Prevalence of alcohol consumption is high in the general population and generates specific problems at the workplace.
ObjectiveTo establish benchmarks between levels of alcohol consumption and cardiovascular risk variables and metabolic syndrome.
MethodsA cross-sectional study of 7644 workers of Spanish companies (2828 females and 4816 males). Alcohol consumption and its relation to cardiovascular risk was assessed using Framingham calibrated for the Spanish population (REGICOR) and SCORE, and metabolic syndrome was assessed using modified ATPIII and IDF criteria and Castelli and atherogenic index and triglycerides/HDL ratio. A multivariate analysis was performed using logistic regression and odds ratios were estimated.
ResultsStatistically significant differences were seen in the mean values of the different parameters studied in prevalence of metabolic syndrome, for both sexes and with modified ATPIII, IDF and REGICOR and SCORE. The sex, age, alcohol, and smoking variables were associated to cardiovascular risk parameters and metabolic syndrome. Physical exercise and stress are only associated to with some of them.
ConclusionsThe alcohol consumption affects all cardiovascular risk parameters and metabolic syndrome, being more negative the result in high level drinkers.
La prevalencia del consumo de alcohol es elevada en población general y genera una problemática específica en el ámbito laboral.
ObjetivosEstablecer parámetros comparativos entre niveles de consumo de alcohol, variables de riesgo cardiovascular y síndrome metabólico.
MétodosEstudio descriptivo transversal en 7.644 trabajadores de empresas españolas (2.828 mujeres y 4.816 varones). Se valora el consumo de alcohol y su relación con riesgo cardiovascular mediante la herramienta de Framingham calibrada para la población española (REGICOR) y SCORE, y síndrome metabólico con ATP-III modificado e IDF e índices aterogénicos o de Castelli y triglicéridos/HDL. Se realiza análisis multivariante mediante regresión logística y se determinan las odss ratio.
ResultadosSe observan diferencias estadísticamente significativas en los valores medios de los diferentes parámetros estudiados en prevalencia de síndrome metabólico, para ambos sexos y con ATP-III modificado, IDF y en REGICOR y SCORE. Las variables sexo, edad, consumo de alcohol y de tabaco se asocian con parámetros de riesgo cardiovascular y síndrome metabólico. El ejercicio físico y estrés lo hacen solo con algunas de ellas.
ConclusionesEl consumo abusivo de alcohol, influye negativamente en todos los parámetros de riesgo cardiovascular y síndrome metabólico, siendo más negativo el resultado en altos niveles de consumo.
The consumption of alcohol, as that of other drugs, is highly prevalent in the general population and is of particular concern in the labor force because of its impact (diseases, work accidents, absenteeism, work disability, decreased productivity, etc.). The harmful effects of alcohol include its impact on the cardiovascular system, and specifically on metabolic syndrome (MS), as well as other effects such as liver disease, associated mental disorders, and different types of cancer.
There are studies in the literature relating alcohol consumption to cardiovascular risk (CVR), some of them after long-term follow-up, such as the one conducted in US males from 1979 to 2005, which found a clear statistical relationship between alcohol consumption and MS regardless of the type of alcohol and with all consumption levels, with HDL reduction and increased blood glucose and triglyceride levels and blood pressure. Such effects were more marked in the presence of prior overweight and obesity.1 Similar results were reported in a male Korean population of 4505 subjects followed up for three years with no prior diagnosis of MS. Results showed a greater risk of MS in men who had drunk alcohol over a longer period and in greater amounts, as compared to data collected from non-drinkers or former drinkers.2
In the labor sphere, alcohol consumption needs to be looked at seriously if we wish to prevent risks to the health of workers, not to mention workplace or traffic accidents, which may also be related to alcohol intake. There is a need for support programs that provide adequate information to the workers concerned if a more effective approach is to be implemented.
These activities, which are the responsibility of occupational physicians working in companies and other organizations, are included in the specialist training program3 and comprise care, training and information aspects, along with epidemiological research derived from collective health monitoring. The most effective actions with regard to alcohol consumption may be performed as health promotion initiatives.
Work regulations in Spain are derived from the Constitution,4 which states that public authorities are responsible for occupational health and safety (Art. 40) and both guarantees the right to a working environment adequate for personal development and establishes the legal requirement to preserve it (Art. 45). These regulations include those aimed at the prevention and care of problems related to alcohol and other drugs, and they are also referred to in legal regulations regarding occupational health and safety.
The International Labour Organization (ILO) stresses the serious impact of the consumption of alcohol and/or other drugs on the working environment, and states that such consumption affects a high number of workers, causing disruption in the workplace and in work performance at all levels and in particular affecting occupational safety and productivity. Moreover, its impact extends to the family as well as fellow workers.5–7
The purpose of this study was to assess in a working population the impact of alcohol consumption and other variables on CVR, estimated using the Framingham tool calibrated for the Spanish population (REGICOR) and SCORE,8 and on MS using the modified ATP-III and IDF models, and atherogenic or Castelli and triglycerides/HDL indices.9
Patients and methodsA descriptive, cross-sectional study was conducted during 2010–2011 of 7644 workers from different companies in the service sector in the Mediterranean area of Spain (2828 females and 4816 males). Workers were selected using random number tables from all workers attending the regular health check-ups carried out by the companies, themselves. Fifty percent of the 15,288 check-ups were selected.
Workers provided written authorization for the use of data for epidemiological purposes, and approval was obtained from the ethics committee of Complejo Hospitalario de Mallorca and the health and safety committees of the companies concerned, as required by the applicable regulations for the prevention of occupational risks.
Both alcohol consumption and the type of alcohol consumed over the previous month were assessed using a questionnaire prepared by the authors. Grams of alcohol and standard drinking units (SDUs), which are equivalent in Spain to 10g of pure alcohol, were calculated from these data.10
To assess alcohol consumption, grams of alcohol were calculated using the formula: g of alcohol=(proof×cc of drink×0.8)/100. The classification prepared by Socidrogalcohol was used to determine the type of consumer.11,12 According to this classification, women and men who drink less than 14 and 21 SDUs respectively per week are considered to be low risk drinkers, while women and men who drink between 14 and 21 SDUs and between 21 and 35 SDUs respectively are considered to be risk drinkers, and consumption of more than 21 SDUs weekly in women and more than 35 SDUs weekly in men is considered to represent heavy drinking.
The study measured laboratory variables including lipid profile (total, LDL, and HDL cholesterol), fasting glucose and gamma-GT (GGT), anthropometric and clinical variables such as the body mass index (BMI), waist circumference (WC), body fat measured by bioimpedanciometry, and blood pressure. CVR was also assessed using the Framingham tool calibrated for the Spanish population (REGICOR) and the SCORE model. MS was assessed using the modified ATP-III and IDF models and, finally, the atherogenic or Castelli index, obtained from the total cholesterol/HDL ratio, and the index obtained from the triglycerides/HDL ratio.
Smoking and physical exercise levels were based on the medical histories. Physical activity was categorized as no exercise, sporadic exercise (when practiced once or twice weekly), and regular exercise (when done at least three times weekly for at least 30min daily). Stress was assessed using the Siegrist effort reward imbalance model. The cut-off point established for stress was 1.13
Laboratory tests were separately performed in males and females because we were interested in knowing the association between alcohol consumption and the different components of CVR in each sex.
The cut-off points established in binary logistic regression analyses were as follows: triglycerides >200, total cholesterol >240, LDL cholesterol >160, HDL cholesterol <40, total/HDL cholesterol ≥4.5 in females and ≥5 in males, LDL/HDL >3, blood glucose >126, the BMI with overweight and obesity, blood pressure >140/90, moderate-high REGICOR, high SCORE, the presence of MS, waist circumference >88cm in females and >102 in males.
Statistical analysisA Student's t or ANOVA test was used to compare means, and a Chi-square test using contingency tables was used to compare proportions. To establish associations between the different variables (alcohol, smoking, physical exercise, stress, age, and sex) and the different parameters related to the CVR and MS tested, a multivariate analysis was performed using binary logistic regression to determine the odds ratios. A value of p<0.05 was considered statistically significant in all cases. Analyses were performed using G-Stat v.2.0 statistical software.
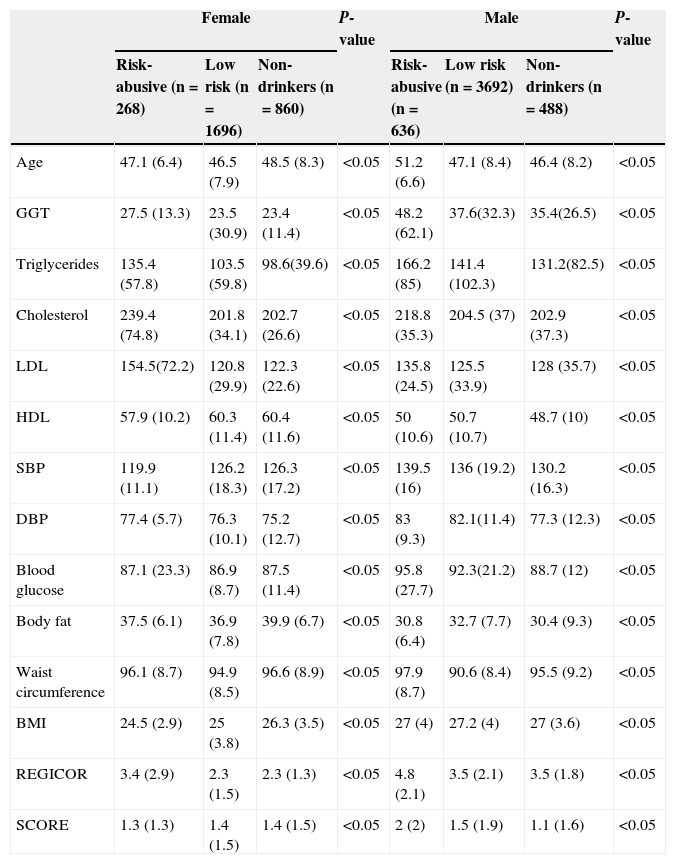
ResultsThe mean values of the different CVR parameters showed differences depending on alcohol consumption. In males, these parameters were usually more unfavorable in the group of people with high alcohol consumption levels, while these differences were not seen among low and non-drinkers. Table 1 shows the complete data.
Mean values of the different cardiovascular risk parameters by alcohol consumption level and sex.
| Female | P-value | Male | P-value | |||||
|---|---|---|---|---|---|---|---|---|
| Risk-abusive (n=268) | Low risk (n=1696) | Non-drinkers (n=860) | Risk-abusive (n=636) | Low risk (n=3692) | Non-drinkers (n=488) | |||
| Age | 47.1 (6.4) | 46.5 (7.9) | 48.5 (8.3) | <0.05 | 51.2 (6.6) | 47.1 (8.4) | 46.4 (8.2) | <0.05 |
| GGT | 27.5 (13.3) | 23.5 (30.9) | 23.4 (11.4) | <0.05 | 48.2 (62.1) | 37.6(32.3) | 35.4(26.5) | <0.05 |
| Triglycerides | 135.4 (57.8) | 103.5 (59.8) | 98.6(39.6) | <0.05 | 166.2 (85) | 141.4 (102.3) | 131.2(82.5) | <0.05 |
| Cholesterol | 239.4 (74.8) | 201.8 (34.1) | 202.7 (26.6) | <0.05 | 218.8 (35.3) | 204.5 (37) | 202.9 (37.3) | <0.05 |
| LDL | 154.5(72.2) | 120.8 (29.9) | 122.3 (22.6) | <0.05 | 135.8 (24.5) | 125.5 (33.9) | 128 (35.7) | <0.05 |
| HDL | 57.9 (10.2) | 60.3 (11.4) | 60.4 (11.6) | <0.05 | 50 (10.6) | 50.7 (10.7) | 48.7 (10) | <0.05 |
| SBP | 119.9 (11.1) | 126.2 (18.3) | 126.3 (17.2) | <0.05 | 139.5 (16) | 136 (19.2) | 130.2 (16.3) | <0.05 |
| DBP | 77.4 (5.7) | 76.3 (10.1) | 75.2 (12.7) | <0.05 | 83 (9.3) | 82.1(11.4) | 77.3 (12.3) | <0.05 |
| Blood glucose | 87.1 (23.3) | 86.9 (8.7) | 87.5 (11.4) | <0.05 | 95.8 (27.7) | 92.3(21.2) | 88.7 (12) | <0.05 |
| Body fat | 37.5 (6.1) | 36.9 (7.8) | 39.9 (6.7) | <0.05 | 30.8 (6.4) | 32.7 (7.7) | 30.4 (9.3) | <0.05 |
| Waist circumference | 96.1 (8.7) | 94.9 (8.5) | 96.6 (8.9) | <0.05 | 97.9 (8.7) | 90.6 (8.4) | 95.5 (9.2) | <0.05 |
| BMI | 24.5 (2.9) | 25 (3.8) | 26.3 (3.5) | <0.05 | 27 (4) | 27.2 (4) | 27 (3.6) | <0.05 |
| REGICOR | 3.4 (2.9) | 2.3 (1.5) | 2.3 (1.3) | <0.05 | 4.8 (2.1) | 3.5 (2.1) | 3.5 (1.8) | <0.05 |
| SCORE | 1.3 (1.3) | 1.4 (1.5) | 1.4 (1.5) | <0.05 | 2 (2) | 1.5 (1.9) | 1.1 (1.6) | <0.05 |
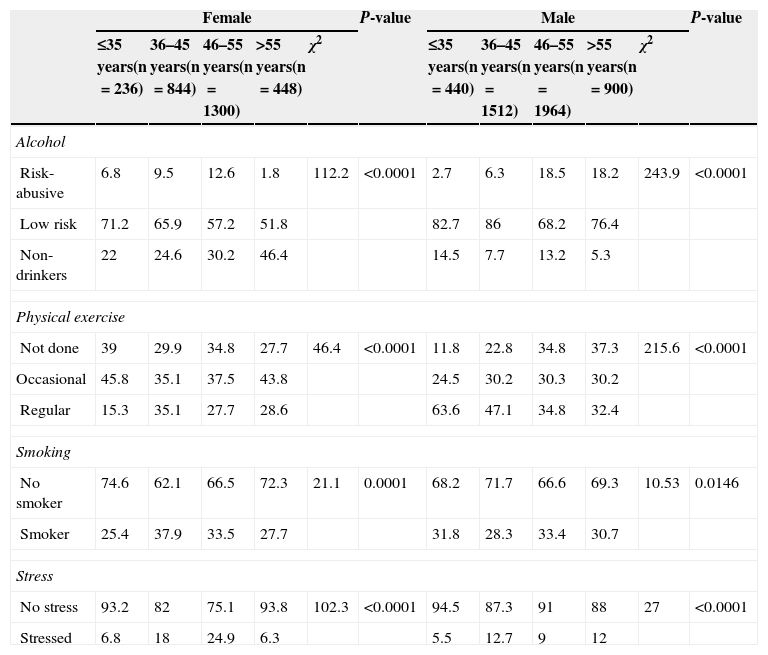
When sample distribution based on the different lifestyle choices was assessed, with both sex and age group, being taken into consideration, a gradual increase with age in the prevalence of both risky or abusive alcohol consumption or lack of physical exercise was seen in males, but not in females. As regards smoking and stress levels, no relationship was seen between the prevalence rates found and age in either sex. Table 2 shows the complete data.
Sample distribution by alcohol consumption, smoking, physical exercise, and stress by age and sex.
| Female | P-value | Male | P-value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ≤35 years(n=236) | 36–45 years(n=844) | 46–55 years(n=1300) | >55 years(n=448) | χ2 | ≤35 years(n=440) | 36–45 years(n=1512) | 46–55 years(n=1964) | >55 years(n=900) | χ2 | |||
| Alcohol | ||||||||||||
| Risk-abusive | 6.8 | 9.5 | 12.6 | 1.8 | 112.2 | <0.0001 | 2.7 | 6.3 | 18.5 | 18.2 | 243.9 | <0.0001 |
| Low risk | 71.2 | 65.9 | 57.2 | 51.8 | 82.7 | 86 | 68.2 | 76.4 | ||||
| Non-drinkers | 22 | 24.6 | 30.2 | 46.4 | 14.5 | 7.7 | 13.2 | 5.3 | ||||
| Physical exercise | ||||||||||||
| Not done | 39 | 29.9 | 34.8 | 27.7 | 46.4 | <0.0001 | 11.8 | 22.8 | 34.8 | 37.3 | 215.6 | <0.0001 |
| Occasional | 45.8 | 35.1 | 37.5 | 43.8 | 24.5 | 30.2 | 30.3 | 30.2 | ||||
| Regular | 15.3 | 35.1 | 27.7 | 28.6 | 63.6 | 47.1 | 34.8 | 32.4 | ||||
| Smoking | ||||||||||||
| No smoker | 74.6 | 62.1 | 66.5 | 72.3 | 21.1 | 0.0001 | 68.2 | 71.7 | 66.6 | 69.3 | 10.53 | 0.0146 |
| Smoker | 25.4 | 37.9 | 33.5 | 27.7 | 31.8 | 28.3 | 33.4 | 30.7 | ||||
| Stress | ||||||||||||
| No stress | 93.2 | 82 | 75.1 | 93.8 | 102.3 | <0.0001 | 94.5 | 87.3 | 91 | 88 | 27 | <0.0001 |
| Stressed | 6.8 | 18 | 24.9 | 6.3 | 5.5 | 12.7 | 9 | 12 | ||||
Data are given as mean (SD).
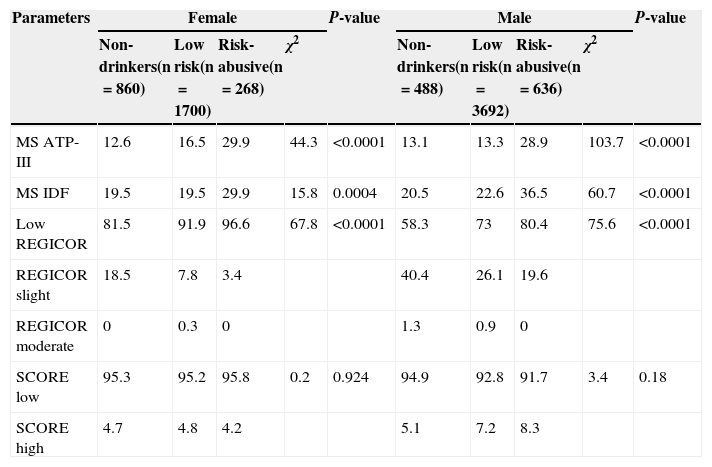
Statistically significant differences were seen in MS prevalence with both the modified ATP-III and IDF models, and in the different REGICOR values, depending on alcohol consumption in both females and males. These differences were not seen when CVR was assessed using the SCORE tool (Table 3).
Prevalence of metabolic syndrome and the different REGICOR and SCORE values by alcohol consumption level by sex.
| Parameters | Female | P-value | Male | P-value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Non-drinkers(n=860) | Low risk(n=1700) | Risk-abusive(n=268) | χ2 | Non-drinkers(n=488) | Low risk(n=3692) | Risk-abusive(n=636) | χ2 | |||
| MS ATP-III | 12.6 | 16.5 | 29.9 | 44.3 | <0.0001 | 13.1 | 13.3 | 28.9 | 103.7 | <0.0001 |
| MS IDF | 19.5 | 19.5 | 29.9 | 15.8 | 0.0004 | 20.5 | 22.6 | 36.5 | 60.7 | <0.0001 |
| Low REGICOR | 81.5 | 91.9 | 96.6 | 67.8 | <0.0001 | 58.3 | 73 | 80.4 | 75.6 | <0.0001 |
| REGICOR slight | 18.5 | 7.8 | 3.4 | 40.4 | 26.1 | 19.6 | ||||
| REGICOR moderate | 0 | 0.3 | 0 | 1.3 | 0.9 | 0 | ||||
| SCORE low | 95.3 | 95.2 | 95.8 | 0.2 | 0.924 | 94.9 | 92.8 | 91.7 | 3.4 | 0.18 |
| SCORE high | 4.7 | 4.8 | 4.2 | 5.1 | 7.2 | 8.3 | ||||
MS, metabolic syndrome.
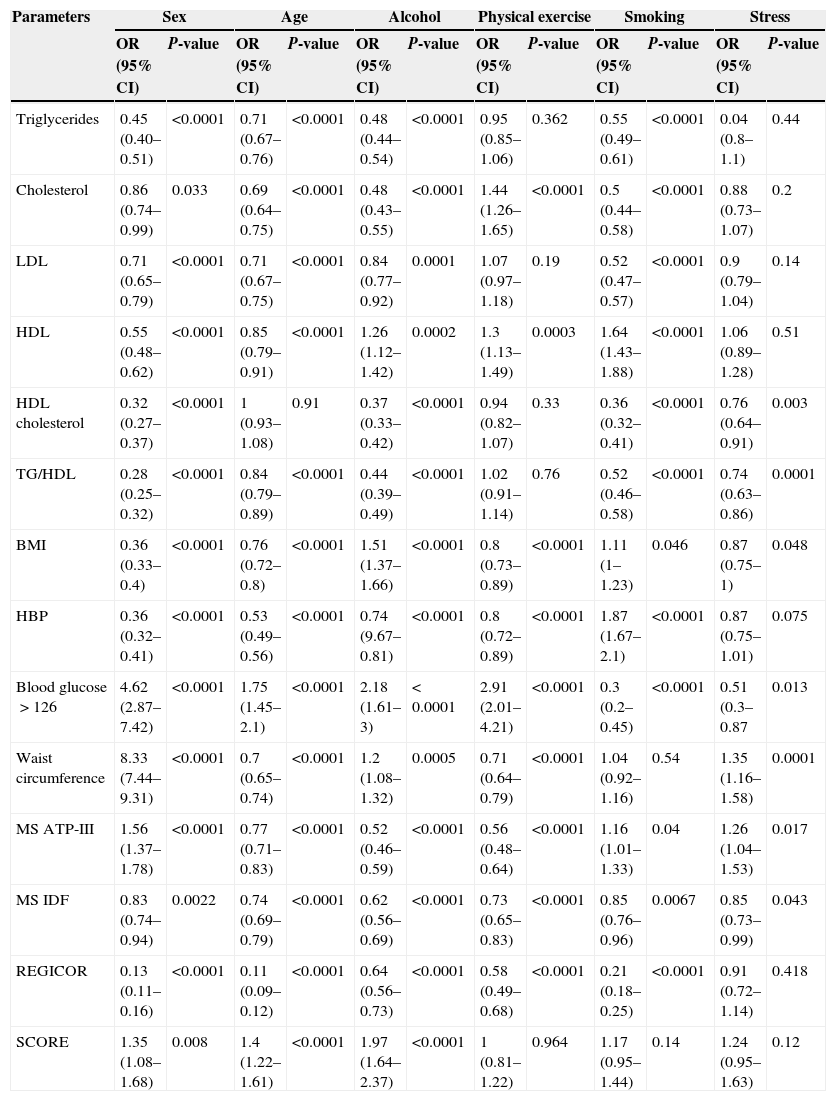
A multivariate analysis was performed, with the parameters related to CVR and MS as variables of interest or response, and sex, age, alcohol consumption, physical exercise, smoking, and stress as explanatory variables.
The purpose of the multivariate analysis was to assess whether one of the explanatory variables influenced, in the presence of the other variables, the response variable. Our study showed that all explanatory variables significantly influenced BMI, blood glucose, and MS. Sex and alcohol consumption were the only explanatory variables with a significant influence on all variables of interest, while physical exercise and stress had less influence. Table 4 shows the complete data, including the odds ratios.
Multivariate analysis of the different variables associated with cardiovascular risk and metabolic syndrome.
| Parameters | Sex | Age | Alcohol | Physical exercise | Smoking | Stress | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | P-value | OR (95% CI) | P-value | OR (95% CI) | P-value | OR (95% CI) | P-value | OR (95% CI) | P-value | OR (95% CI) | P-value | |
| Triglycerides | 0.45 (0.40–0.51) | <0.0001 | 0.71 (0.67–0.76) | <0.0001 | 0.48 (0.44–0.54) | <0.0001 | 0.95 (0.85–1.06) | 0.362 | 0.55 (0.49–0.61) | <0.0001 | 0.04 (0.8–1.1) | 0.44 |
| Cholesterol | 0.86 (0.74–0.99) | 0.033 | 0.69 (0.64–0.75) | <0.0001 | 0.48 (0.43–0.55) | <0.0001 | 1.44 (1.26–1.65) | <0.0001 | 0.5 (0.44–0.58) | <0.0001 | 0.88 (0.73–1.07) | 0.2 |
| LDL | 0.71 (0.65–0.79) | <0.0001 | 0.71 (0.67–0.75) | <0.0001 | 0.84 (0.77–0.92) | 0.0001 | 1.07 (0.97–1.18) | 0.19 | 0.52 (0.47–0.57) | <0.0001 | 0.9 (0.79–1.04) | 0.14 |
| HDL | 0.55 (0.48–0.62) | <0.0001 | 0.85 (0.79–0.91) | <0.0001 | 1.26 (1.12–1.42) | 0.0002 | 1.3 (1.13–1.49) | 0.0003 | 1.64 (1.43–1.88) | <0.0001 | 1.06 (0.89–1.28) | 0.51 |
| HDL cholesterol | 0.32 (0.27–0.37) | <0.0001 | 1 (0.93–1.08) | 0.91 | 0.37 (0.33–0.42) | <0.0001 | 0.94 (0.82–1.07) | 0.33 | 0.36 (0.32–0.41) | <0.0001 | 0.76 (0.64–0.91) | 0.003 |
| TG/HDL | 0.28 (0.25–0.32) | <0.0001 | 0.84 (0.79–0.89) | <0.0001 | 0.44 (0.39–0.49) | <0.0001 | 1.02 (0.91–1.14) | 0.76 | 0.52 (0.46–0.58) | <0.0001 | 0.74 (0.63–0.86) | 0.0001 |
| BMI | 0.36 (0.33–0.4) | <0.0001 | 0.76 (0.72–0.8) | <0.0001 | 1.51 (1.37–1.66) | <0.0001 | 0.8 (0.73–0.89) | <0.0001 | 1.11 (1–1.23) | 0.046 | 0.87 (0.75–1) | 0.048 |
| HBP | 0.36 (0.32–0.41) | <0.0001 | 0.53 (0.49–0.56) | <0.0001 | 0.74 (9.67–0.81) | <0.0001 | 0.8 (0.72–0.89) | <0.0001 | 1.87 (1.67–2.1) | <0.0001 | 0.87 (0.75–1.01) | 0.075 |
| Blood glucose>126 | 4.62 (2.87–7.42) | <0.0001 | 1.75 (1.45–2.1) | <0.0001 | 2.18 (1.61–3) | <0.0001 | 2.91 (2.01–4.21) | <0.0001 | 0.3 (0.2–0.45) | <0.0001 | 0.51 (0.3–0.87 | 0.013 |
| Waist circumference | 8.33 (7.44–9.31) | <0.0001 | 0.7 (0.65–0.74) | <0.0001 | 1.2 (1.08–1.32) | 0.0005 | 0.71 (0.64–0.79) | <0.0001 | 1.04 (0.92–1.16) | 0.54 | 1.35 (1.16–1.58) | 0.0001 |
| MS ATP-III | 1.56 (1.37–1.78) | <0.0001 | 0.77 (0.71–0.83) | <0.0001 | 0.52 (0.46–0.59) | <0.0001 | 0.56 (0.48–0.64) | <0.0001 | 1.16 (1.01–1.33) | 0.04 | 1.26 (1.04–1.53) | 0.017 |
| MS IDF | 0.83 (0.74–0.94) | 0.0022 | 0.74 (0.69–0.79) | <0.0001 | 0.62 (0.56–0.69) | <0.0001 | 0.73 (0.65–0.83) | <0.0001 | 0.85 (0.76–0.96) | 0.0067 | 0.85 (0.73–0.99) | 0.043 |
| REGICOR | 0.13 (0.11–0.16) | <0.0001 | 0.11 (0.09–0.12) | <0.0001 | 0.64 (0.56–0.73) | <0.0001 | 0.58 (0.49–0.68) | <0.0001 | 0.21 (0.18–0.25) | <0.0001 | 0.91 (0.72–1.14) | 0.418 |
| SCORE | 1.35 (1.08–1.68) | 0.008 | 1.4 (1.22–1.61) | <0.0001 | 1.97 (1.64–2.37) | <0.0001 | 1 (0.81–1.22) | 0.964 | 1.17 (0.95–1.44) | 0.14 | 1.24 (0.95–1.63) | 0.12 |
MS, metabolic syndrome.
Concern for the effects of the consumption of alcohol and other drugs in the workplace is a priority for risk prevention and has resulted in prevention campaigns in specific areas which have been reported in the literature. These include the study of González and Salgado (2000) of dockworkers in the port of Barcelona, carried out with the active participation of both workers and employers,14 and the 2002 campaign in the transport sector (RENFE), which included a training program for representatives of unions and middle management to teach them how to recognize the initial signs of danger, and to involve them in identification and monitoring during treatment and the occupational rehabilitation process.15 The main objective in both cases was the prevention of accidents at work caused by alcohol consumption.
But beyond such attempts at accident prevention, alcohol consumption by workers may be addressed from the perspective of health promotion and the implementation of health surveillance actions, as was done in this study. In this case, the variables analyzed in relation to alcohol consumption were those related to CVR and, specifically, MS.
The most recent studies have reopened the debate regarding the benefits of moderate alcohol consumption and the adverse effects of high consumption, with an increasing trend to a greater emphasis being placed on the latter over the former, as shown, for example, by the Taylor study published in 2013.16 This debate had already been addressed in prior studies such as the literature review on this subject conducted by Britton A and McKee M in 2000 in Eastern European countries17 or in Russia in 2002.18
The results obtained in this study in the work environment should be treated with caution, as this was a cross-sectional study that could not provide results as robust as prospective studies, although both types of studies have provided similar results.
The impact of alcohol consumption on CVR factors, and especially on MS, is controversial. In fact, the results of this study do not fully agree with those reported by authors such as Bhanushali et al.19 in the general US population. These authors found no direct relationship between aspects related to quality of life, including alcohol consumption, and an increased risk of MS, although they reported a greater incidence of this syndrome in females and in relation to their marital status. By contrast, studies such as the one by Shin MH et al. report results which agree with those found in this study, with a clearly significant relationship between alcohol consumption levels and the presence of MS in Korean adults, particularly males.20 The results obtained in the Fan AZ study conducted in 2008 more specifically reported a clear relationship between alcohol consumption and an increased risk of an elevation of blood glucose, blood pressure, triglyceride, and obesity levels, all of them related to MS. This study concluded by recommending public health campaigns to prevent alcohol consumption and so reduce the risk of MS.21
Current theories on the impact of alcohol consumption, in terms of both the type of alcohol consumed and the rate of consumption, on MS rates are controversial and appear to suggest that low or moderate consumption may decrease the impact of obesity on the risk of diabetes, especially as regards wine and beer consumption. However, other factors also need to be taken into consideration, such as strict adherence to a Mediterranean diet, which can have a protective effect, allegedly because of its potential pleiotropic effects on health.22
By contrast, in a study of Korean males, other authors suggested a positive association between heavy alcohol consumption and MS, which was stronger among occasional than regular drinkers, and concluded that heavy alcohol consumption, even when indulged in occasionally, was a risk factor for MS. However, the authors considered that further studies were needed to confirm this association.23
Other studies along this same line include the one reported by Sun et al. in 2014. A prospective meta-analysis including 28,862 participants with 3305 cases of MS concluded that heavy drinkers had a greater risk of MS as compared to non-drinkers, while very light drinkers had a lower risk of MS.24
This controversial subject was also addressed in the review conducted by Alkerwi et al. in a meta-analysis of observational studies including a review of 14 relevant publications that identified the relationship between alcohol consumption and MS prevalence. The results of the seven studies finally included in the meta-analysis showed that alcohol consumption lower than 40g/day in males and 20g/day in females significantly decreased the prevalence of MS.
This review suggests that responsible alcohol consumption is associated with a decreased prevalence of MS and supports current recommendations regarding alcohol consumption by apparently healthy people.25
Occupational health, in addition to comprehensive health and disease prevention in workers in its role of health promotion, also addresses aspects related to occupational safety, risk prevention, and the reduction of accident rates. As occupational health is a part of public health, it is a suitable field for the implementation of preventive measures and training and information campaigns on CVR diseases, MS, and lifestyle habits such as alcohol consumption. The European Union considers the workplace, together with family and school, to be one of the mainstays for the management of drug addiction.26 Specific health surveillance check-ups performed by occupational physicians on behalf of companies give physicians ready access to workers. Health examinations provide them with an excellent opportunity to reduce the risks inherent in the tasks performed by workers, to prevent diseases once consumption (excess regular consumption) is detected and to give advice to workers on the risks of such consumption for their health.27,28
Excess alcohol consumption has a negative impact on all CVR parameters, particularly in heavy drinkers. The results are worse with increasing age and in females. In MS, alcohol consumption and being female are the only explanatory variables with a significant influence on all the variables of interest. Taking into account the results obtained, it appears well worth the effort to meticulously assess alcohol consumption in the general and working populations, and to suggest preventive strategies based on such results. Such strategies will be the more effective the earlier they are implemented and if there is a coordinated effort at all the health care levels involved.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Vicente-Herrero MT, López González ÁA, Ramírez-Iñiguez de la Torre MV, Capdevila-García L, Terradillos-García MJ, Aguilar-Jiménez E. Parámetros de riesgo cardiovascular, síndrome metabólico y consumo de alcohol en población laboral. Endocrinol Nutr. 2015;62:161–167.