Most people with persistent tics report an unpleasant sensation (premonitory urge) before the tic. In recent years, interest in these sensory phenomena has increased due to their important role in behavioural therapy. However, instruments for assessing these sensations remain scarce. Among the available instruments, the Premonitory Urge for Tics Scale (PUTS) is the most widely used.
MethodsWe examined the psychometric properties and factor structure of the Spanish-language version of the PUTS in a sample of 72 children and adolescents with Tourette syndrome or persistent tic disorders. We analysed data from the total sample and by age group (children up to 10 years old and children/adolescents over 10).
ResultsThe PUTS presented good internal consistency and moderate correlations between items on the scale (except for item 1). Divergent validity was good, test-retest reliability was adequate, and a bifactorial structure was identified (one dimension related to mental phenomena reported in obsessive-compulsive disorder, and another related to the quality and frequency of premonitory urges). These results were replicated in both age groups, with lower divergent validity and test-retest reliability in the younger group.
ConclusionsThe Spanish-language version of the PUTS is a valid, reliable tool for assessing premonitory urges in both children and adolescents, especially after the age of 10.
La mayoría de personas con tics persistentes refiere notar una sensación desagradable (impulso premonitorio) antes de sufrir un tic. En los últimos años, el interés hacia estos fenómenos sensoriales ha aumentado debido al importante papel que tienen en la terapia de conducta. Sin embargo, los instrumentos para evaluarlos aún son escasos. Entre ellos, la Escala para el Impulso Premonitorio al Tic (Premonitory Urge for Tics Scale, PUTS) es el más utilizado.
MétodosExaminamos las propiedades psicométricas y la estructura factorial de la versión española de la PUTS en una muestra de 72 niños y adolescentes con síndrome de Tourette o trastorno de tics persistentes. Analizamos los datos para el total de la muestra y por grupos de edad (niños hasta los 10 años y mayores de 10 años).
ResultadosLa PUTS obtuvo una buena consistencia interna y correlaciones moderadas entre ítems de la escala (excepto en el ítem 1). Se encontró una buena validez divergente, una adecuada fiabilidad test-retest y una estructura bifactorial (con una dimensión de fenómenos mentales relacionados con el trastorno obsesivo-compulsivo y otra sobre las cualidades y frecuencia de los impulsos premonitorios). Estos resultados se replicaron para ambos grupos de edad, excepto la validez divergente y la fiabilidad test-retest que fueron inferiores en el grupo de menor edad.
ConclusionesLa versión española de la PUTS es una herramienta válida y fiable para evaluar los impulsos premonitorios en población infanto-juvenil, especialmente después de los 10 años.
Tourette syndrome (TS) and chronic tic disorders (CTD) are neuropsychiatric disorders characterised by the appearance of motor and/or vocal tics persisting for over a year.1 These disorders appear in childhood,2 frequently in association with attention-deficit/hyperactivity disorder (ADHD) and obsessive-compulsive disorder (OCD).3
Most patients with TS and CTDs report that their tics are preceded by uncomfortable sensations, known as premonitory urges. These sensations are described as itching, pressure, or tension, and they are usually relieved or disappear after performing the tic.4 Although premonitory urges have traditionally received little attention from the scientific community, they have recently begun to be studied more systematically due to the important role they play in behavioural therapy.5
However, few instruments are available to evaluate these sensory phenomena. One of the most frequently used tools is the Premonitory Urge for Tics Scale (PUTS), a self-administered 10-item questionnaire that evaluates the severity of premonitory urges. The PUTS was created by Woods et al.6 and validated in a sample of 42 children and adolescents from the United States in 2005. In recent years, the PUTS has been validated in several languages and populations, replicating the good psychometric properties of the original version in children7–10 and adults11–13 (Table 1).
Psychometric properties of the Premonitory Urge for Tics Scale in previous studies into the paediatric population.
| Authors (year) | Sample, subgroups | Mean PUTS score (SD) | α | Test-retest reliability | Factor analysis |
|---|---|---|---|---|---|
| Woods et al.6 (2005) | 42 children and adolescents with TS or CTDs (mean age, 10.8 years; SD = 2.3) | 18.5 (6.1) | 0.81 | 1 week (r1 = 0.79)2 weeks (r2 = 0.86) | NA |
| Group 1 (n = 19; ≤ 10 years) | 18.3 (4.6) | 0.57 | r1 = 0.75 / r2 = 0.72 | ||
| Group 2 (n = 23; > 10 years) | 18.6 (7.3) | 0.89 | r1 = 0.81 / r2 = 0.91 | ||
| Steinberg et al.9 (2010) | 40 children and adolescents with TS or CTDs (mean age, 11.05 years; SD = 2.05) | 20.15 (5.89) | 0.79 | NA | NA |
| Group 1 (n = 18; ≤ 10 years) | 18.61 (5.20) | 0.69 | |||
| Group 2 (n = 22; > 10 years) | 21.41 (6.24) | 0.83 | |||
| Gulisano et al.10 (2015) | 95 children and adolescents with TS evaluated at 2 time points: | NA | NA | ||
| Baseline (mean age, 7.3; SD = 1.5) | 13.4 (5.5) | 0.85 | |||
| 7-year follow-up (mean age, 13.1 years; SD = 3.7) | 24.1 (6.1) | 0.70 | |||
| Raines et al.7 (2018) | 84 children, adolescents, and young adults with CTDs (mean age, 11.39 years; SD = 3.68) | 19.60 (6.31) | 0.82 | NA | Exploratory, 2 factors |
| Group 1 (n = 34; ≤ 10 years) | 18.85 (5.12) | 0.66 | NA | ||
| Group 2 (n = 50; > 10 years) | 20.12 (7.01) | 0.87 | NA | ||
| Openneer et al.8 (2019) | 656 children and adolescents with CTDs (mean age, NA) | 20.16 (6.17) | 0.80 | NA | Exploratory, 1 factor |
| Group 1 (n = 103; ≤ 7 years) | 17.03 (6.15) | 0.84 | 1 factor | ||
| Group 2 (n = 253; 8-10 years) | 19.40 (6.14) | 0.83 | 1 factor | ||
| Group 3 (n = 300; > 10 years) | 21.87 (5.65) | 0.76 | 2 factors |
CTD: chronic tic disorder; NA: not available; PUTS: Premonitory Urge for Tics Scale; SD: standard deviation; TS: Tourette syndrome.
The objective of this study is to evaluate the psychometric properties of the Spanish-language version of the PUTS in a sample of children and adolescents with TS/CTDs, and to provide further evidence on certain aspects that have received little attention, such as test-retest reliability and the factor structure. We studied the 9-item version of the PUTS, excluding item 10, as recommended by the authors of the scale6 and also by subsequent studies in which the item was found not to correlate well with the rest of the scale.
MethodsParticipantsThe study included 72 children and adolescents with TS or CTD. They were recruited between 2013 and 2015 from the department of child and adolescent psychiatry and clinical psychology of Hospital Clínic de Barcelona and from the paediatric neurology department of Hospital Universitario Virgen del Rocío in Seville, in the context of the European Multicentre Tics in Children Studies. This is a longitudinal study examining the role of genes, immunity, and psychosocial stress in the development and progression of tics.14 To this end, 715 children and adolescents with TS or CTDs aged 3-16 years were followed up for 16 months, with visits scheduled every 4 months to evaluate tic severity and presence of comorbid symptoms and to gather biological samples. We excluded patients with severe concomitant diseases, those receiving antibiotics in the previous month, and those with difficulty understanding the protocol. Although the use of psychotropic drugs was not an exclusion criterion, we did record this information. The study was approved by our hospital’s ethics committee. All participants and their parents gave written informed consent.
ProcedureDuring the initial assessment, a clinical researcher from each centre confirmed the diagnosis of a tic disorder using a standardised form with the criteria established by the Diagnostic and Statistical Manual of Mental Disorders, 4th edition. Similar forms were used to confirm diagnosis of OCD and ADHD. We gathered demographic data and information about psychotropic drugs, and evaluated the severity of tics and other psychiatric symptoms using standardised instruments.
Clinical assessmentThe PUTS6 was translated into Spanish by our research group and back-translated into English by a bilingual clinician. The scale contains 10 items evaluating premonitory urges on a 4-point ordinal scale (1: not at all; 2: a little; 3: pretty much; 4: very much). The total score is obtained by adding the scores of the first 9 items, and ranges from 9 to 36 points. We used baseline data to analyse the scale’s psychometric properties and 4-month follow-up data (n = 55) to evaluate test-retest reliability. Seventeen patients were lost to follow-up at 4 months: 12 did not attend the 4-month follow-up assessment and the remaining 5 did not fully complete the questionnaire (< 80% of items).
The Yale Global Tic Severity Scale (YGTSS)15 is a semistructured interview that evaluates the severity of tics. Motor and vocal tics present over the week prior to the assessment were scored separately on a scale scoring 5 dimensions (number, frequency, intensity, complexity, and interference) from 0 to 5 points. The severity of tics was calculated by adding the severity scores for motor (0-25 points) and vocal tics (0-25 points). The YGTSS has shown good psychometric properties and has been confirmed to have a two-factor structure in the Spanish population.16
The Children’s Yale-Brown Obsessive-Compulsive Scale (CY-BOCS)17 is a semistructured interview for children and adolescents that assesses the severity of obsessive-compulsive symptoms occurring in the week prior to assessment. Obsessive and compulsive behaviours are scored separately on a scale from 0 to 4 points evaluating 5 dimensions: time occupied, interference, distress, resistance, and control. The total severity score results from adding severity scores for obsessive (0-20) and compulsive behaviours (0-20). The Spanish-language version of this questionnaire has been found to be valid and reliable.18
The Strengths and Difficulties Questionnaire (SDQ)19 is a 25-item scale evaluating emotional and behavioural problems in children and adolescents. It assesses 5 domains: emotional symptoms, conduct problems, hyperactivity/inattention, peer relationships problems, and prosocial behaviour. The Spanish-language version of the SDQ has shown adequate validity and reliability, as well as a factor structure that is consistent with the 5 subscales.20
Statistical analysisWe used the t test for independent samples and the chi-squared test to analyse the potential demographic and clinical differences between participants from Barcelona and Seville. The Cronbach alpha test was used to determine the internal consistency of the PUTS. The Pearson bivariate correlation test was used to calculate the association between PUTS, YGTSS, and CY-BOCS scores; divergent validity (correlation between the PUTS and the SDQ), and test-retest reliability. An exploratory factor analysis was performed using Varimax rotation to determine the factor structure of the PUTS, following the procedure described in previous studies evaluating the factor structure of the scale.7,8,13 As in previous studies,6–9 all analyses were repeated with participants classified by age (27 children aged up to 10 years [mean: 8.77 years; SD: 1.54] vs 45 children and adolescents aged over 10 years [mean: 13.62; SD: 1.60]). Data were analysed using SPSS statistical software version 23.21
ResultsSample characteristicsThe sample included 72 children and adolescents (83.3% were boys; 97% were white Europeans) with a mean age (SD) of 11.80 (2.84) years (range, 5-16). Most participants (n = 47; 65.3%) were recruited from Hospital Clínic de Barcelona. We found no statistically significant differences in age, sex, or baseline PUTS scores between the 2 centres.
Regarding clinical data, 67 participants (93.1%) had a diagnosis of TS, 4 (5.5%) had chronic motor tic disorder, and one (1.4%) had chronic vocal tic disorder. A total of 62.5% of participants were receiving pharmacological treatment (mainly atypical antipsychotics). Lastly, 29 participants (40.3%) also had a diagnosis of ADHD and 17 (23.6%) also had OCD. Table 2 presents mean PUTS scores for the whole sample and by age group. Mean total YGTSS and CY-BOCS scores were 22.10 (8.64) and 7.61 (8.69), respectively. No statistically significant differences were observed in mean PUTS, YGTSS, or CY-BOCS scores between age groups.
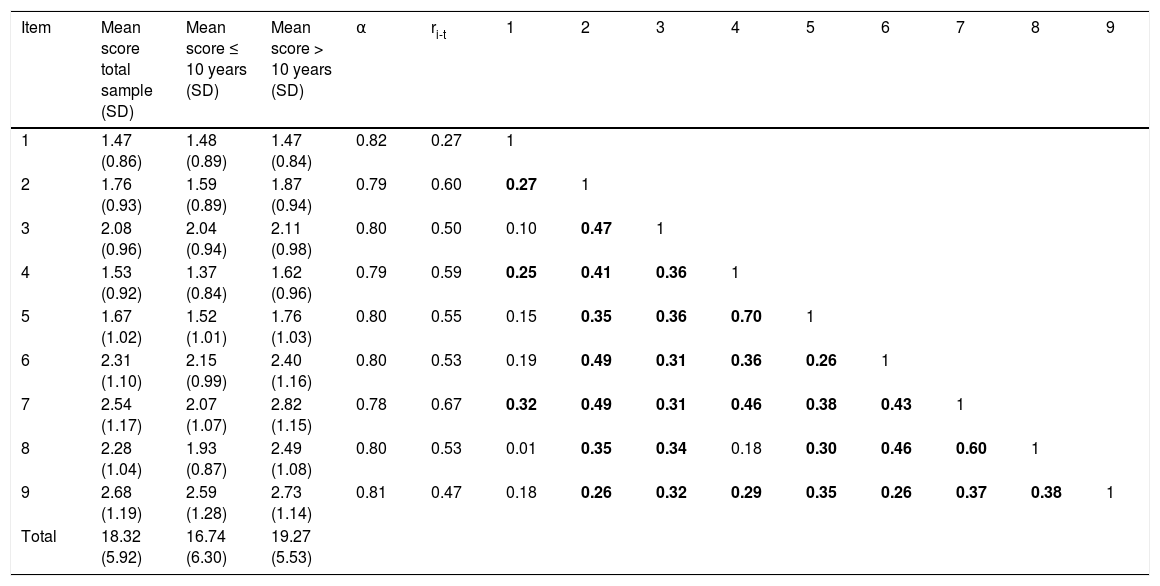
Mean scores, Cronbach alpha, item-total correlations, and correlations between items for the Premonitory Urge for Tics Scale.
| Item | Mean score total sample (SD) | Mean score ≤ 10 years (SD) | Mean score > 10 years (SD) | α | ri-t | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 1.47 (0.86) | 1.48 (0.89) | 1.47 (0.84) | 0.82 | 0.27 | 1 | ||||||||
| 2 | 1.76 (0.93) | 1.59 (0.89) | 1.87 (0.94) | 0.79 | 0.60 | 0.27 | 1 | |||||||
| 3 | 2.08 (0.96) | 2.04 (0.94) | 2.11 (0.98) | 0.80 | 0.50 | 0.10 | 0.47 | 1 | ||||||
| 4 | 1.53 (0.92) | 1.37 (0.84) | 1.62 (0.96) | 0.79 | 0.59 | 0.25 | 0.41 | 0.36 | 1 | |||||
| 5 | 1.67 (1.02) | 1.52 (1.01) | 1.76 (1.03) | 0.80 | 0.55 | 0.15 | 0.35 | 0.36 | 0.70 | 1 | ||||
| 6 | 2.31 (1.10) | 2.15 (0.99) | 2.40 (1.16) | 0.80 | 0.53 | 0.19 | 0.49 | 0.31 | 0.36 | 0.26 | 1 | |||
| 7 | 2.54 (1.17) | 2.07 (1.07) | 2.82 (1.15) | 0.78 | 0.67 | 0.32 | 0.49 | 0.31 | 0.46 | 0.38 | 0.43 | 1 | ||
| 8 | 2.28 (1.04) | 1.93 (0.87) | 2.49 (1.08) | 0.80 | 0.53 | 0.01 | 0.35 | 0.34 | 0.18 | 0.30 | 0.46 | 0.60 | 1 | |
| 9 | 2.68 (1.19) | 2.59 (1.28) | 2.73 (1.14) | 0.81 | 0.47 | 0.18 | 0.26 | 0.32 | 0.29 | 0.35 | 0.26 | 0.37 | 0.38 | 1 |
| Total | 18.32 (5.92) | 16.74 (6.30) | 19.27 (5.53) |
ri-t: corrected item-total correlation; SD: standard deviation.
Internal consistency (Cronbach alpha) was calculated after removing each item. Statistically significant correlations between items are indicated in bold.
Cronbach’s alpha was 0.82. Table 2 presents Cronbach’s alpha coefficients with each scale item removed; corrected item-total correlations (ie, correlation between each item and the sum of the rest of items); and correlations between items for the PUTS. The results show high internal consistency; internal consistency did not increase with removal of any of the items. Item-total correlations were strong. Correlations between items were moderate in all cases except for item 1, which showed no correlation with 5 of the remaining items.
By age group, the Cronbach’s alpha coefficient was higher in the group of children aged up to 10 years than in the older age group (α = 0.88 vs α = 0.77).
Correlations between PUTS, YGTSS, and CY-BOCS scoresTotal PUTS score was not correlated with severity of motor tics (r = 0.15; P = .212), severity of vocal tics (r = 0.17; P = .167), total YGTSS score (r = 0.19; P = .114), severity of obsessive behaviour (r = 0.14; P = .251), severity of compulsive behaviour (r = 0.21; P = .082), or total CY-BOCS score (r = 0.18; P = .128). Analysis by age group yielded similar results.
Divergent validityNo statistically significant correlations were observed between PUTS scores and scores on most SDQ dimensions (emotional symptoms: r = 0.17; P = .157; conduct problems: r = 0.16; P = .606; peer relationship problems: r = −0.01; P = .940; prosocial behaviour: r = 0.06; P = .612). We did observe a statistically significant positive correlation between PUTS and the dimension hyperactivity/inattention (r = 0.30; P = .011). By age group, the younger group displayed positive correlations between the PUTS and the dimensions hyperactivity/inattention (r = 0.43; P = .029) and emotional symptoms (r = 0.44; P = .026). In the older group, in contrast, no correlation was found between the PUTS and any SDQ dimension.
Test-retest reliabilityA moderate correlation was found between PUTS scores at baseline and at 4 months (r = 0.49; P < .001), with similar results in the older group (r = 0.61; P < .001); the correlation was not statistically significant in the group of younger participants.
Factor analysisAs shown in Table 2, item 1 showed a weak correlation with the remaining items, and was therefore removed from the factor analysis, as reported in previous studies where items 1 or 9 were removed.7,8
According to the factor analysis, 2 factors were found to explain 59.42% of total variance (Table 3). Items 2, 3, 6, 7, 8, and 9 showed higher saturations in the first factor, whereas items 4 and 5 showed higher saturations in the second factor. The Kaiser–Meyer–Olkin (KMO) test confirmed the adequacy of our data for factor analysis (KMO value of 0.75; values above 0.6 indicate sampling adequacy).22 Bartlett’s test of sphericity yielded significant results (χ228 = 195.26; P < .001), which suggests that correlations between items were sufficiently strong for factor analysis to be performed. Analysis by age group yielded similar results in children aged up to 10 years and in older children and adolescents.
Factor saturations after Varimax rotation for the Premonitory Urge for Tics Scale.
| Items | Factor 1 | Factor 2 |
|---|---|---|
| 2. Right before I do a tic, I feel pressure inside my brain or body. | 0.607 | 0.384 |
| 3. Right before I do a tic, I feel “wound up” or tense inside. | 0.458 | 0.440 |
| 4. Right before I do a tic, I feel like something is not “just right.” | 0.189 | 0.890 |
| 5. Right before I do a tic, I feel like something is not complete. | 0.182 | 0.868 |
| 6. Right before I do a tic, I feel like there is energy in my body that needs to get out. | 0.710 | 0.164 |
| 7. I have these feelings almost all the time before I do a tic. | 0.738 | 0.298 |
| 8. These feelings happen for every tic I have. | 0.845 | 0.014 |
| 9. After I do the tic, the itchiness, energy, pressure, tense feelings, or feelings that something is not “just right’’ or complete go away, at least for a little while. | 0.499 | 0.306 |
| % of explained variance | 45.88% | 13.54% |
The factor into which each item is grouped is indicated in bold.
The Spanish-language version of the PUTS has been shown to have good psychometric properties, making it a valid and reliable tool for evaluating premonitory urges in children and adolescents. Our study provides new evidence on the scale’s test-retest reliability and factor structure.
Our results indicate that the Spanish-language version of the PUTS has good internal consistency, as shown by several indicators (Cronbach alpha, corrected item-total correlation, and correlations between items); this is consistent with the results reported for the original, English-language scale6–8 and for adaptations into Hebrew9 and Italian.10 However, while most studies report greater consistency in older children, internal consistency in our sample was slightly higher in the group of children aged up to 10 years; the same was observed in the study by Openneer et al.8 A plausible explanation is the high mean age in our group of younger children (nearly 9 years). This could explain why intergroup differences in internal consistency were not as marked in our study (0.11 points, compared to differences of up to 0.32 points in previous studies).6 Furthermore, although correlations between items were good overall, we agree with Openneer et al.8 that item 1 (“Right before I do a tic, I feel like my insides are itchy”) has a weak correlation with the rest of the scale. As shown in our study and in previous studies,11 describing premonitory urges in terms of pressure or tension may be more useful for clinicians, as these sensations are reported more frequently than itching.
We did not find statistically significant correlations between PUTS score and such other variables as severity of tics and presence of obsessive-compulsive symptoms, either for the whole sample or by age group. Although we believe that this finding underscores the discriminatory power of the tool, it stands in contrast with the results of other studies describing positive associations between premonitory urges and tics or obsessive-compulsive symptoms.6–8 These discrepancies may be explained by the mild severity of tics and obsessive-compulsive symptoms (subclinical mean total score) observed in our sample. Likewise, the lack of correlation between these variables may also be due to a lower incidence of comorbidities in our sample than in previous studies (some report up to 62% of patients with ADHD6 or nearly 30% with OCD8). Furthermore, and similarly to Openneer et al.,8 we found positive correlations between the PUTS and symptoms of hyperactivity/inattention. However, we believe that these data, together with the weak or non-existent correlations with the SDQ, suggest that the Spanish-language version of the PUTS presents good divergent validity, mainly in the older group (> 10 years). Future studies are needed to replicate these findings and to analyse the association between PUTS scores and the severity of tics.
The PUTS showed excellent test-retest reliability, with good temporal stability even at 4 months of follow-up. The fact that the retest was performed at 4 months may explain why our correlations were considerably weaker than those reported in the only previous study (in which retests were performed at one and 2 weeks),6 given that tics often present exacerbations, which become more frequent with time. As in the study by Woods et al.,6 younger children reported their premonitory urges less consistently (correlations were not statistically significant in the group of children under the age of 10 years); this is coherent with the difficulties identifying premonitory urges described in young children.23
Factor analysis confirmed the two-factor structure observed in the only 2 studies conducted to date in children and adolescents,7,8 which clearly reflects the existence of a dimension of mental phenomena related to OCD (“not just right experiences”) and another dimension linked to the qualities and frequency of premonitory urges. The content of these 2 factors coincides with the results reported by Openneer et al.8 in children older than 10 years (although our results are similar for the whole sample and in each age group), as well as with studies describing 2 types of premonitory urges: “specific feelings such as tension or an itch in a particular area, or more vague feelings that something is ‘not just right.’”23
Our results should be interpreted with caution due to several limitations. Firstly, the classification of participants by age resulted in groups of fewer than 30 participants, which may have affected the validity of our results. Secondly, nearly all participants were white Europeans, which may limit the possibility of extrapolating our results to other populations. Thirdly, the severity of tics and other psychiatric symptoms was relatively mild, which may have influenced some of our results. Furthermore, we did not evaluate convergent validity with another instrument designed for the assessment of premonitory urges. The only study published to date that has evaluated convergent validity included a sample of adults and compared the PUTS against a real-time urge assessment monitor, finding a strong correlation between both instruments.13 Lastly, a considerable percentage of participants were lost to follow-up at 4 months; therefore, test-retest reliability analyses were conducted with 55 participants.
In conclusion, our data suggest that the Spanish-language version of the PUTS has good psychometric properties, similar to those described in the literature. Our study provides additional evidence on the temporal stability and two-factor structure of the PUTS. The Spanish-language version of the PUTS is a valid, reliable tool for evaluating premonitory urges in children and adolescents, especially in children older than 10 years. Further research should focus on certain aspects for which the available data present discrepancies and other outstanding questions, such as sensitivity to change.
FundingThis study received no funding of any kind.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors are grateful for the collaboration of the families participating in the European Multicentre Tics in Children Studies, a project funded by the European Commission’s Seventh Framework Programme (grant no. 278367).