Paraneoplastic cerebellar degeneration (PCD)1–3 is a rare syndrome that most frequently occurs in women with gynaecological cancer.4 It is characterised by extensive loss of Purkinje cells which are targeted by antibodies (anti-Yo, anti-Tr)5,6; these antibodies may be detected in serum and/or cerebrospinal fluid (CSF).7 These syndromes manifest with pancerebellar symptoms including vertigo, ataxia, dysarthria, and nystagmus.8,9 Symptoms are usually expressed during the underlying tumour's early stages of development, which means that any occult neoplasia should be located urgently.10–12
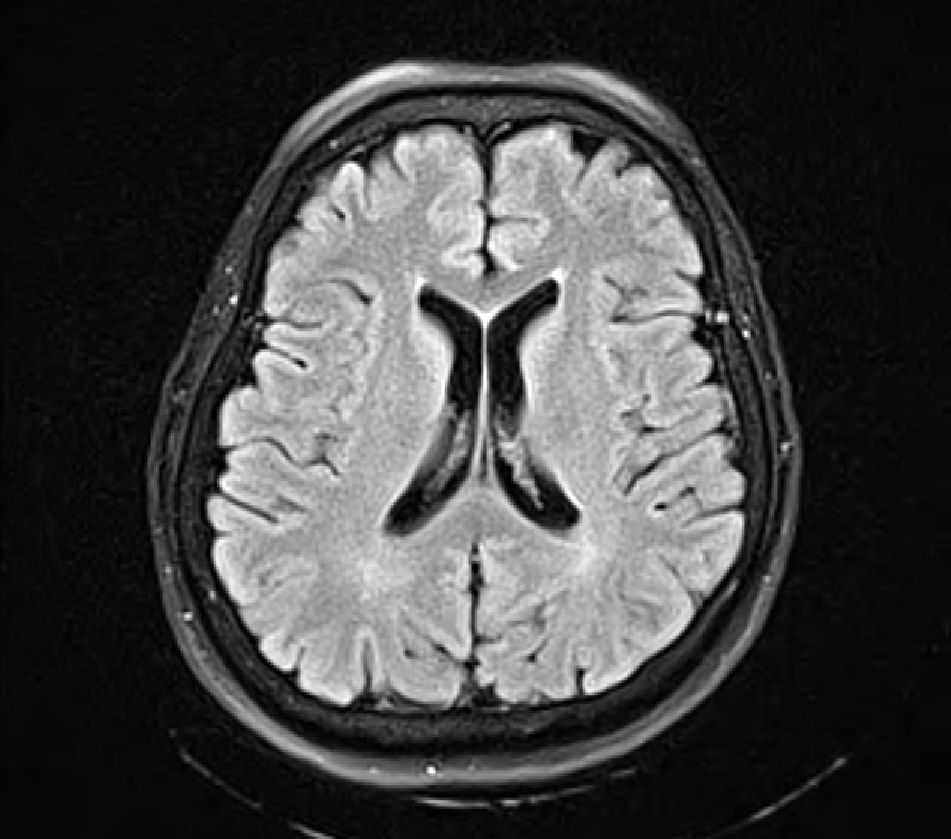
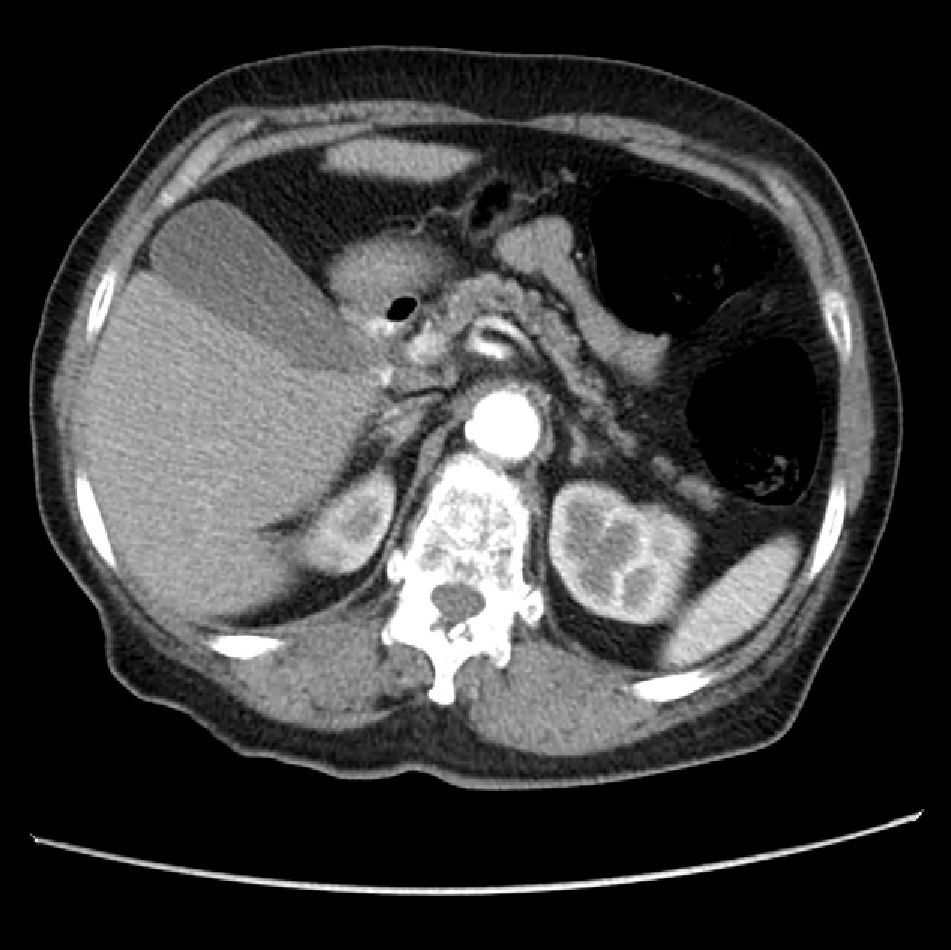
The patient was a 69-year-old woman treated at our hospital for left gaze deviation, generalised hypotonia followed by limb hypertonia, and loss of consciousness lasting approximately 5minutes. Medical history included arterial hypertension and hypothyroidism, both of which were controlled. She had lost 8kg in the preceding 6 months and also experienced difficulty walking, blurred vision, and difficulty speaking in the week prior to hospital admission. Examination showed normal vital signs. The patient was alert and oriented, displaying dysarthria, difficulty following directions, saccadic eye movements, vertical nystagmus, and pronounced left-sided dysmetria on the finger-to-nose test. The patient was unable to perform the heel-to-knee-to-shin test; tendon reflexes, cranial nerves, and sensitivity showed no alterations. Complementary tests showed normal blood count and renal function, no positive ELISA tests for HIV or other entities, normal vitamin B12 levels, and normal CSF results (cytochemistry, direct study, and cultures). Brain MRI with gadolinium contrast (Fig. 1) revealed microangiopathic leukoencephalopathy with no lesions in the posterior fossa and normal MRA. Based on this evidence, doctors suspected PCD. Doctors extended the search for a primary tumour by ordering a thoracic CT and mammary ultrasound; both yielded normal results. Abdominal and pelvic CT (Fig. 2) revealed a retroperitoneal mass proximate to the third part of the duodenum with no masses in ovaries or adjacent structures. The mass was resected and determined to be a retroperitoneal lymph node with poorly differentiated metastatic adenocarcinoma. The immunohistochemical study was inconclusive. The Western blot test was used to check for anti-Hu and anti-Yo antibodies, and the latter were detected. The patient was started on steroid treatment at 1mg/kg/day, but progress was poor. Cerebellar symptoms evolved rapidly, and the patient was unable to walk or swallow less than 7 days after being admitted. Due to the patient's rapid clinical decline and poor prognosis, doctors decided not to undertake further studies or provide any treatments (plasmapheresis, immunoglobulin) that might worsen her clinical state without providing significant benefits, as has been described in the literature.13,14 This case generates concern about the benefits of searching for the primary tumour and using full immunosuppression in patients with PCD and anti-Yo antibodies. This situation gives rise to a survival time of between 13 and 22 months, and oncological treatment has no effect on the functional outcome; patient decline tends to be rapid and pronounced.6,11,15
We would like to thank Dr Yuri Takeuchi Tan, Dr Andrés Felipe Echeverri Garcia, and Dr Yaneth Aljure.
Please cite this article as: Cadavid D, Diaz JC, Masaru Shinchi A, Jesualdo Ariza Y. Deterioro neurológico rápido y severo asociado a degeneración cerebelosa paraneoplásica con anticuerpos anti-Yo positivos. Neurología. 2014;29:128–129.