Epileptic psychoses are categorised as peri-ictal and interictal according to their relationship with the occurrence of seizures. There is a close temporal relationship between peri-ictal psychosis and seizures, and psychosis may present before (preictal), during (ictal) or after seizures (postictal). Epileptic psychoses usually have acute initial and final phases, with a short symptom duration and complete remission with a risk of recurrence. There is no temporal relationship between interictal or chronic psychosis and epileptic seizures. Another type of epileptic psychosis is related to the response to epilepsy treatment: epileptic psychosis caused by the phenomenon of forced normalisation (alternative psychosis), which includes epileptic psychosis secondary to epilepsy surgery. Although combination treatment with antiepileptic and neuroleptic drugs is now widely used to manage this condition, there are no standard treatment guidelines for epileptic psychosis.
Clinical casesWe present 5 cases of peri-ictal epileptic psychosis in which we observed an excellent response to treatment with levetiracetam. Good control was achieved over both seizures and psychotic episodes. Levetiracetam was used in association with neuroleptic drugs with no adverse effects, and our patients did not require high doses of the latter.
ConclusionsCategorising psychotic states associated with epilepsy according to their temporal relationship with seizures is clinically and prognostically useful because it provides important information regarding disease treatment and progression. The treatment of peri-ictal or acute mental disorders is based on epileptic seizure control, while the treatment of interictal or chronic disorders has more in common with managing disorders which are purely psychiatric in origin. In addition to improving the patient's quality of life and reducing disability, achieving strict control over seizures may also prevent the development of interictal psychosis. For this reason, we believe that establishing a treatment protocol for such cases is necessary.
Las psicosis epilépticas se dividen respecto de su relación con las crisis en periictales e interictales. Las psicosis periictales tienen una estrecha relación temporal con las crisis epilépticas y ocurren antes (preictales), durante (ictales) o después de las mismas (postictales). Generalmente, tienen un inicio y final agudo, corta duración y una remisión completa, con riesgo de recurrencia. Las psicosis interictales o crónicas no guardan relación temporal con las crisis epilépticas. Existe otro tipo de psicosis epilépticas que se relaciona con la respuesta al tratamiento de la epilepsia: psicosis epiléptica por fenómeno de normalización forzada (psicosis alternativa) y dentro de esta se encuentra la psicosis epiléptica secundaria a cirugía de la epilepsia. Aunque se ha generalizado la combinación de antiepilépticos y neurolépticos para su manejo, no existen unas pautas estandarizadas de tratamiento en las psicosis epilépticas.
Casos clínicosPresentamos 5 casos de psicosis epilépticas periictales y remarcamos la excelente respuesta al tratamiento con levetiracetam. Consiguiendo un buen control tanto de las crisis como de los episodios psicóticos. Este fármaco resultó inocuo al asociarlo con neurolépticos en nuestros pacientes y no se precisaron dosis elevadas de estos últimos.
ConclusionesLa diferenciación de los estados psicóticos asociados con la epilepsia según la relación temporal con las crisis epilépticas tiene utilidad clínica y pronóstica, dado que aporta aspectos importantes respecto al tratamiento y a la evolución de la enfermedad. El tratamiento de los trastornos mentales periictales o agudos se basa en el control de las crisis epilépticas, mientras que el tratamiento de los interictales o crónicos guarda más similitud con el de los trastornos de origen puramente psiquiátrico. El control estricto de las crisis puede, además de mejorar la calidad de vida del paciente y su discapacidad, prevenir el desarrollo de una psicosis interictal, por lo que consideramos que sería necesario establecer un protocolo de tratamiento para estos casos.
Doctors have known since the mid-19th century that there is a relationship between epilepsy and psychosis1; however, the pathophysiological causes of this association remain unknown even today. The temporal lobe houses structures of the limbic system that participate in the regulation of emotional behaviour. Changes in personality are known to be related to interaction between the hippocampus and the amygdala.2 Moreover, patients with temporal lobe epilepsy present a higher frequency of schizophrenia-like psychoses.3,4 According to the literature, between 19% and 80% of all epileptic patients experience a psychotic episode at some point during the course of the disease. Some studies have shown that the type of epileptic syndrome, treatment response, and the patient's psychosocial conditions affect an epileptic patient's probability of developing psychosis.5
Epileptic psychoses often manifest as visions, auditory or visual hallucinations, and affective changes, such as agitation, fear, or paranoia. They may be described as peri-ictal or interictal psychoses depending on the moment in which they appear. Peri-ictal psychoses have a close temporal relationship with epileptic seizures, and may occur before (pre-ictal), during (ictal), or after (postictal) seizures. They are generally characterised by abrupt onset and resolution, short duration, and full remission with risk of recurrence. The relationship between interictal or chronic psychoses and epileptic seizures is not based on proximity in time. Based on the link between psychosis and type of seizure treatment, we can distinguish between epileptic psychosis due to forced normalisation and alternative psychosis, which includes epileptic psychosis secondary to epilepsy surgery.6
A combination of antiepileptic and neuroleptic drugs is frequently used in treating epileptic psychoses, despite the interactions caused by the hepatic metabolism of most of these drugs. Nevertheless, there is no consensus on the optimal antiepileptic drug for this pathology and no standard guidelines for treating this type of psychosis.6
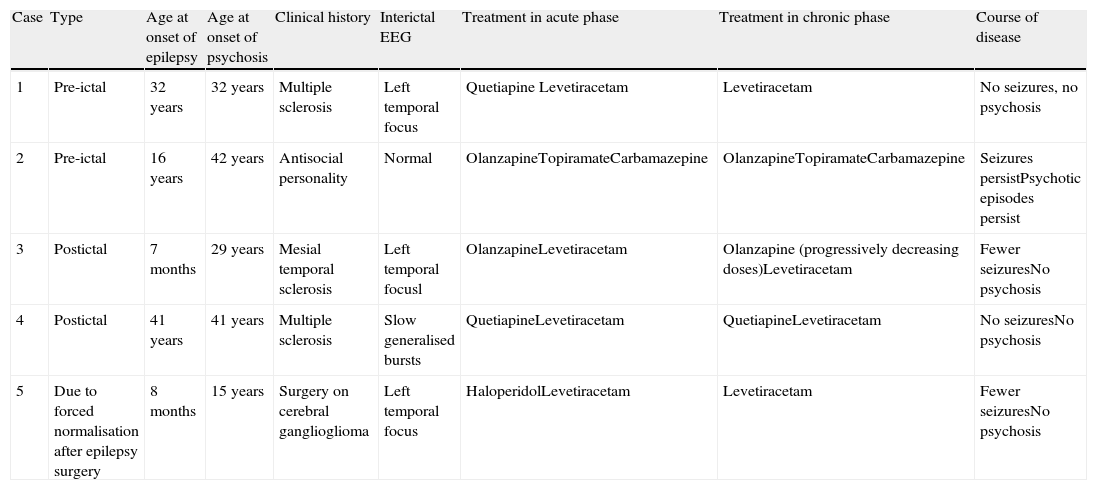
Patients and methodsWe present a descriptive study of 5 cases of peri-ictal epileptic psychosis that respond to treatment with antiepileptic drugs associated with an antipsychotic during the acute phase (Table 1). We highlight the safety of and good response to treatment with levetiracetam and low doses of neuroleptic drugs in these cases.
Summary table of the cases with peri-ictal epileptic psychosis.
| Case | Type | Age at onset of epilepsy | Age at onset of psychosis | Clinical history | Interictal EEG | Treatment in acute phase | Treatment in chronic phase | Course of disease |
| 1 | Pre-ictal | 32 years | 32 years | Multiple sclerosis | Left temporal focus | Quetiapine Levetiracetam | Levetiracetam | No seizures, no psychosis |
| 2 | Pre-ictal | 16 years | 42 years | Antisocial personality | Normal | OlanzapineTopiramateCarbamazepine | OlanzapineTopiramateCarbamazepine | Seizures persistPsychotic episodes persist |
| 3 | Postictal | 7 months | 29 years | Mesial temporal sclerosis | Left temporal focusl | OlanzapineLevetiracetam | Olanzapine (progressively decreasing doses)Levetiracetam | Fewer seizuresNo psychosis |
| 4 | Postictal | 41 years | 41 years | Multiple sclerosis | Slow generalised bursts | QuetiapineLevetiracetam | QuetiapineLevetiracetam | No seizuresNo psychosis |
| 5 | Due to forced normalisation after epilepsy surgery | 8 months | 15 years | Surgery on cerebral ganglioglioma | Left temporal focus | HaloperidolLevetiracetam | Levetiracetam | Fewer seizuresNo psychosis |
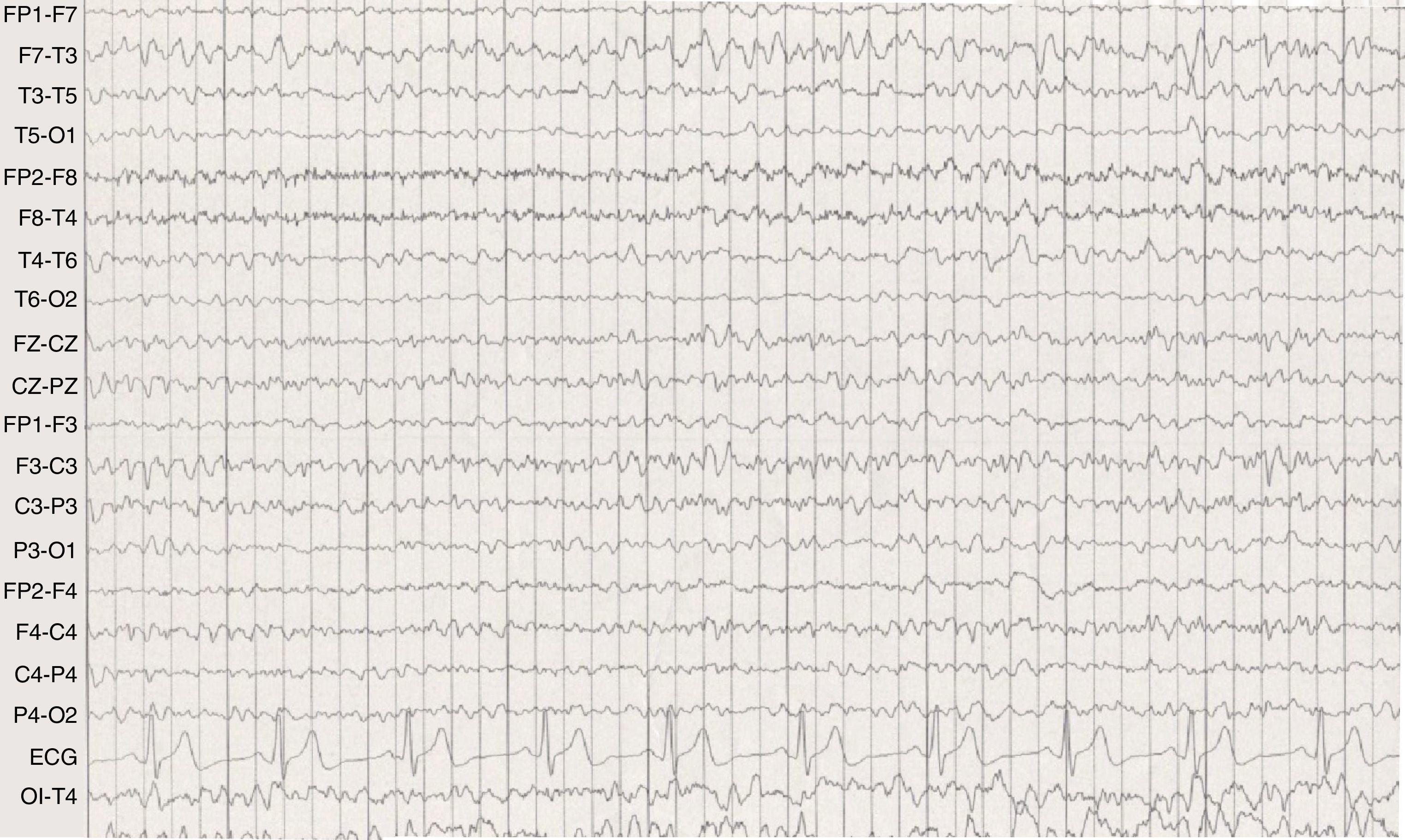
Case 1 was a female patient aged 32 years who was diagnosed in 1997 with relapsing-remitting multiple sclerosis that progressed rapidly. She therefore was treated consecutively with interferon β-1a, azathioprine, and mitoxantrone. The condition stabilised over the 2 following years (EDSS 3.5) with glatiramer acetate, amantine, and oxybutynin. The patient visited the emergency department and stated that she was hearing voices. She was diagnosed with obsessive intrusive thoughts, with judgement and sense of reality remaining intact; the patient was discharged under treatment with oxcarbazepine. After 48hours, she returned to the emergency department with symptoms of disorientation, distress, and paranoia. Clinical progression was changeable and she was even conscious of her agitation at times. She was able to speak coherently, exhibiting spontaneous, fluent, and occasionally verbose language. She also expressed self-obsessed damaging delusional thinking (“I’m going to go mute”, “I’m going to die”) and auditory hallucinations. She was admitted into the psychiatry department and treated with quetiapine (100mg/day). Forty-eight hours later, she suffered a tonic-clonic seizure preceded by bending of the torso and head to the right for a few minutes, with no tongue biting or sphincter dilation, followed by post-ictal stupor. A few minutes later, a similar new seizure occurred. The brain MRI showed no new lesions or contrast uptake in pre-existing lesions. Waking EEG showed a deep irritative temporal left focus with normal recorded baseline reading (Fig. 1). In light of the above, she was diagnosed with pre-ictal epileptic psychosis and treated with levetiracetam (2000mg/day) and quetiapine (100mg/day). The patient has not experienced any new epileptic seizures or psychotic episodes during the last 4 years. Therefore, quetiapine was progressively discontinued and she remains under treatment with levetiracetam (1000mg/day).
Case 2 was a male patient aged 42 years with antisocial personality traits, impulsive behaviour, and low self-esteem. The patient had suffered from idiopathic focal epilepsy of the temporal lobe since childhood. He was being treated with carbamazepine (800mg/day) and topiramate (300mg) which failed to achieve correct epilepsy control (2 seizures per month). The patient experienced symptoms of paranoia and distressing auditory hallucinations (in the second and third person) with spiritual and religious content. He was therefore admitted to the psychiatry unit. The patient had delusional and megalomaniac thoughts that were related to his auditory hallucinations and notions of thought extraction. Twenty-four hours after he was admitted, he suffered partial epileptic seizure with secondary generalisation. CT and waking EEG were performed during the episode, but revealed no abnormalities. The condition was brought under control with neuroleptic drugs (60mg of olanzapine every 24hours) during the acute phase. Upon discharge, he was asymptomatic. Nevertheless, the patient still experienced frequent epileptic seizures (2–3 per month), occasionally preceded by psychotic episodes. During the course of the disease, he also suffered from psychotic episodes which were not seizure-related.
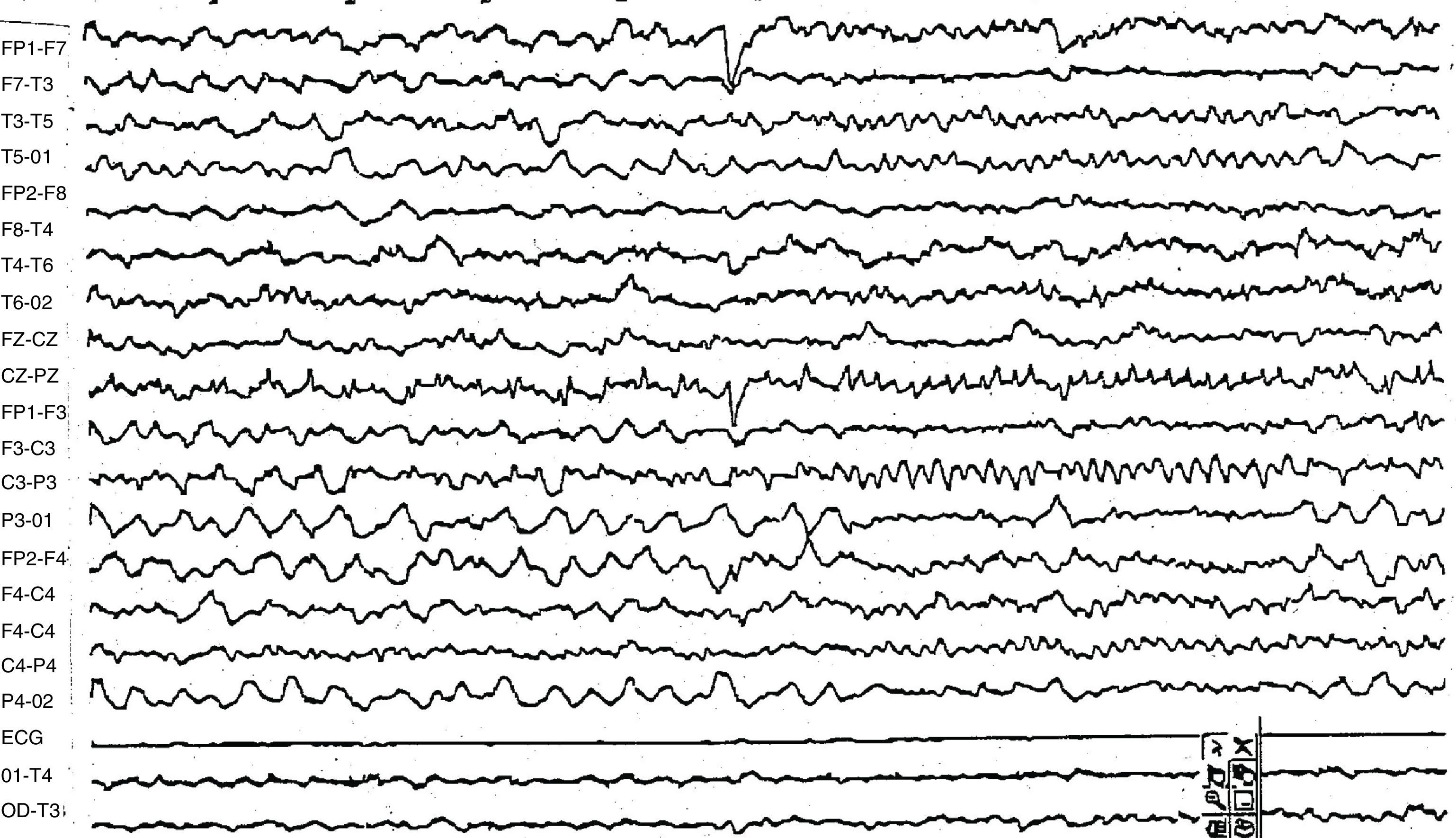
Postictal psychosisCase 3 was a male who had suffered from temporal epilepsy secondary to left mesial temporal sclerosis since childhood. Beginning at the age of 7 months, the patient experienced frequent complex focal epileptic seizures (15 seizures per month), which were refractory to treatment with multiple combinations of antiepileptic drugs including valproic acid, carbamazepine, oxcarbazepine, topiramate, zonisamide, lamotrigine, and benzodiazepines. At the age of 29, 36hours after a focal seizure with secondary generalisation, the patient presented hallucinations with spiritual delusions lasting 72hours and attempted to attack a member of his family while in a confusional state. Results from the urine test for toxic substances were negative. Waking EEG showed an irregular activity of 2 to 4Hz in the left temporal region and acute waves in the left medial temporal region which were moderately persistent during the intercritical period (Fig. 2). Despite treatment with neuroleptic drugs (olanzapine 20mg/day) and antiepileptic polytherapy (rivotril 3mg/day, lamotrigine 600mg/day, zonisamide 400mg/day), he continued having epileptic seizures and occasional postictal psychotic episodes with similar characteristics lasting between 1 and 5 days. When the patient was 32, a preoperative study ruled out bitemporal irritative activity. Doctors decided to perform left temporal lobectomy to treat the drug-resistant epilepsy. After surgery, seizures persisted (6 per month) and frequency of the post-critical psychotic episodes increased despite maintenance of the patient's antiepileptic treatment. After levetiracetam (3000mg/day) was associated with olanzapine (5mg/day), the patient attained acceptable seizure control, with 1 seizure per month and no new episodes of postictal psychosis after the seizure. Neuroleptic drugs could therefore be gradually discontinued.
Case 4 was a 41-year-old woman diagnosed in 1991 with relapsing-remitting multiple sclerosis. She had experienced multiple sensory, motor, and cerebellar exacerbations despite successive courses of treatment with interferon, azathioprine, and mitoxantrone (EDSS 4.5). In 2002 she suffered a first-ever generalised tonic-clonic seizure. A day later, she suffered a psychotic episode with delusional thoughts and hallucinations of voices criticising her behaviour, which caused distress. The patient reported having experienced olfactory hallucinations and frequent déjà vu phenomena. Brain MRI showed no acute lesions. The intercritical waking EEG revealed a slightly slow and unstable record with some generalised slower bursts (Fig. 3). Doctors began treatment with quetiapine (100mg/day) and lamotrigine (400mg/day). Despite the treatment, epileptic seizures persisted on a bimonthly basis and were sometimes followed by psychotic episodes. Doctors decided to add a second antiepileptic drug, and since the patient did not respond to oxcarbazepine, they opted for levetiracetam (1500mg/day). The patient continued taking levetiracetam in monotherapy since her response to that treatment was optimal. Her quetiapine dose has been reduced to 50mg/day.
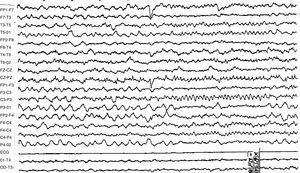
Psychosis secondary to epilepsy surgery due to forced normalisationCase 5 was a woman with a mild intellectual disability who had suffered from complex focal epilepsy since the age of 8 months. The patient showed a poor response to several combinations of antiepileptic drugs with a mean of 8 seizures per month while awake and daily during sleep. During video-EEG monitoring, she presented 30 simple focal seizures and 7 complex focal seizures. The waking EEG performed during the intercritical period showed high-voltage spikes and polyspikes in the left posterior temporal region which were very frequent during the REM sleep phase (Fig. 4). Brain MRI revealed a left temporal mass compatible with ganglioglioma, which was confirmed in the anatomical pathology study. Anterior resection of the left temporal lobe was performed when the patient was 15. Forty-five days later, she had not experienced any additional epileptic seizures and the waking EEG showed no sign of irritative activity. However, she suffered an acute episode of delusional thoughts with visual hallucinations, inability to recognise people, and extreme agitation, which required neuroleptic drugs (haloperidol) to treat the symptoms. Four months later, less intense epileptic seizures reappeared and the patient resumed treatment with levetiracetam (2000mg/day). Seizure intensity and number decreased (3 to 4 seizures per month) with no new psychotic episodes.
DiscussionPre-ictal psychotic episodes begin during the prodromal phase of epileptic seizures (hours or days). The chronological sequence in these psychoses are a matter of debate. According to some theories, episodes are really seizures induced by a psychotic substrate rather than disorders predicting a new epileptic seizure. Other authors believe them to be interictal phenomena.7 The main distinguishing feature of our cases is that psychotic episodes were acute and self-limiting. In the long term, however, they entail a higher risk of developing interictal psychosis. The second case shows that if there is inadequate control over seizures, and therefore over associated psychosis, patients may experience episode recurrence and interictal psychosis. However, use of levetiracetam in the first case provided seizure control and prevented new psychotic episodes.
Ictal psychoses are uncommon. These phenomena are typically localised in the temporal lobe and elicit activation of the limbic system and neocortical temporal areas. Prolonged ictal psychotic states are even more infrequent. They usually occur in non-convulsive status epilepticus with simple or complex focal seizures and petit mal seizures. Transient ictal psychoses may be secondary to continuous epileptic discharges that cause no other epileptic symptoms.
Postictal psychosis is the most well-known type of epileptic psychosis and occurs in 2% to 7% of patients with epilepsy. It is defined as a psychotic episode lasting more than 15hours and less than 3 months which appears within a week of an epileptic seizure. The patient presents a confusional state which may appear psychotic, possibly accompanied by hallucinations and delusional thoughts. Affective disorders (depression, mania, aggressiveness) are more common than hallucinations. Negative symptoms are not remarkable. A lucid period lasting 2.5 to 48hours typically presents between the epileptic seizure and the onset of psychotic symptoms.6 Risk factors are as follows: age above 30 years, bilateral seizures or intercritical focus, cluster seizures, secondary generalisation, and family history of affective disorders. Postictal psychosis usually appears a minimum of 10 years after onset of epilepsy (although it has been described after only 5 years) and it is equally frequent in right and left temporal seizures. As the frequency of postictal psychotic episodes increases, so does the risk of developing chronic interictal psychosis.8 Postictal psychosis is related to the presence of bilateral epileptic activity, whether interictal9 or ictal.10 The presence of postictal psychosis is considered to be a poor surgical prognostic factor in mesial temporal epilepsy,11 given that postictal psychosis is associated with bitemporal dysfunction. On the other hand, some authors have achieved good seizure control with no recurrence of postictal psychosis.12 In the third case, a preoperative study showed no evidence of bilateral ictal and interictal activity, but the patient did not respond well to surgical treatment. As in the fourth case, epilepsy and postictal psychosis were controlled using the combination of levetiracetam and low doses of a new neuroleptic drug. We were able to reduce the dose in once case and discontinue the antipsychotic drug in the other.
Several studies have highlighted the relationship between seizures, psychosis, and the phenomenon of forced normalisation.13 This phenomenon is quite uncommon in patients with partial drug-resistant epilepsy whose seizures have been controlled or reduced through treatment. Forced normalisation usually occurs after administration of an effective antiepileptic drug or performance of epilepsy surgery that normalises a previously aberrant EEG (forced normalisation or alternative psychosis). The first 6 months after surgery constitute a high-risk period. The prevalence of developing psychosis as a complication of epilepsy surgery, after resection of the temporal focus, ranges between 3% and 28%.14 The underlying pathophysiological mechanisms remain unclear. It is believed that the high number of temporal lobe discharges could have an inhibitory effect on the limbic structures. Therefore, once seizures have abated, limbic disinhibition responsible for behaviour disorders will appear. Risk factors for psychosis as a neurosurgical complication are as follows: the presence of a right-sided focus, anomalous tissue suggesting an alteration in cell differentiation, hamartomas, and gangliogliomas.15 Our female patient presented symptomatic epilepsy caused by a left cerebral ganglioglioma. In this case, the appearance of de novo epileptic psychoses would be determined by both processes: the surgery itself and the phenomena of forced normalisation, since treatment resulted in a considerable decrease in seizure number and intensity.
Although there are no standard guidelines for treating epileptic psychoses, associating antiepileptic and neuroleptic drugs is frequent. Numerous antiepileptic drugs have been proposed in these cases (carbamazepine, valproic acid, lamotrigine, etc.), but there is no standard treatment at present.16 Most antiepileptic drugs increase hepatic metabolism, which decreases the effective levels of neuroleptic drugs. Patients with epileptic psychoses therefore require higher doses of neuroleptic drugs than do patients with isolated psychosis, which increases the probability of drug interactions. This is why in these cases we suggest using renally metabolised antiepileptic drugs, such as levetiracetam, in association with neuroleptics. There are no controlled trials with levetiracetam for epileptic psychosis. Whereas 2% of the patients on long-term treatment with levetiracetam have experienced behavioural disorders,17 this drug has been confirmed as a safe treatment for mania and bipolar psychosis.18,19 According to our experience, levetiracetam is an ideal drug for use with neuroleptics both during the acute phase of peri-ictal psychosis and on a long-term basis in cases of interictal psychosis.
Differentiating between mental disorders associated with epilepsy according to their temporal relationship with epileptic seizures is clinically and prognostically useful, since it provides important data regarding the treatment and course of the disease. The treatment of peri-ictal or acute mental disorders is oriented towards rigorous control over epileptic seizures, whereas treatment of interictal or chronic disorders resembles that of true psychiatric disorders. Controlled trials are needed to study this condition given that strict seizure control may prevent interictal psychosis, improve quality of life, and decrease level of disability.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: González Mingot C, et al. Psicosis epiléptica periictal, una causa de psicosis reversible. Neurología. 2013;28:81–7.