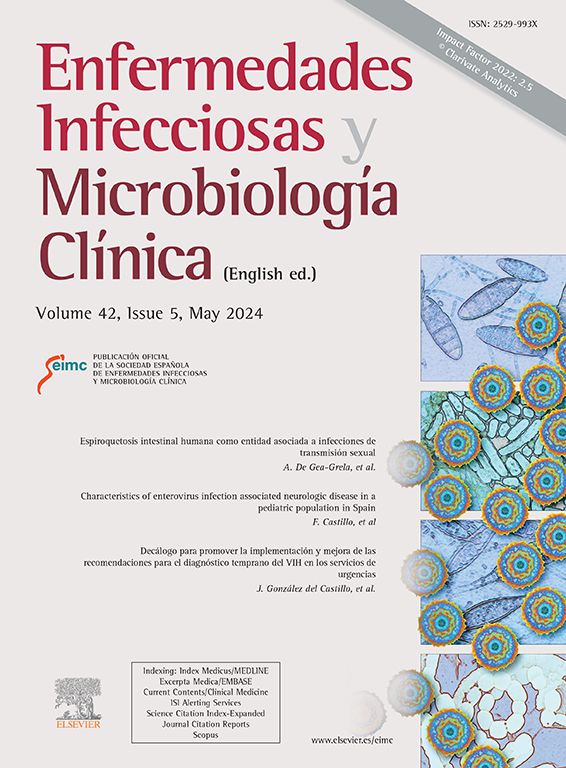
This was the case of a 65-year-old male referred to the Dermatology Department presenting with non-pruritic skin lesions coursing for one day, which began on his forehead and spread following a cranial-caudal path. On the same day that the lesions began, he presented fever, diarrhoea and abdominal pain. The patient was being followed up by the Oncology Department for locally advanced distal oesophageal cancer that was treated with paclitaxel-carboplatin and nivolumab, suspended one year previously and four months previously, respectively. He was undergoing treatment with allopurinol for gout arthritis, co-trimoxazole, and prednisone, in a tapering-off regimen. The patient denied taking and/or having taken epidermal growth factor receptor inhibitors. Physical examination revealed papules and pustules with a monomorphic appearance distributed over the scalp, forehead, cheeks, chest, abdomen, back and extensor surfaces of the arms (Fig. 1).
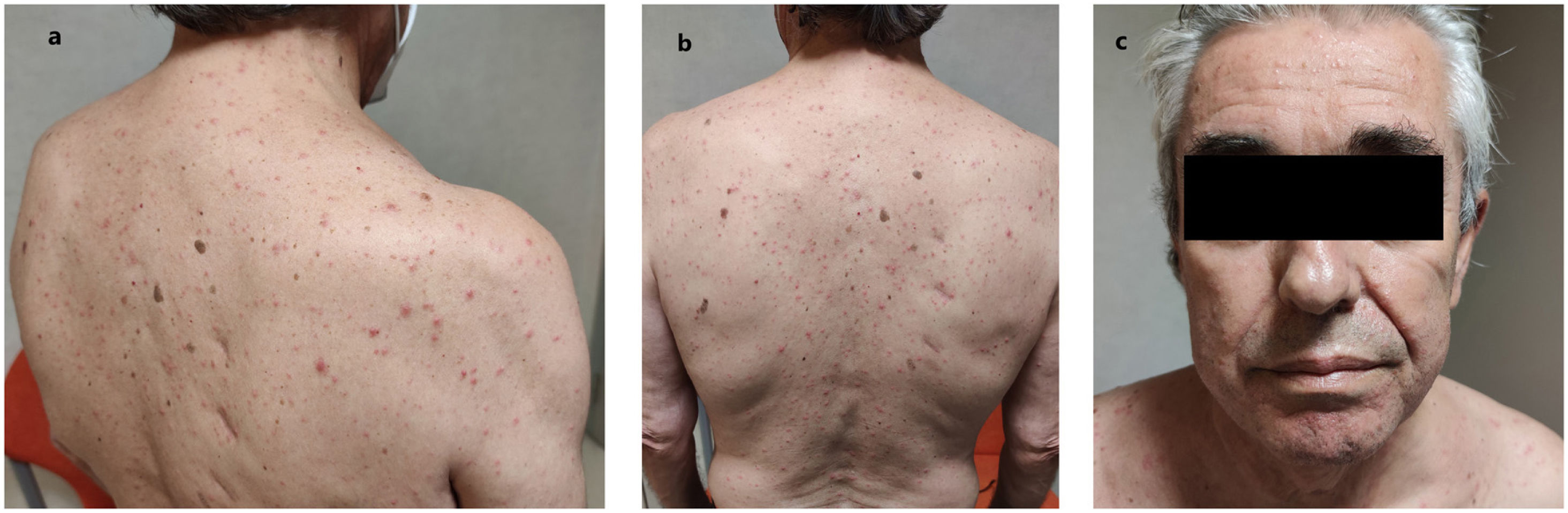
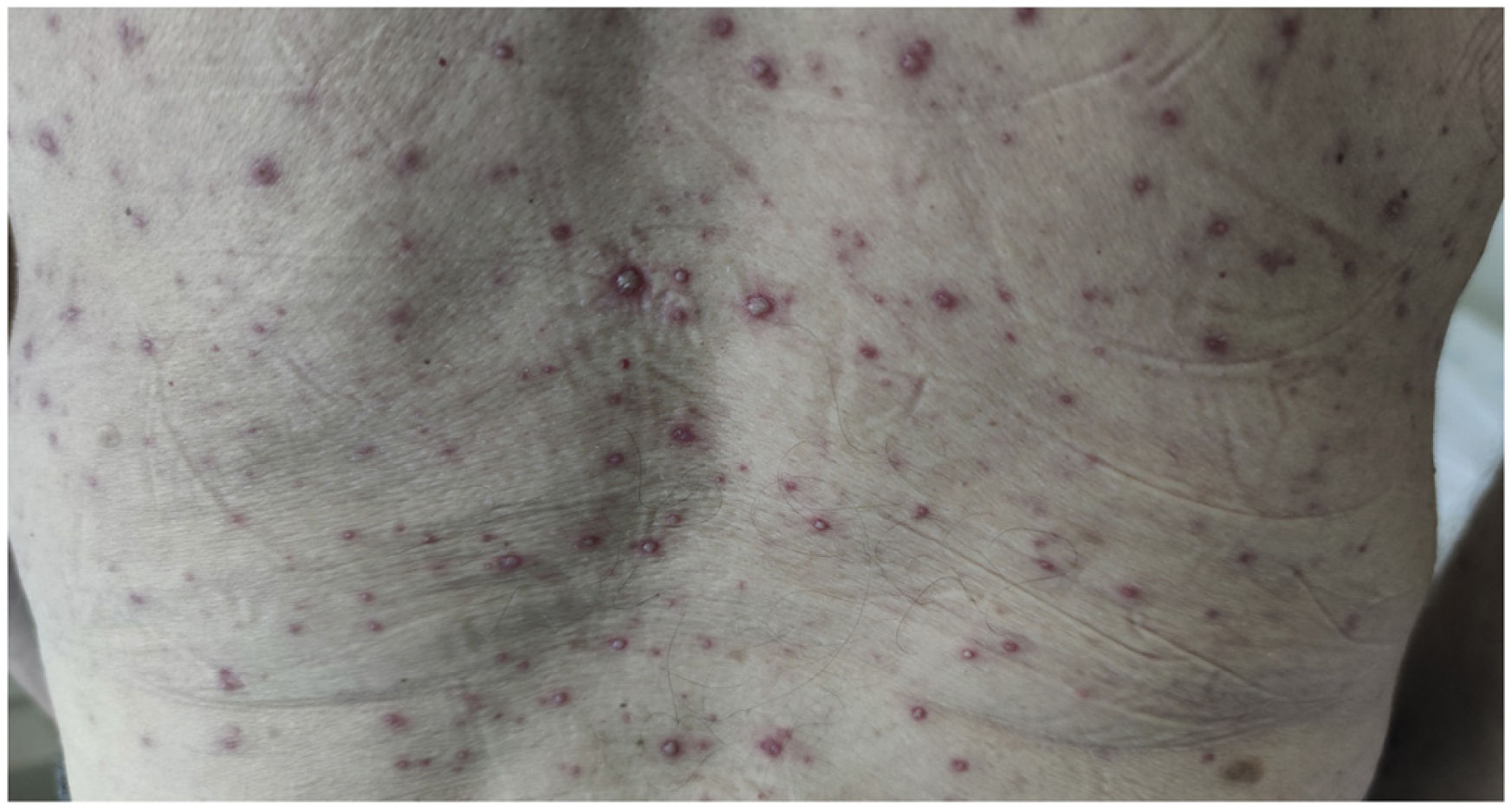
Clinical courseA sample was taken for herpes virus PCR from one of the pustules, oxygen saturation was determined to be 96% and a chest X-ray was performed, which was unremarkable. The patient was hospitalised and oral valacyclovir was prescribed. Three days later, he presented papules, pustules and scabs with a polymorphous appearance (Fig. 2). After five days, varicella-zoster virus was amplified in the PCR. The patient stated that he did not remember having chickenpox in childhood or having been vaccinated.
Closing remarksChickenpox is a disease caused by the varicella-zoster virus. It is an infectious disease that usually appears in childhood with a good prognosis, while it presents in adults less frequently and usually involves a more serious clinical course.1,2 Skin lesions in chickenpox are generally polymorphic and usually appear following a cranial-caudal distribution. However, in cases of very short evolution they can adopt a monomorphic acneiform morphology, which makes diagnosis more difficult.3 Some data that can support the diagnosis include frontal and scalp involvement and the presence of systemic symptoms such as fever, dyspnoea, abdominal pain, vomiting or diarrhoea, among others.4,5 In immunosuppressed patients, it is important to take into account chickenpox as a differential diagnosis because the clinical symptoms may be serious.1,2,5 Oxygen saturation and chest X-ray are useful in determining if there is lung involvement.4 Given the slightest clinical suspicion, a herpes virus PCR of any of the lesions with fluid content can be requested, and in immunosuppressed patients, empiric treatment with oral acyclovir, valacyclovir, famciclovir or brivudine should be initiated if the clinical symptoms are mild or moderate and with intravenous acyclovir in the event of severe clinical symptoms.1,4,6 Another important aspect to bear in mind is that primary infection with varicella-zoster virus is very contagious and may begin to be transmitted two days before the onset of the skin rash. Transmission of the virus is usually airborne, but it can also occur through contact with skin lesions due to the large amount of virus in the fluid content of the vesicles.1 For this reason, it is important to isolate these patients and ensure that they avoid any contact with people who do not have antibodies against the varicella-zoster virus.2,6 The differential diagnosis would include acneiform eruption due to toxicity of epidermal growth factor receptor inhibitors or steroids, which were ruled out, the first one because they were not part of the patient's treatment and the second due to the decrease in the dose of prednisone with regard to the previous weeks. These clinical symptoms result in monomorphic acneiform lesions, but systemic symptoms are absent.7,8
The importance of considering chickenpox in immunosuppressed patients who present a very short-lasting monomorphic acneiform eruption accompanied by systemic symptoms, and the importance of assessing the presence of pulmonary involvement, of establishing early treatment at the slightest suspicion and of isolating the patient so that they do not come into contact with people who have not had chickenpox is highlighted.