was less than 50μm (isotropic voxel).
In the Ebrahim et al. study19 with CBCT, the relative bone volume, density and trabecular separation values are in the same range as those obtained in our study. Another study that also used CBCT showed slightly lower values for these parameters.20 The resolution used in these studies was around 100μm (isotropic voxel).
One study which used micro-MRI in cadaver samples21 obtained similar results to those presented by the Lee group16 for micro-CT. In this case, a resolution of 110μm was used, with a slice thickness of 600μm. It should be mentioned that they also observed structural differences between incisors, premolars and molars, although only for the anisotropy of the trabecular structure.
It would therefore seem that the relative bone volume values obtained with MDCT are similar to those of micro-CT. However, both the trabecular thickness and the separation between trabeculae are overestimated, in some cases by a factor of two. Comparing MDCT and CBCT, the differences between the techniques are not evident in terms of image quality, definition of structures and structural analysis of the alveolar bone, with disparate results.22–25 Future studies should therefore also apply and validate the methodology proposed in this study in longitudinal studies (pre- and post-implant) with CBCT, given the routine use of this technique in dental imaging scans.
We found very few studies which analysed the trabecular alveolar bone according to tooth type; that of Choël et al.,21 mentioned above, and those of Almasoud et al.5 and Park et al.,26 in which relative differences between tooth types similar to those obtained in our study were found in mean HU values, with a decreasing gradient from incisors to molars. These studies showed the opposite behaviour for the density in the mandibular cortex, i.e. an increasing gradient from incisors to molars, associated with mandibular mechanical/biological properties.27
In our study we found that the bone ratio for alveolar spaces without teeth was higher. It is known that a bone resorption process takes place after the loss of a tooth, with gradual decrease in volume in the area of mandible exposed. This process is variable and depends on multiple factors, such as age, gender, metabolism, oral hygiene and length of time since the tooth was lost.28 Our results could be explained by the increase in trabecular bone during the trabecular restructuring process to compensate for the loss of bone mass and so maintain the stability of the mandible within the overall process of atrophy.29
The results obtained in our study provide the basis for advanced biomechanical analysis of the mandible to support the planning and placement of dental implants, and aid post-implant follow-up.30
One limitation of this study is the marked difference in the numbers of cases associated with each tooth status. In the study sample, we were only able to analyse the volumes of 24 spaces where the tooth was absent, compared to a total of 260 volumes where the tooth was present. Moreover, in some of the alveolar bone volumes associated with absent teeth, there may be a marked bone resorption process, with the consequent loss of bone mass. In these cases, the automatic segmentation and the separation between trabecular bone and marrow by thresholding was not as precise as in the presence of normal alveolar bone, making it necessary to apply some manual corrections. Future studies will need to expand the patient series to include a more representative sample size for absent teeth and implants and improve automatic segmentation. Age ranges higher than those in this study and other factors which can affect bone resorption/remodelling, such as time since tooth loss, presence of periodontal disease or other iatrogenic, genetic, mechanical, vascular or hormonal factors should also be taken into account.
This study focused on analysis of the mandible because of the greater ease in automatic segmentation. The study of the maxilla is more complex due to the presence of other facial bones, which probably makes it necessary to manually specify some starting slices to facilitate segmentation. The planning and placement of implants also involve greater difficulty, because of the proximity of the maxillary sinus and the lower bone density compared to the mandible.31
In our series, a number of studies which had metallic artefacts were not included. There are filters based on iterative methods which help to significantly reduce such artefacts and which can be integrated automatically into workflows.32,33 These filters can also be combined with other super-resolution filters to improve the detail of the structures.34
In our study, no significant differences were found between the results for the entire alveolar bone and the bone above the canal, probably due to the fact that they have similar microarchitecture. However, it may be important to take this separation into account in the planning and placement of dental implants. We defined the location of the dental canal manually in this study, but there are methods for doing it automatically.35
ConclusionsThe methodology developed in this study makes it possible to quantify the structural properties of the trabecular alveolar bone of the lower jaw from MDCT images. We found overall differences between different tooth types and states, with excellent precision for the bone-volume-to-total-volume ratio, but less reliability for the other parameters. Nonetheless, these results need to be expanded on with a larger sample of patients with absent teeth and patients with implants, taking other factors which affect bone resorption/remodelling into account. The results we obtained are useful for objectifying the state of the bone substrate in the planning and monitoring of dental implant placement.
Authorship1. Responsible for the study as a whole: RSR.
2. Study conception: VHB, RSR, LMB and MB.
3. Study design: VHB, RSR and LMB.
4. Data acquisition: VHB, RSR and ATE.
5. Analysis and interpretation of the data: RSR, ATE, GGM, VHB, MB and LMB.
6. Statistical processing: RSR and GGM.
7. Literature search: VHB and RSR.
8. Drafting of the manuscript: RSR, ATE, VHB and LMB.
9. Critical review of the manuscript with relevant intellectual contributions: RSR, ATE, GGM, VHB, MB and LMB.
10. Approval of the final version: RSR, ATE, GGM, VHB, MB and LMB.
FundingThis study was funded by a research grant from the Sociedad Española de Radiología [Spanish Society of Radiology] (Sociedad Española de Radiología Médica (SERAM) [Spanish Society of Medical Radiology]-Industry Grants). The above organisation did not participate in either the design or the conduct of this study.
Conflict of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Sanz-Requena R, Ten Esteve A, Hervás Briz V, García-Martí G, Beltrán M, Martí-Bonmatí L. Análisis estructural cuantitativo del hueso alveolar trabecular de la mandíbula en tomografía computarizada multidetector: diferencias por tipo y estado dentario. Radiología. 2019;61:225–233.