Analyse the role of the nurse at the end of the life of a critically ill patient.
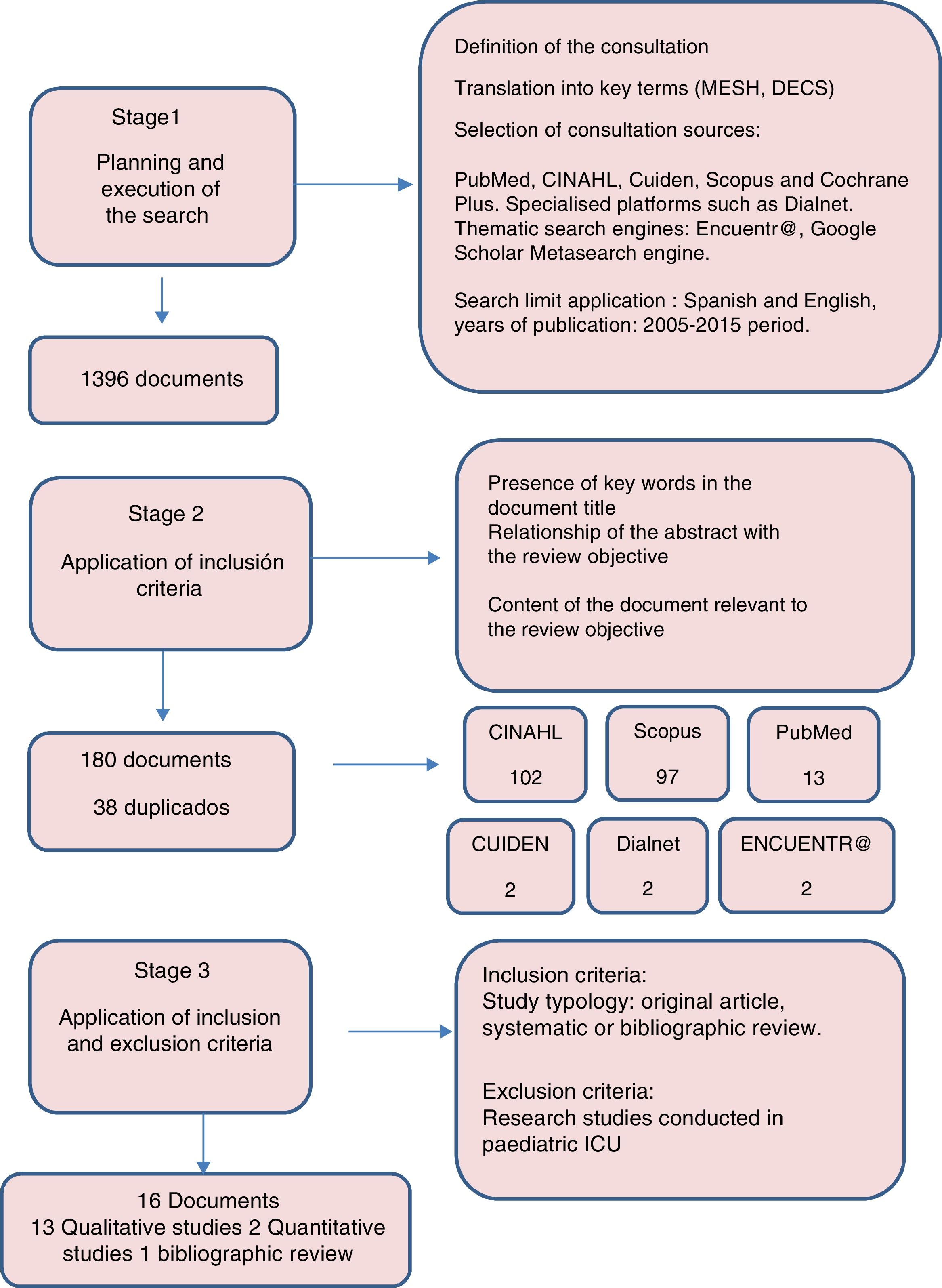
MethodBibliographic review from a search of the health science databases such as PubMed, CINAHL, Cuiden, Scopus, Cochrane, as well as specialised platforms, general and thematic browsers. The limits were language (English or Spanish) and publication date (2005–2015).
Results180 articles met the inclusion criteria, and 16 of them were selected for analysis. The main results were grouped into three categories of analysis: direct patient care, family-focussed care and the nurse's role within the team.
Conclusionsthe described roles place the nurse as a key element in humanising death in the ICU and so nurses can and must lead change, playing an active role in creating strategies that really promote the integration of a palliative care approach in ICU.
Analizar el rol de la enfermera en el cuidado al final de la vida del paciente crítico.
MétodoRevisión bibliográfica a partir de la búsqueda en bases de datos de ciencias de la salud: PubMed, CINAHL, Cuiden, Scopus, Cochrane Plus, y en plataformas especializadas, buscadores generales y temáticos. Los límites establecidos fueron el idioma (español e inglés) y la fecha de publicación (2005-2015).
ResultadosCiento ochenta artículos cumplieron los criterios de inclusión, seleccionándose 16 para su análisis. Los principales resultados se agruparon en tres categorías de análisis: el cuidado directo al paciente, la atención centrada en la familia y el rol dentro del equipo multidisciplinar.
ConclusionesLos roles descritos sitúan a la enfermera como un elemento clave para humanizar la muerte en las UCI, por ello las enfermeras pueden y deben liderar el cambio desempeñando un papel activo en la creación de estrategias que hagan realidad la integración del enfoque de cuidados paliativos en las UCI.
Care of the critically ill end-of-life patient in intensive care units (ICU) has undergone major changes during the last few decades due to the advance of life-sustaining treatments (LST), the rise in elderly patients and/or chronic disease and the higher demand for patient participation in decision-making on their health.1–4 This reality poses major ethical dilemmas for healthcare and establishes the need to humanise the process of dying in the intensive care environment. The debate over the last two decades has led to a major consensus in scientific societies on the aspects to be regarded for end of life quality care of the critically ill patient. This consensus emphasizes the need to incorporate a multidisciplinary approach in taking decisions on the limitations of life-sustaining treatments (LLST) and the integration of palliative care from admittance into the ICU.3,5–8
There is however, an enormous variability in how the LLST is applied in the ICU, with regard to the national and international environment,9 mainly in relation to the frequency with which LLST is decided, the type of therapeutic interventions most frequently withdrawn, the use of advance care directives, the appointment of representatives, the participation from family members in decision making, the extent to which nurses and other professionals are involved and the role of consultants and ethics committees. There are many reasons for this situation and they include differences in cultural environments.2,10,11
Despite acceptance of the practice of LLST, treatment at the end of life for critically ill patients and caring for their needs and the needs of their families continues to pose challenges for the professionals for several reasons: the difficulty in predicting death with precision and the frequency with which the patient's treatment is fragmented between different specialists; the lack of training in palliative care; insufficient communication skills and erroneous consideration of death as a failure of treatment.3
Attention to quality at the end of life for the patients in these units continues to be a challenge, since the curative focus in some cases continues to prolong the agony, at high emotional cost to the patient, their family and the professionals. Decisions at the end of life are often not taken by a multidisciplinary team and the nurses’ contribution towards a biosphychosocial and spiritual focus guaranteeing comprehensive care of the patient and their family continues to be largely irrelevant.12,13
In view of this reality the search for quality end-of-life care for the critically ill patient needs to recognise the role the nurse plays and his or her active involvement in this process. Nurses have their own body of knowledge, a methodological strategy to support the planning of their interventions, a code of ethics and a legal framework to guarantee their actions. Moreover, in the ICU setting, nurses are well placed for establishing close relationships with the patients and their families, getting to know their wishes with regard to treatment and configuring a vision which allows them to integrate both biological and psychosocial aspects in the process of taking end-of-life decisions.12,14 The aim of this study was therefore to analyse the role of the nurse at the end of the life of a critically ill patient.
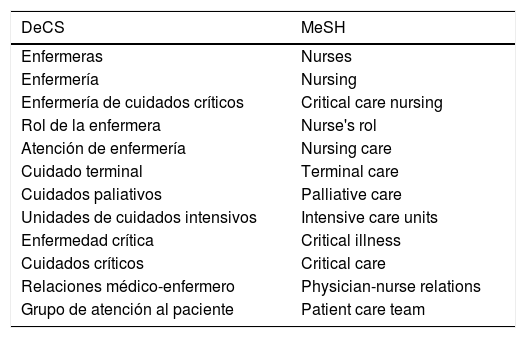
MethodBibliographic review from a search of the health science databases of: PubMed, CINAHL, Cuiden, Scopus and Cochrane Plus. Documents from specialised platforms and thematic search engines were also obtained. For database searches we used Thesaurus of Descriptors of Health Sciences (DeCS) and Medical Subject Headlines (MeSH) (Table 1), and also Boolean operators AND and OR and the following limits were established: language (Spanish and English) and publication date (2005–2015). In the specialised platforms and in the search engines free language was used.
Descriptors used in the searches with controlled language.
| DeCS | MeSH |
|---|---|
| Enfermeras | Nurses |
| Enfermería | Nursing |
| Enfermería de cuidados críticos | Critical care nursing |
| Rol de la enfermera | Nurse's rol |
| Atención de enfermería | Nursing care |
| Cuidado terminal | Terminal care |
| Cuidados paliativos | Palliative care |
| Unidades de cuidados intensivos | Intensive care units |
| Enfermedad crítica | Critical illness |
| Cuidados críticos | Critical care |
| Relaciones médico-enfermero | Physician-nurse relations |
| Grupo de atención al paciente | Patient care team |
Selection criteria of the articles were that in the title several of the key words appeared; that in the abstract the relationship between the theme and the objective was clear for this review and that with regard to study typology, the article was original or a systematic or bibliographic review. In Fig. 1 the selection process of the information was described. In Table 2 the search sentences were presented, together with the limits used and the number of documents obtained.
Search strategies and results of the bibliographic search.
| PubMed | |||||
|---|---|---|---|---|---|
| Search sentence | Limits | Articles obtained | Title selection | Abstract selection | Complete reading |
| (((«Nurses»[Mesh] OR «nursing»[Subheading]) OR «Nurse's Role»[Mesh]) AND «Intensive Care Units»[Mesh]) AND «Terminal Care»[Mesh] | Publication: 2005/01/01–2015/03/31Language: English/Spanish | 55 | 41 | 22 | 4 |
| (((«Nurse's Role»[Mesh] OR «Nursing Care»[Mesh]) AND «Family»[Mesh]) AND «Terminal Care»[Mesh]) AND «Intensive Care Units»[Mesh] | Publication: 2005–2015Language: English/Spanish | 11 | 12 | 8 | 2 |
| («Critical Illness/nursing»[Mesh] OR («Critical Care/ethics»[Mesh] OR «Critical Care/nursing»[Mesh])) AND «Terminal Care»[Mesh] | Publication: 2005–2015Language: English/Spanish | 122 | 33 | 12 | 3 |
| ((«Physician-Nurse Relations»[Mesh] OR «Patient Care Team»[Mesh]) AND «Terminal Care»[Mesh]) AND «Intensive Care Units»[Mesh] | Publication: 2005–2015Language: English/Spanish | 52 | 34 | 16 | 4 |
| CUIDEN | |||||
| (nursing)AND((care)AND((intensive)AND((care)AND(palliative)))) | Publication: 2005–2015 | 17 | 7 | 2 | 2 |
| (nursingAND((professional role)AND((critical care)AND(treatment limitation))) | Publication: 2005–2015 | 0 | 0 | 0 | 0 |
| COCHRANE PLUS | |||||
| (critical care nursing) AND (terminal care) AND (palliative care) | Publication: 2005_2015Language: English/Spanish | 13 | 1 | 1 | 0 |
| (nurse) AND (intensive care unit) AND (terminal care) | Publication: 2005–2015Language: English/Spanish | 20 | 1 | 1 | 0 |
| SCOPUS | |||||
| (TITLE-ABS-KEY (nursing) OR TITLE-ABS-KEY (nurses) OR TITLE-ABS-KEY (nurses's role) AND TITLE-ABS-KEY (terminal care) AND TITLE-ABS-KEY (intensive care)) | Publication: 2005–2015 Subarea «Nursing»Language: English/Spanish | 174 | 112 | 40 | 30 |
| (TITLE-ABS-KEY (nurses) AND TITLE-ABS-KEY(decision making) AND TITLE-ABS-KEY (life support care) AND TITLE-ABS-KEY (intensive care units)) | Publication: 2005–2015Language: English/Spanish | 83 | 60 | 31 | 25 |
| (TITLE-ABS-KEY (nurses) AND TITLE-ABS-KEY (critical care) AND TITLE-ABS-KEY (palliative care)) | Publication:2005–2015Subarea: «Nursing»Language: English/Spanish | 159 | 52 | 30 | 25 |
| SCOPUS | |||||
|---|---|---|---|---|---|
| Search sentence | Limits | Articles obtained | Title selection | Abstract selection | Complete reading |
| (TITLE-ABS-KEY (communication) AND TITLE-ABS-KEY (terminal care) AND TITLE-ABS-KEY (intensive care units)) | Publication: 2005–2015Subarea: «Nursing»Language: English/Spanish | 72 | 37 | 27 | 14 |
| (TITLE-ABS-KEY (physician nurse relations) AND TITLE-ABS-KEY (patient care team) AND TITLE-ABS-KEY (terminal care) AND TITLE-ABS-KEY (intensive care units)) | Publication: 2005–2015 | 9 | 9 | 7 | 3 |
| CINHAL | |||||
| (MH «Critical Care Nursing») AND (MH «Terminal Care») | Publication: 2005–2015Language: English/SpanishSource type:AcademicPublication | 199 | 80 | 54 | 33 |
| (MH «Nursing Role») AND (MH «Terminal Care») AND (MH «Intensive Care Units») | Publication: 2005–2015Language: English/SpanishSource type:AcademicPublication | 18 | 16 | 11 | 10 |
| (MH «Nurses») AND (MH «Palliative Care») AND (MH «Intensive Care Units») | Publication: 2005–2015Language: English/SpanishSource type:Academic publication | 7 | 4 | 3 | 2 |
| (MH «Nurse-Physician Relations») AND (MH «Terminal Care») AND (MH «Intensive Care Units») | Publication: 2005–2015Language: English/SpanishSource type:Academic publication | 10 | 9 | 9 | 7 |
| (TITLE-ABS-KEY (nurses) AND TITLE-ABS-KEY(decision making) AND TITLE-ABS-KEY (life support care) AND TITLE-ABS-KEY (intensive care units)) | Publication: 2005–2015Language: English/Spanish | 83 | 60 | 31 | 25 |
| (TITLE-ABS-KEY (nurses) AND TITLE-ABS-KEY (critical care) AND TITLE-ABS-KEY (palliative care)) | Publication:2005–2015Subarea: «Nursing»Language: English/Spanish | 159 | 52 | 30 | 25 |
| DIALNET | |||||
|---|---|---|---|---|---|
| Search sentence | Limits | Articles obtained | Title selection | Abstract selection | Complete reading |
| Palliative care in the intensive care unit | Publication: 2005–2015 | 14 | 7 | 2 | 1 |
| Physician-nurse relation in the critical care unit | Publication: 2005–2015 | 7 | 5 | 3 | 1 |
| ENCUENTR@ | |||||
| care+intensives+taking decisions+terminal patient | Publication: 2005–2015 | 33 | 6 | 4 | 1 |
| unit of+intensive+care+nursing+death+taking+of+decisions | Publication: 2005–2015 | 16 | 9 | 0 | 0 |
| unit+of+intensive care+nurse's role+death | Publication: 2010–2015 | 63 | 8 | 3 | 1 |
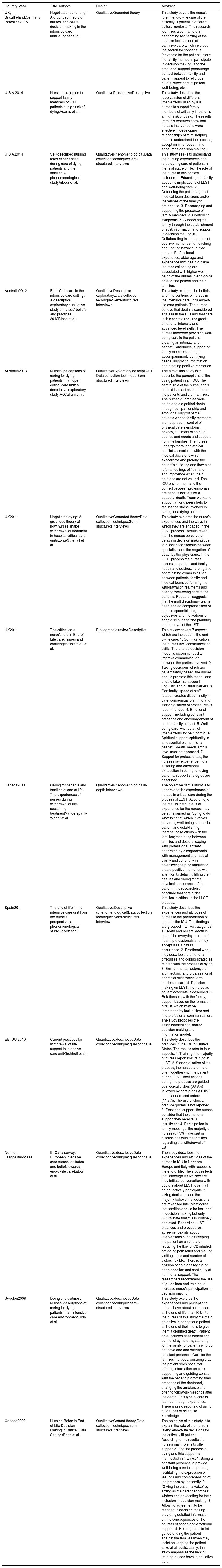
After complete reading of the 180 articles, 16 were finally selected for in-depth analysis (Table 3). The main results were grouped into three analysis categories: direct patient care; family-focused care and the role within the multidisciplinary team.
Articles analysed and included in this review.
| Country, year | Title, authors | Design | Abstract |
|---|---|---|---|
| UK, BrazilIreland,Germany, Palestine2015 | Negotiated reorienting: A grounded theory of nurses’ end-of-life decision-making in the intensive care unitGallagher et al. | QualitativeGrounded theory | This study covers the nurse's role in end-of-life care of the critically ill patient in different cultural contexts. The research identifies a central role in negotiating reorienting of the curative focus to one of palliative care which involves the search for consensus (advocate for the patient, inform the family members, participate in decision making) and the emotional support (encourage contact between family and patient, appeal to religious rituals, direct care at patient well-being, etc.) |
| U.S.A.2014 | Nursing strategies to support family members of ICU patients at high risk of dying.Adams et al. | QualitativeProspectiveDescriptive | This study describes the repercussion of different interventions used by ICU nurses to support family members of critically ill patients at high risk of dying. The results from this research show that nurse's interventions were effective in developing relationships of trust, helping them to understand the process, accept imminent death and encourage decision making. |
| U.S.A.2014 | Self-described nursing roles experienced during care of dying patients and their families: A phenomenological studyArbour et al. | QualitativePhenomenological.Data collection technique:Semi-structured interviews | This study seeks to understand the nursing experiences and roles during care of patients in the final stage of life. The role of the nurse in this context includes: 1. Educating the family about the implications of LLST and well-being care. 2. Defending the patient against medical team decisions and/or the wishes of the family to prolong life. 3. Encouraging and supporting the presence of family members. 4. Controlling symptoms. 5. Supporting the family through the establishment of trust, information and support in decision making. 6. Collaborating in the creation of positive memories. 7. Teaching and tutoring newly qualified nurses. Professional experience, older age and experience with death outside the medical setting are associated with higher well-being of the nurses in end-of-life care for the patient and their families. |
| Australia2012 | End-of-life care in the intensive care setting: A descriptive exploratory qualitative study of nurses’ beliefs and practices 2012Rinse et al. | QualitativeDescriptive exploratory.Data collection technique:Semi-structured interviews | This study explores the beliefs and interventions of nurses in the intensive care units end-of-life care patients. The nurses believe that death is considered a failure in the ICU and that care in this context requires great emotional intensity and advanced level skills. The nurses intervene providing well-being care to the patient, creating an intimate and peaceful ambiance, supporting family members through accompaniment, identifying needs, supplying information and creating positive memories. |
| Australia2013 | Nurses’ perceptions of caring for dying patients in an open critical care unit: a descriptive exploratory study.McCallum et al. | QualitativeExploratory,descriptive.T Data collection technique:Semi-structured interviews | The aim of this study is to describe the perceptions of the dying patient in an ICU. The central role of the nurse in this context is to act as protector of the patients and their families. The nurses guarantee well-being and a dignified death through companionship and emotional support of the patients whose family members are not present, control of physical care symptoms, privacy, fulfilment of spiritual desires and needs and support from the families. The nurses undergo moral and ethical conflicts associated with the medical decisions which exacerbate and prolong the patient's suffering and they also refer to feelings of frustration and impotence when their opinions are not valued. The ICU environment and the conflict between professionals are serious barriers for a peaceful death. Team work and support among peers help to reduce the stress involved in caring for a dying patient. |
| UK2011 | Negotiated dying: A grounded theory of how nurses shape withdrawal of treatment in hospital critical care unitsLong-Sutehall et al. | QualitativeGrounded theoryData collection technique:Semi-structured interviews | This study explores the nurse's experiences and the ways in which they are engaged in the LLST process. Results reveal that the nurses perceive of delays in decision making due to a lack of consensus between specialists and the negation of death by the physicians. In the LLST process the nurses assess the patient and family needs and desires, helping and coordinating communication between patients, family and medical team, performing the withdrawal of treatments and offering well-being care to the patients. Research suggests that the multidisciplinary teams need shared comprehension of roles, responsibilities, objectives and motivations of each discipline for the planning and removal of the LST |
| UK2011 | The critical care nurse's role in End-of-Life care: issues and challengesEfstathiou et al. | Bibliographic reviewDescriptive | This review covers 7 aspects which are included in the end-of-life care. 1. Communication, the nurses lack communication skills. The shared decision model is recommended to improve communication between the parties involved. 2. Taking decisions which are patient/family based, the nurses should promote this model, and should take into account linguistic and cultural barriers. 3. Continuity, speed of staff rotation creates discontinuity in care, consensual planning and standardisation of procedures is recommended. 4. Emotional support, including constant presence and encouragement of patient-family contact. 5. Well-being care, with detail of interventions for pain control. 6. Spiritual support, spirituality is an essential element for a peaceful death, needs at this level must be assessed. 7. Support for professionals, the nurses may experience moral suffering and emotional exhaustion in caring for dying patients, support strategies are described. |
| Canada2011 | Caring for patients and families at end of life: The experiences of nurses during withdrawal of life-sustaining treatmentVanderspank-Wright et al. | QualitativePhenomenologicalIn-depth interviews | The objective of this study is to understand the experiences of nurses in critical care during the process of LLST. According to the results the nucleus of experience for the nurses may be summarised as “trying to do what is right”, which involves providing well-being care to the patient and establishing therapeutic relations with the families; mediating between families and doctors; coping with professional anxiety generated by disagreements with management and lack of clarify and continuity in objectives; helping families to create positive memories with attention to detail, fulfilling their desires and caring for the physical appearance of the patient. The researchers conclude that care of the families is critical in the LLST process. |
| Spain2011 | The end of life in the intensive care unit from the nurse's perspective: a phenomenological studyGálvez et al. | Qualitative:Descriptive (phenomenological)Data collection technique: Semi-structured interviews | This study describes the experiences and attitudes of nurses to the phenomenon of death in the ICU. The findings are grouped into five categories: 1. Death and beliefs, death is part of the everyday routine of health professionals and they accept it as a natural occurrence. 2. Emotional work, they describe the emotional difficulties and coping strategies related with the process of dying 3. Environmental factors, the architectonic and organisational characteristics which form barriers to care. 4. Decision making on LLST, the nurse as patient advocate is described. 5. Relationship with the family, support based on the formation of trust, which may be threatened by lack of time and interprofesional communication. The study proposes the establishment of a shared decision-making and information model. |
| EE. UU.2010 | Current practices for withdrawal of life support in intensive care unitKirchhoff et al. | Quantitative:descriptiveData collection technique: questionnaire | This study describes the practices in the ICU of United States. The results refer to four aspects: 1. Training, the majority of nurses report low training in LLST. 2. Standardisation of the process, the nurses are more often together with the patient during LLST, their actions during the process are guided by medical orders (63.8%) followed by care plans (20.0%) and standardised orders (11.8%). The use of clinical practice guides is not reported. 3. Emotional support, the nurses consider that the emotional support they receive is insufficient. 4. Participation in family meetings, the majority of nurses (87.5%) take part in discussions with the families regarding the withdrawal of LST |
| Northern Europe,Italy2009 | EnCana survey: European intensive care nurses’ attitudes and beliefstowards end-of-life careLatour et al. | Quantitative:descriptiveData collection technique: questionnaire | The study describes the experiences and attitudes of the nurses in ICU in Northern Europe and Italy with respect to the end of life. The study reflects that, although 63.6% declare they initiate conversations with doctors about LLST, over half do not actively participate in taking decisions and the majority believe that decisions are taken too late. Most agree that families should be included in decision making but only 59.3% state that this is routinely achieved. Regarding LLST practices and procedures, agreement exists about interventions such as keeping the patient on a ventilator reducing the flow of O2 inhaled, providing pain relief and making visiting times and number of vistors flexible. There is a division of opinions regarding deep sedation and continuity of nutritional support. The researchers recommend the use of guidelines and training to increase nurse's participation in decision making. |
| Sweden2009 | Doing one's utmost: Nurses’ descriptions of caring for dying patients in an intensive care environmentFridh et al. | Qualitative:descriptiveData collection technique: semi-structured interviews | This study explores the experiences and perceptions nurses have about patient care at the end of life in an ICU. For the nurses of this study the main objective in caring for a patient at the end of their life is to give them a dignified death. Patient care includes assessment and control of symptoms, standing in for the family for patients who do not have one and offering constant presence. Care for the families includes: ensuring that the patient does not suffer, offering information on care, supporting and guiding contact wiht the patient, promoting their presence at the deathbed, changing the ambiance and offering follow-up meetings after the death. This type of care is learned through experience. There was no reporting of using guidelines or scientific knowledge. |
| Canada2009 | Nursing Roles in End-of-Life Decision Making in Critical Care SettingsBach et al. | QualitativeGround theory.Data collection technique: semi-structured interviews | The objective of this study is to explain the role of the nurse in taking end-of-life decisions for the critically ill patient. According to the results the nurse's main role is to offer support during the process of dying and this support is manifested in 4 ways: 1. Being a constant presence to provide well-being care to the patient, facilitating the expression of feelings and comprehension of the process by the family. 2. “Giving the patient a voice” by acting as the defender of their wishes and advocating for their inclusion in decision making. 3. Allowing agreement to be reached in decision making, providing detailed information on the consequences of the courses of action and emotional support. 4. Helping them to let go, defending the patient against the families when they insist on keeping the patient alive at all costs. Lastly, this study emphasise the lack of training nurses have in palliative care. |
| Country, year | Title, authors | Design | Abstract |
|---|---|---|---|
| U.S.A.2009 | The “Big Picture” Communicating With Families About End-of-Life Care in Intensive Care Unit.Liaschenko et al. | QualitativeData collection technique: focus groups | The objective of this study is to understand and document the factors affecting care of the families of critically ill patients in the final stage of their life in the ICU. The results show that the main objective of care of families in this context is to facilitate comprehension of the complete image of the situation or the “big picture”, for which nurses establish relationships of trust with the families, compile information, construct a global vision of the patient status and assist in the communication between families and doctors. |
| Australia2007 | Advocacy at end-of-lifeResearch design: An ethnographic study of an ICUSorensen et al. | QualitativeEthnographic | This study explores the role of the nurse as the defender of dying patients in the ICU. The results show the existence of barriers in fulfilling this role, among which are the biomedical focus, the conflicts between doctors and nurses on patient care, the power relations in the working environment with a lack of nursing autonomy and authority inside the organisations. The researchers state that for their role as advocates to be recognised the nurses need to acquire an advanced level of knowledge and skills in palliative care and be committed both on a care and management level, with the introduction of a focus on comprehensive care in decision making |
| Australia2006 | Fruitful or futile: intensive care nurses’ experiences and perceptions of medical futility.Heland | Qualitative:descriptive, exploratoryData collection technique: semi-structured interviews | This study describes the perceptions and experiences of nurses in the ICU relating to futile treatments. Results show that the nurse feels frustration and experiences moral conflict in the administration of futile treatments. They express concern for the lack of consideration of patient desires in the LLST and the exclusion of nurses from decision making. They describe the nurse's functions as patient advocate, mediator between medical staff and families, educator of families, supporter in comprehending the process and care in the early stages of grief. They suggest that experienced nurses can significantly influence in the management of futile treatment cases. The need for the introduction of a shared decision making model is proposed. |
ICU regulations which limit contact between the patient and their family contribute to the fact that the nurses provide continuous presence and are the primary carers of the end-of-life patients.15–17 The roles adopted under these circumstances involve defence of the patient, guarantee of well-being care,a dignified death, and emotional and spiritual support.
With regard to the role of the nurse advocacy in possible situations of therapeutic intransigence, the nurses take actions to seek acceptance and consensus among the parties involved on the need to limit the LST and establish palliative care when they perceive of the patient's impairment and lack of response to treatments. In these cases they usually intervene communicating their desires to the patient and the family, seeking clarity in the treatment plan and even seeking intervention from authorities such as the healthcare ethics committee to protect the patient from unnecessary suffering or to making the arrangement for the formulation of advance directives.17–25 In turn, they defend the patient against the family's wishes to keep them alive at all costs, guiding the family members towards a global view of the situation, accompanying them in the process of “letting go” of their loved one.18,22,26 The nurses stress the fact that to exercise their role as advocates, reflection and personal analysis need to be made to avoid influencing decisions as much as possible. They believe it is essential to know the patient, the course of their disease, to have enough information from all the parties involved and to have training in palliative care in addition to clinical practice guidelines.16,18,20,24,25,27 Thus Gallagher et al.24 identified the need for nursing organisations to become nurse advocacies in the patients’ interests and those of their families in countries where the focus of palliative care has not yet been sufficiently developed.
Another widely treated aspect in the literature is the reference to wellbeing care, since when the decision for LLST has been made, the nurses offer care to the patient where the goal is to provide wellbeing and a dignified death, free from suffering, so that in some cases they remind the doctors of the need to pay attention to controlling symptoms such as pain, agitation, dyspnoea and even keeping the patient connected to the ventilator to ease the task of breathing.19,20,22,24,28–30
Regarding emotional and spiritual support, Gallagher et al.24 and Adams et al.,29 refer to the importance of talking to the patient even when there is a low level of consciousness and they show that communication is mainly established through touch and/or information on everyday issues, daily care and the people in their environment. The need for guaranteeing that the patient dies accompanied is also considered, and the nurses take steps to encourage contact with the family. In its absence they act as a replacement offering a constant presence, emotional comfort and the guarantee of respect for religious, personal and cultural beliefs.18,22,23,28–30
Family-centred careThe nurses play a vital role in confronting the loss of the loved one and in reducing the feeling of vulnerability and stress which the family members experience in an unknown and highly technological environment. They cover psychoemotional aspects, providing access to information and comprehension on patient status, supporting the taking of decisions and accompanying the families both emotionally and spiritually during the process. 22,23,25,28–30
The nurse stands out as the facilitator of communication between the medical team and the family and as the mediator in the process of taking shared decisions. This role is classified as a key aspect in quality of care and as one of the most demanding and difficult jobs to perform by the nurses in these units. 18,19,24,25,29 The extent of the nurses’ knowledge is vast and they liase between the professionals and the family so that an overall idea of the situation is obtained whereby the families can understand what is happening and prepare for the possible death of the patient.25 To do this they become educators, explaining medical information in a comprehensible language, clarifying the potential consequences of the different interventions and encouraging meetings between family members and the medical team to provide a response to the demands of the information.18,21,25,26 Although they set limits to prevent medical issues being raised, they insist on the need for the family to be informed about the worsening of the patient's status at all times.18,24–26
Once the LLST option has been contemplated, the nurse adopts the role of guide and educator as a normal part of family interaction. During this phase evaluation focuses on the knowledge the families have on the implications of the removal of the LST and well-being care.22
Regarding accompaniment and emotional support as aids to coping, several studies15,17,18,21,22,30 show that the nurses usually adopt different strategies for approach, communication and sensitive help to the family member needs. According to Latour et al.,20 families say they feel more satisfied with the LLST decision when they have regular discussions with the healthcare professionals on end-of-life planning. Here the nurses create spaces for doubts to be raised and feelings to be expressed, sometimes with the duel proposal of becoming familiar with the patient and allowing the family members to express their feelings and reflect upon the process.18,20,24–26,30
In view of the worsening of the patient prognosis and imminent death, the nurses intervene, aiming the attention of the family towards relief of symptoms and well-being care, fostering greater contact with the loved one and supporting the expression of religious and departure from life rituals.16,23,24,27
Facilitating contact between families and patient is priority when the nurses perceive that the families do not appreciate the gravity of the situation.17,20,22,24–26,29,30 Fridh et al.27 suggest the need to approach patients and families as a step towards overcoming the dehumanisation which solitary death entails. In the literature the need for modification of the strict ICU regulations limiting contact between families and terminally ill patients are appreciated.17,20,24 Some nurses tend to waiver visiting times and hours as a strategy to offer emotional support and greater contact between the family and the patient.24,26 In turn, faced with possible death from the LLST, the nurses promote the presence of the family members by negotiating with the physicians to delay the time of removal of the LST until the family has bene notified and their presence is guaranteed.21,22,24,29 A recurrent concern for nurses is that of providing an intimate environment for the stimulation of privacy and spiritual support needed by the patient.16,19–21,24,26,29,30
The nurse's role within the interdisciplinary teamResearch studies reflect that, although nurses acknowledge the role the doctors have as those in charge of taking decisions on the establishment and limitation of the LST, they may affect this decision and focus attention on palliative care.17,19,24 According to Kirchhoff et al.,16 the majority of critical care nurses in the United States participate in meetings with the families where they discuss LLST and a small percentage initiate these meetings. In Europe, the study by Latour et al.20 also indicates that the nurses state they iniate conversations with the doctors on this issue.
The nurses’ involvement in taking decisions is influenced by their perception of the suffering of the patient, their considerations for ethical and moral implications of therapeutic intransigence, their religious beliefs and years of experience. Some research studies point out that the greater their expertise, knowledge and training, the higher the probability that they will be considered as consultants and their opinions will be taking into account by the medical team.16,20,21,24 Long-Sutehall et al.19, describe that in the LLST context, some doctors seek the opinion of nurses because they spend more time with the patients and their families and they are considered to be more aware of their wishes. However, findings from several research studies underline that the current trend of end-of-life care in the ICU does not focus on collaboration.17,20,21,27
Adams et al.29 report that the attitudes of nurses may range from avoidance to open discussion of issues and Gallagher et al.24 suggest that nurses have a higher predisposition to get involved in family support by informing when their opinion is taking into account by other members of the team. However, some are reticent about confrontation with the doctors and these leads to them adopting a passive or neural role. The studies included in this review attach great importance to experience as the requisite for assuming roles in end-of-life care. Nurses with less experience tend to be overwhelmed by patient care and have difficulties in adopting a global viewpoint of the situation which is essential for appropriate support throughout the process.16,18,20 Years of experience, training in palliative care and in bioethical challenges, means a broad outlook may be obtained and they increase the confidence in their ability to care for the patient, give an opinion in debates with the medical team and suggest questions to start conversations with the families regarding end-of-life care.16,20,24 Additional experience with death outside the medical environment is connected to a higher level of confidence in patient and family care. Some research studies reflect that the best learning and assimilation of the roles described may be learned with tutoring and observation of the most experienced nurses.18,22 Arbour et al.22 mention that the professionals take on the role of mentor and consider that this is something which encourages a healthier working environment. Interventions relating to this role include assessing the degree of ease with which newly qualified nurses care for their patients, probe into their experiences with death within and without the medical environment, explore their personal circumstances which may interfere in care and guide them on the aspects which they should focus their attention on and the possible courses of action.18,22
DiscussionIn the care environment the decision on LLST and end-of-life care continue to be a major source of conflict between the family, patients and professionals and a challenge for the intensive care teams. Nursing professionals believe it is necessary for them to participate in taking decisions and one of their main goals is to define their role within the multidisciplinary team and to accept their role as part of the comprehensive care of the patient and their family at the end of life.8 The EPIPUSE multicentre study conducted in Spain reflects that there is a low percentage of cases in which nurses propose limited treatment probably due to the face that they do not take part in clinical sessions.9 In the European context, although they do not actively participate with the medical team in end-of-life discussions the majority of nurses state that they initiate conversations with doctors on this issue.20
With regard to direct patient care the literature emphasizes the role of the nurse as advocate or protector of the patient against possible situations of therapeutic intransigence, in keeping with the ethical code regulations of the profession in safeguarding compliance of the rights and safety of people who are in their care.17,18,20–25
Another aspect to be highlighted is the need to guarantee well-being care, which includes symptom control, physical care and appropriateness of ambiance, with particular reference to pain control rather than control of other symptoms. This may be related to the finding in different research studies of insufficient training in palliative care and the low use of scientific knowledge in guiding clinical practice.19,20,22,24,28–30
There is little reference to emotional support to patients, although studies stress the importance of the patient having company and for death not to occur in solitude, together with the consideration of the spiritual needs as an important element to guarantee a peaceful death.18,22,23,28–30
There is greater reference to family-centred care in the literature, since the frequent impairment in the level of consciousness and the ability to communicate of patients admitted to ICU means that the families are an important source of information. Family support is an essential aspect of care in promoting confrontation and empowerment in decision-making. The role of the nurse stands out as a facilitator of communication between the parties involved, coordinating exchange of relevant information and aiming attention at families so that they may understand the patient's status.15,1719,22–24,27
Within the multidisciplinary team, the nurse has the role of “reorienting negotiator” participating in family meetings and initiating conversations for taking decisions.16,17,19,20,22,24,29The way in which the nurses with more experience take on the role as informal tutors of the newly qualified nurses is outstanding. The more experienced nurses also perform the end-of-life care to the patient in a more satisfactory manner.22,27 for this reason, Galvez ET al.17, and Bach et al.18 state the need to include the experienced nurse as a key element in the management of end-of –life care through their role as mentors.
Most of the articles included in this review refer to research studies carried out in English-speaking countries and there is therefore a need to carry out both qualitative and quantitative investigations to describe and analyse the role of the nurse in the end-of-life process for critically ill patients in broader contexts. We also suggest that subsequent reviews cover this issue in the context of the Neonatal Intensive Care Units (NICU) and Paediatric Intensive Care Units (PICU).
Finally we should mention the limitations of this study since although the aim was to analyse the largest number possible of articles, we acknowledge the implicit subjectivity in defining the search criteria and the possibility of other interpretations
Providing greater thoroughness of the same.
ConclusionsIn this review the nurse is described as the key element for humanising the process of dying in the ICU and his or her action or inaction is significant to the experience of the patient and their family during this process. The analysis carried out in this review highlights that the role of the nurse at the end of the life of a critically ill patient is the relationship with direct patient care, family-focused care and their role within the multidisciplinary team. The effective expression of the nurses roles in these circumstances seeks to offer a response to the patient and family needs, acting as advocate of the patient, providing well-being care, relieving anxiety, helping them to cope and participate in decision-making and guaranteeing a dignified death as a result.
The literature underlines the nurse's role within the team in two ways, one as a mentor/tutor of newly qualified nurses, informally undertaken by nurses with greater experience and the other as the reorientation of care, participating in meetings with family members and initiating conversations on decision making. An essential element in incorporation of palliative care to ICU is the active participation of nurses in discussions within the multidisciplinary teams relating to the transfer of critical care to palliative care. The nurses are able to offer a biopsychosocial viewpoint of the situation and for this specific training in palliative care and bioethics is essential, that they may be able to resolve the ethical conflicts they encounter. Special interest resides in the fact that this review is a source of information to bring light to the clarification of the nurse's role within the multidisciplinary team in end-of-life care in the ICU. It is believed that nurses can and should be the leaders of change and perform an active role in the creation of strategies to integrate a palliative care focus in the intensive care units.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: González-Rincón M, Díaz de Herrera-Marchal P, Martínez-Martín ML. Rol de la enfermera en el cuidado al final de la vida del paciente crítico. Enferm Intensiva. 2019;30:78–91.