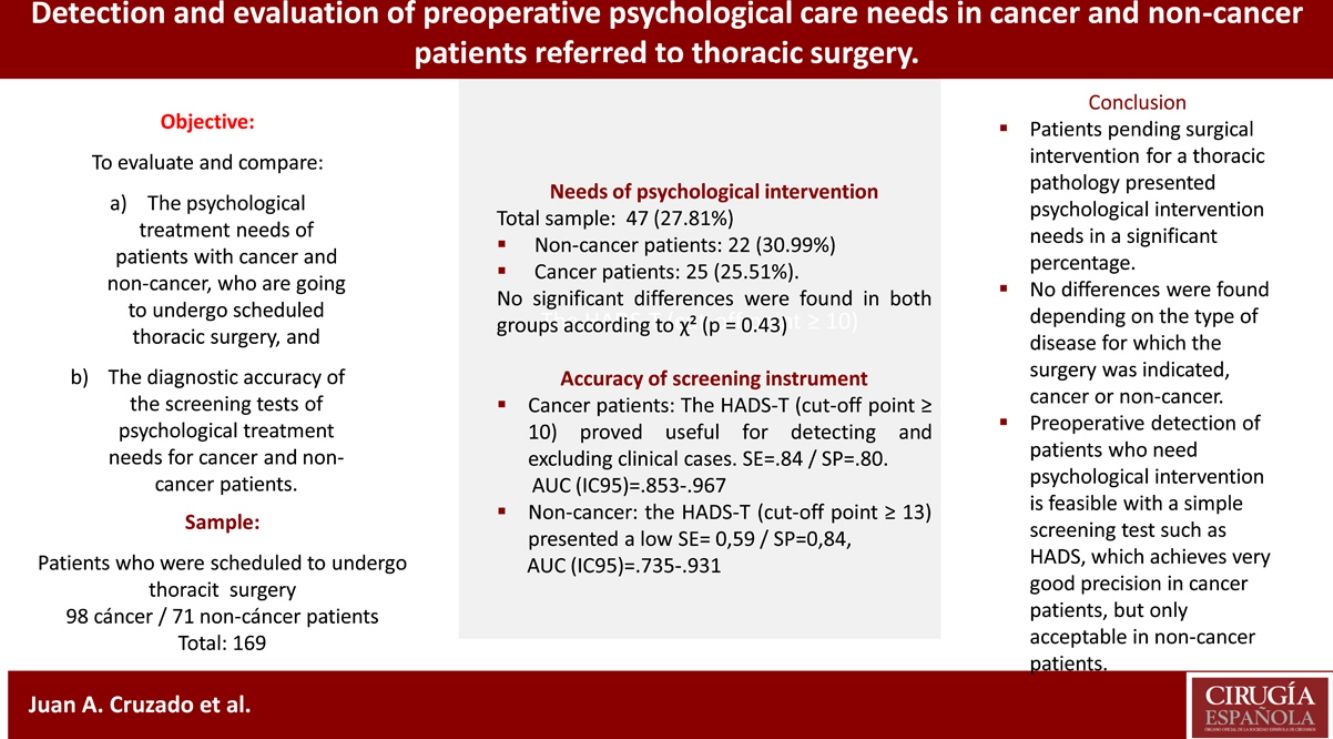
(a) to evaluate and compare the psychological treatment needs of patients with cancer and non-cancer, who are going to undergo scheduled thoracic surgery, and (b) evaluate and compare the diagnostic accuracy of the screening tests of psychological treatment needs for cancer and non-cancer patients.
MethodThe need for psychological treatment was evaluated in a total of 169 patients prior to thoracic surgery, through a clinical interview. The screening tests used were: the physician's judgment (yes/no), the Hospital Anxiety and Depression Scale (HADS) and, the single-item interview to assess depression “Do you feel depressed?” (DEPQ).
ResultsThe number of patients who needed psychological treatment in the total sample was 47 (27.81%), in non-cancer-patients: 22 (30.99%) and in cancer patients: 25 (25.51%). The participants with treatment needs were more often young women with primary education levels, with more fears and concerns regarding their disease. With respect to the screening tests, the HADS-T (cut-off point ≥13) obtained a sensitivity (SE) of 0.75 and Specificity (SP) of 0.81 in the total sample. In patients with cancer, the HADS total score (cut-off point ≥10) obtained an SE=0.84 and SP=0.80, and, in non-cancer patients, the HADS total score (cut-off point ≥13) showed an SE=0.59 and SP=0.84. The DEPQ and the physician's judgment did not achieve adequate levels of precision.
ConclusionsA high percentage of patients have psychological treatment needs before performing thoracic surgery, which are similar for cancer and non-cancer patients. Preoperative detection of patients who need psychological intervention is feasible with a simple screening test: HADS, which achieves greater precision in cancer patients.
Evaluar y comparar: a) las necesidades de tratamiento psicológico de pacientes con cáncer y sin cáncer, que van a someterse a una cirugía torácica programada, y b) la precisión diagnóstica de las pruebas de detección de necesidades psicológicas para pacientes con y sin cáncer.
MétodosSe evaluó la necesidad de tratamiento psicológico en un total de 169 pacientes antes de la cirugía torácica, a través de una entrevista clínica. Las pruebas de cribado fueron: el criterio médico (sí/no), la Escala de Ansiedad y Depresión Hospitalaria (HADS) y la entrevista de un solo ítem de depresión «¿Se siente deprimido?» (DEPQ).
ResultadosEl número de pacientes que necesitaron tratamiento psicológico fue en el total 47 (27,81%), en pacientes sin cáncer: 22 (30,99%) y con cáncer: 25 (25,51%). Las participantes con necesidades de tratamiento eran con mayor frecuencia mujeres jóvenes con niveles de educación primaria y más temores con respecto a su enfermedad. Con respecto a las pruebas de detección, el HADS total (corte ≥ 13) obtuvo una sensibilidad (S)=0,75/especificidad (E)=0,81 en la muestra total. En pacientes con cáncer el HADS total (corte ≥ 10): S=0,84/E=0,80 y en pacientes sin cáncer, la HADS total (corte ≥ 13): S=0,59/E=0,84. DEPQ y juicio médico obtuvieron bajos niveles de precisión.
ConclusionesUn alto porcentaje de pacientes antes de realizar una cirugía torácica tiene necesidades de tratamiento psicológico, similares para pacientes con y sin cáncer. La HADS total es un buen método de cribado de necesidades psicológicas, especialmente en pacientes con cáncer.
Major surgery is associated with high levels of anxiety, depression and emotional distress, which can increase postoperative complications, such as pain, use of analgesics, prolongation of hospital stay,1–4 quality of life,5 and even increasing the risk of mortality.6,7 Preoperative psychological preparation has positive effects on postoperative results, for those most vulnerable patients, which is why the need to implement a preoperative assessment of the psychological state of patients has been pointed out, including symptoms of anxiety, depression and other variables of psychological risk in routine clinical care.8,9
Specifically, it has been proven that, in the moment prior to carrying out a thoracic surgery, one third of the patients present the need of psychological intervention referral.10 However, there is a lack of research on the possible differences in the need for psychological treatment and the levels of anxiety and depression among patients undergoing a thoracic surgical procedure depending on the nature of the disease that forces such surgery, whether it is oncological or not. It has been reported that patients with lung cancer have a high incidence of anxiety and depression symptoms.11,12 Likewise, it has been reported that hospitalized non-cancer patients frequently show a high level of emotional distress, although to a lesser extent than cancer patients.13 However, the available data are insufficient, and do not refer specifically to thoracic surgery services.
A comprehensive health care with optimal quality requires identifying those patients who have high levels of emotional distress and are therefore in need of a psychological approach in earlier stages of their process. Likewise, it is important to check whether the levels of anxiety, depression and psychological treatment needs of patients with lung cancer differ in incidence, severity or characteristics to those presented by those patients with a non-neoplastic process. In addition, it is necessary to verify whether an early, accurate and effective detection can be carried out by means of a brief and simple screening test applied by the thoracic surgery services.
The request for referral to mental health services is often carried out at the initiative of the patients themselves and their families, or by the referral of the healthcare professionals involved in the patients’ process. This is not effective, as often the demands of those affected do not correspond to the severity of emotional distress, and doctors often underestimate the needs of patients in this regard.10,14 A screening method for emotional distress should be implemented because it has greater potential as a method of referral of the psychological care that the patient demands or medical referral.15 Among the most used tests are the Hospital Anxiety Depression Scale (HADS),16 or the Single-item interview, which can detect the presence and, where appropriate, the severity of depressive elements through the simple question: Are you depressed? (DEPQ).17 As criteria to assess the diagnostic perception of these tests, standardized clinical diagnostic interviews have been used. The inconveniences of such interviews are that they require a relatively long application time and are ultimately expensive. In addition, they may be unattractive to patients, and focus on identifying well-defined psychopathological conditions. A feasible alternative is to conduct a clinical interview that assesses the patients’ level of emotional distress, explores the clinical symptoms of anxiety and depression, fears and concerns, the perceived social support and the coping strategies that patients use to face their disease.10,18
The objectives of the present study are: (a) to evaluate and compare the psychological needs of patients with cancer and non-cancer, who are going to undergo scheduled thoracic surgery, and the symptoms of anxiety and depression among patients according to the type of pathology and, (b) evaluate and compare the diagnostic accuracy of the screening tests of the most appropriate psychological treatment needs for cancer and non-cancer patients.
The following hypotheses were formulated: (a) the frequency of cancer and non-cancer patients with psychological intervention needs is the same, and (b) the diagnostic precision of each of the screening tests for the need for psychological treatment will be satisfactory, for cancer and non-cancer patients.
MethodSamplePatients who were scheduled to undergo surgical intervention in a Department of Thoracic Surgery at a public hospital were included in the study prospectively. The inclusion criteria were: being over 18 years of age, having good comprehension and expression in Spanish, and having adequate levels of cognitive function (Mini-Mental score>26).19 Patients who – according to their medical and/or psychiatric diagnosis – had severe cognitive impairment or a severe psychiatric disorder were excluded from the sample. The study was conducted throughout a period of 18 months, the number of initial patients was 199, of which 16 declined taking part in the study, and 14 did not meet the inclusion/exclusion criteria, thus, the total sample was 169 patients.
Variables and instrumentsScreening tests were chosen for their simplicity, brevity in their application, adequate psychometric properties, and having been used in previous studies:
Hospital Anxiety and Depression Scale (HADS).16,20 It is a self-applied instrument, composed of 14 items. It evaluates the presence of symptoms of anxiety and depression during the past week. High scores in its subscales – anxiety (HADS-A) and depression (HADS-D), of 7 items each – indicate a high frequency of these symptoms. The total scale score (HADS-T) provides a valid measure of emotional distress. HADS has been shown to have good sensitivity and specificity.21–23
The Single-item interview, which measures depressed mood through the question: “are you depressed?” (DEPQ) was developed by Chochinov et al.17 This question has a dichotomous response (Yes/No) and is complemented by 5 Likert-type response options.17 This can be a highly recommended measure due to the brevity of its application. Chochinov et al. reported values of sensitivity (SE) and specificity (SP) of 100%. The meta-analysis performed by Mitchell concluded that the SE of this test is 0.72 and SP is 0.83.24
Medical judgment is issued by the physician after a medical consultation with the patient. Each physician completes a form in which he/she issues a judgment on whether the patient needs psychological attention.
The need for psychological intervention was assessed through a psychological interview similar to that carried out by Bonachi et al.18 These interviews were carried out by a psychologist, with a duration of one hour. At the end of the interview, the psychologist assessed whether the patient needed psychological treatment, as indicated by at least one of the following variables assessed by the interview: The presence and intensity of anxious-depressive symptoms, as well as fears and concerns about their medical condition or other areas; the current or past presence of mental health disorders and the consumption of psychoactive drugs; perceived family and/or social support; coping strategies toward their medical condition and resilience; and other personal and family problems. This interview was the criterion variable to verify the diagnostic accuracy of the screening tests.
The psychologist's rating of the case with psychological needs may be for any symptom or problem that the patient reveals in the interview that were indicative of poor adaptation to the surgical process or the disease. Each interview was recorded, and subsequently heard by another psychologist who independently evaluated whether the patient needed psychological treatment or not without knowing the first interviewer's judgment. In the case of disagreement among psychologists, the case was examined by a third psychologist who made the final decision.
ProcedureEthical approval for this study was obtained from clinical research Ethics Committee of the Hospital Clínico San Carlos (n° 16/109). All patients were informed of the study by one of the surgeons in the service at the time of surgical indication. Next, a psychologist gave each patient an explanatory sheet of the research project and explained it verbally, and answered the questions, if he agreed to participate, he signed the informed consent document. After that, the psychologist then administered the HADS and DEPQ tests. The surgeon who had assessed the patient established his/her professional judgment about the need for psychological intervention based on the medical interview. Next, the clinical interview was carried out, carried out by another psychologist, to verify the results of the tests and the physician's judgment. After this specialized interview, the need for psychological treatment for each case was assessed.
Statistical analysesDescriptive, sociodemographic and clinical data were collected from patients with oncological and non-oncological processes, and the entire sample, as well as for patients who, after the clinical interview, were considered to need preoperative psychological intervention and those who were not. The possible differences between both groups were verified by chi-square tests in the case of categorical and mean variables and through the Student's t test for interval or continuous variables. The Cohen Kappa coefficient was calculated to verify the concordance among the interviewers.
The significance of the mean differences between the oncological and non-oncological patients for the HADS and DEPQ scales was checked. As both samples were found to be different in terms of sex and age, a covariance analysis was applied to control the effect of these variables.
To assess the diagnostic accuracy of the screening tests with respect to the interview (gold standard), the Sensitivity (SE) and Specificity (SP) indices, the Positive Predictive Values (PPV) and the Negative Predictive Value (NPV) and the indexes recommended by Mitchell were calculated.24 Mitchell's recommended indexes were: The Clinical Positive Utility Index, (CUI+)=SE×PPV, which shows the usefulness of the test in detecting problem cases, and the Clinical Negative Utility Index (CUI−), used to determine the usefulness of the instrument when discarding the cases considered as non-clinical: (CUI−)=SP×NPV. In addition, the Overall Value Index for the (CUI+) and (CUI) for each test was extracted. This is a single measure that determines the validity of each screening test. The qualitative value ranges for these indices are as follows: excellent: ≥0.81; good: 0.64–0.80; fair: 0.49–0.63; poor: 0.37–0.48; very poor <0.37 (see: http://www.psychooncology.info/cui.html). Those cut-off points that showed better levels of SE and SP were selected for each of the screening tests.
In addition, the diagnostic accuracy of each test was assessed using the receiver operating characteristic (ROC).
ResultsThe sociodemographic and clinical data of the final sample of patients are presented in Table 1.
Sociodemographic and clinical data for cancer and non-cancer patient groups.
| Cancer | Non-cancer | Total | p (cancer vs. non-cancer) | |
|---|---|---|---|---|
| (N=98) | (N=98) | (N=169) | ||
| Mean age (SD) | 67.9 (15.8) | 53.9 (8.3) | 62.04 (13.92) | <0.001 |
| Sex n (%)Female/male | 42 (42.9)/56 (57.1) | 43 (60.6)/28 (39.4) | 85 (50.3)/84 (49.7) | 0.023 |
| Marital status n (%) | ||||
| Married | 67 (68.4) | 52 (73.2) | 119 (70.4) | 0.074 |
| Widow/widowed | 15 (13.9) | 4 (6.6) | 19 (11.2) | |
| Divorced | 9 (8.3) | 4 (6.6) | 13 (7.7) | |
| Single | 7 (7.1) | 11 (15.5) | 18 (10.7) | |
| Education n (%) | ||||
| Primary | 39 (39.8) | 27 (38.0) | 66 (39.1) | 0.095 |
| Secondary | 28 (28.6) | 20 (28.2) | 48 (28.4) | |
| Higher education | 31 (31.6) | 24 (33.8) | 55 (32.5) | |
| Diagnosis n (%) | ||||
| Adenocarcinoma | 50 (51.0) | 50 (29.6) | 0.001 | |
| Squamous cell carcinoma | 22 (22.4) | 22 (13.0) | ||
| Metastasis | 14 (14.3) | 14 (8.3) | ||
| Other tumors | 12 (12.3) | 12 (7.1) | ||
| Benign/no neoplasm | 71 (100.0) | 71 (42.0) | ||
| Surgical treatment n (%) | ||||
| Lobectomy | 41 (41.8) | 6 (8.45) | 47 (27.81) | <0.001 |
| Timectomy | – | 5 (7.04) | 5 (2.96) | |
| Pleurodesis | 2 (1.9) | 5 (7.04) | 7 (4.14) | |
| Pleurectomy | 2 (1.9) | 10 (14.08) | 12 (7.10) | |
| Atypical segmentectomy | 28 (28.6) | 18 (25.35) | 46 (27.22) | |
| Typical segmentectomy | 19 (19.4) | 8 (11.27) | 27 (15.98) | |
| Mediastinal Resection | 8 (1.0) | 11 (15.49) | 11 (6.51) | |
| Other | 5 (5.1) | 8 (11.27) | 14 (8.28) | |
| Type of surgery n (%) | ||||
| VATS | 27 (27.6) | 36 (50.7) | 63 (37.3) | 0.02 |
| Thoracotomy | 71 (72.4) | 35 (49.3) | 106 (62.7) | |
The Cohen's Kappa coefficient used to verify the concordance among the interviewers was 0.89 (excellent).
After the clinical interview, 47 patients (27.81%) were considered in need of psychological intervention. In the sample of patients without an oncological process, the number was 22 (30.99%), and in the sample of patients with an oncological process, it was 25 (25.51%). No significant differences were found in the χ2 test (p=0.43).
Patients with treatment needs (cases) were more frequently women (78.7%) than men (p<0.001). The mean age of the clinical cases was 83.90 (SD=8.64) compared to that of non-clinical cases (67.94, SD=15.54) (p=0.011). The level of studies was lower in clinical cases, as 51.11% of them only had primary studies (p=0.47).
Table 2 shows the means and standard deviations for each of the screening tests for both cancer and non-cancer patients, and the total sample. As can be observed in Table 1, the sample of patients without cancer had a higher percentage of women (p<0.001) and had a lower mean age (p<0.001) than the sample of cancer patients. The means of HADS-A and HADS-T were higher for non-cancer patients, but once the ANCOVA controlled for differences in sex and age, there were no significant differences between the two groups. It is interesting to note that 80.30% of patients without cancer responded positively to the question of whether they felt fear and intense concerns about their disease, while in the group of cancer patients the result was 62.30% (p=0.03).
Symptoms of anxiety, depression and emotional distress measured by the HADS, and DEPQ for cancer and non-cancer patients. The result of the covariance analysis is presented to verify the differences between both groups after controlling for the variables sex and age.
| Cancer | Non-cancer | p | Total | |
|---|---|---|---|---|
| (N=98) | (N=71) | (N=169) | ||
| Mean/(SD) | Mean/(SD) | Mean/(SD) | ||
| HADS-A | 5.60 (3.63) | 7.17 (4.28) | p=0.175 | 6.26 (3.98) |
| HADS-D | 3.92 (3.14) | 4.60 (4.19) | p=0.53 | 4.21 (3.63) |
| HADS-T | 9.51 (5.99) | 11.77 (7.75) | p=0.20 | 10.46 (6.85) |
| DEPQ | 1.56 (0.72) | 1.69 (0.87) | p=0.711 | 1.62 (0.61) |
HADS: Hospital Anxiety and Depression Scale; HADS-A: anxiety subscale of the Hospital Anxiety and Depression Scale; HADS-D: depression subscale of the Hospital Anxiety and Depression Scale; HADS-T: total score of the Hospital Anxiety and Depression Scale; DEPQ: Depression Question.
The results of the diagnostic accuracy of each screening instrument for emotional distress for patients with cancer and without cancer, as well as for the total sample, are shown in Table 3. It can be observed that the physician's judgment had a very low SE (0.30) but a high SP (0.86), both in the total sample and in the cohorts with and without cancer pathology.
Diagnostic accuracy of the screening tests.
| Test cut-off | SE (CI 95%) | SP (CI 95%) | PPV (CI 95%) | NPV (CI 95%) | CUI+ | CUI− | O. Value |
|---|---|---|---|---|---|---|---|
| Cancer patients | |||||||
| Medical referral Yes/not | 0.32 (0.10–0.50) | 0.84 (0.75–0.92) | 0.40 (0.19–0.62) | 0.78 (0.69–0.87) | 0.13 | 0.65 | 0.70 |
| HADS-A≥7 | 0.76 (0.59–0.93) | 0.78 (0.69–0.88) | 0.54 (0.38–0.71) | 0.91 (0.83–0.98) | 0.41 | 0.71 | 0.78 |
| HADS-D≥5 | 0.64 (0.45–0.83) | 0.88 (0.80–0.95) | 0.64 (0.45–0.83) | 0.88 (0.80–0.95) | 0.41 | 0.77 | 0.82 |
| HADS-T≥10 | 0.84 (0.70–0.98) | 0.80 (0.70–0.89) | 0.58 (0.42–0.74) | 0.94 (0.87–0.1) | 0.49 | 0.74 | 0.81 |
| DEPQ>1 | 0.80 (0.68–0.98) | 0.71 (0.52–0.72) | 0.49 (0.25–0.52) | 0.91 (0.86–0.1) | 0.39 | 0.65 | 0.74 |
| Non-cancer patients | |||||||
| Medical referral Yes/no | 0.26 (0.08–0.44) | 0.92 (0.84–0.98) | 0.60 (0.30–0.90) | 0.72 (0.61–0.83) | 0.16 | 0.66 | 0.70 |
| HADS-A≥7 | 0.64 (0.44–0.84) | 0.84 (0.73–1) | 0.64 (0.44–0.84) | 0.84 (0.72–0.94) | 0.41 | 0.70 | 0.78 |
| HADS-D≥4 | 0.55 (0.34–0.75) | 0.80 (0.68–0.91) | 0.55 (0.34–0.75) | 0.80 (0.68–0.91) | 0.30 | 0.63 | 0.72 |
| HADS-T≥13 | 0.59 (0.41–0.85) | 0.84 (0.68–0.91) | 0.62 (0.41–0.79) | 0.82 (0.72–0.94) | 0.37 | 0.69 | 0.76 |
| DEPQ>1 | 0.78 (0.61–0.95) | 0.68 (0.53–0.80) | 0.53 (0.36–0.70) | 0.87 (0.76–0.98) | 0.41 | 0.58 | 0.70 |
| Total | |||||||
| Medical referral Yes/no | 0.30 (0.18–0.43) | 0.86 (0.80–0.92) | 0.45 (0.28–0.63 | 0.76 (0.69–0.83) | 00.13 | 0.66 | 70 |
| HADS-A≥7 | 0.79 (0.67–0.90) | 0.71 (0.62–0.79) | 0.51 (0.39–0.62) | 0.90 (0.84–0.96) | 0.40 | 0.63 | 0.73 |
| HADS-D≥5 | 0.72 (0.60–0.85) | 0.75 (0.67–0.82) | 0.52 (0.40–0.65) | 0.88 (0.81–0.94) | 0.39 | 0.65 | 0.74 |
| HADS-T≥13 | 0.75 (0.62–0.87) | 0.84 (0.77–0.90) | 0.64 (0.60–0.76) | 0.90 (0.84–0.95) | 0.47 | 0.76 | 0.81 |
| DEPQ>1 | 0.81 (0.70–0.92) | 0.69 (0.61–0.77) | 0.50 (0.39–0.61) | 0.90 (0.84–0.96) | 0.40 | 0.62 | 72 |
In the total sample, the HADS-T (cut-off point ≥13), presented an adequate SE (0.75) and a good SP (0.81), the PPV was modest, but the PPN was high, so we can consider that it is an adequate screening test. The results for HADS-A (cut-off point ≥7) and HADS-D (cut-off point ≥5) presented modest levels, which were sufficient to consider them as acceptable screening tests.
In the sample of cancer patients, the accuracy of HADS was better than in the total sample. The HADS-T (cut-off point ≥10) proved useful for detecting and excluding clinical cases. Whereas the HADS-A (cut-off point ≥7) and HADS-D (cut-off point ≥5) only reached acceptable levels.
In the sample of patients with non-oncological pathologies, the HADS-T (cut-off point ≥13) presented a low SE, although the SP was correct. The diagnostic accuracy was lower than in the sample of cancer patients, although HADS-A (cut-off point ≥7) and HADS-T (cut-off point ≥13) reached an acceptable level.
The DEPQ achieved acceptable levels of SE but the SP was low for the total sample, and for the differentiated cohorts with and without cancer pathology. Therefore, we cannot consider it a good screening test.
The results of the AUC for the screening tests are shown in Table 4. The HADS-T reached a good AUC, higher than 0.8, as did the HADS-A and HADS-D in the total sample. In the case of cancer patients, the results were more satisfactory than in the total sample, achieving an excellent level for HADS-T, and good levels for HADS-A and HADS-D. In the sample of non-cancer patients, HADS-T and HADS-A reached good levels, while HADS-D was only acceptable. The DEPQ did not reach good levels in the total sample, nor in the subsamples, and was lower than the HADS indices.
Area under the curve for each of the screening tests and their statistical significance.
| Cancer | Non-cancer | Total | ||
|---|---|---|---|---|
| HADS-D | AUC | 0.855* | 0.790* | 0.823* |
| IC95 −/+ | 0.777–0.932 | 0.677–0.903 | 0.756–0.890 | |
| HADS-A | AUC | 0.871* | 0.824* | 0.849* |
| IC95 −/+ | 0.789–0.952 | 0.725–0.923 | 0.787–0.911 | |
| HADS-T | AUC | 0.911* | 0.833* | 0.877* |
| IC95 −/+ | 0.853–0.967 | 0.735–0.931 | 0.825–0.930 | |
| DEPQ | AUC | 0.782* | 0.781* | 0.782* |
| IC95 −/+ | 0.672–0.891 | 0.660–0.901 | 0.701–0.863 |
HADS-A: Anxiety subscale of the Hospital Anxiety and Depression Scale; HADS-D: Depression subscale of the Hospital Anxiety and Depression Scale; HADS-T: total score of the Hospital Anxiety and Depression Scale.; ANXQ: Anxiety Question; DEPQ: Depression Question.
Fig. 1 shows the graphic representation of the results of the diagnostic precision of the HADS-T, for the total sample, cancer and non-cancer patients.
DiscussionThe patients who were to undergo a thoracic surgical intervention presented psychological treatment needs in a significant percentage (27.81%), as well as high scores in symptoms of anxiety (HADS-A) and emotional distress (HADS-T). These results are similar to those reported in a previous study on the psychological needs in patients pending thoracic surgery.10 Similar results have been found in patients with oncological processes who must undergo radiotherapy treatment.21,25
As has been reported in other research, women and younger people score higher on HADS-A and HADS-T.25-27 In the present study, the sample of patients without cancer consisted of a greater number of women, with a lower mean age than the samples of patients with cancer. The highest scores in HADS-A and HADS-T in the group of patients without cancer are not statistically different from those in cancer patients once the sex and age differences between the samples are controlled for. Moreover, there are no significant differences in the frequency of people with psychological needs between patients with cancer and without cancer.
The results of the present study showed how cancer patients reported fears and concerns about their disease less frequently than non-cancer patients. In the case of patients with non-operable lung or other cancer, higher levels of emotional distress have been reported than those reported here and could be higher than those with other non-cancerous diseases.11,25,28 In this sense, Deshields et al. reported that there were higher levels of psychological distress in cancer patients compared to other medical conditions.13 Therefore, more research is needed on differences and similarities in terms of psychological needs between cancer and non-cancer patients. However, in the present study, the results obtained state that patients who are going to undergo thoracic surgery have psychological treatment needs, whether they are patients with cancer or with other pathologies.
In relation to screening procedures, the data shows that the physician's judgment underestimates the number of patients with psychological intervention needs, as it only identifies those with very intense symptoms, with a very poor SE. However, the physician's judgment does detect cases that do not need psychological treatment with good precision.
The HADS-T (cut-off point ≥13) proves to be a good screening test for the total sample, and even better in the case of cancer patients (cut-off point ≤10), but only reaches an acceptable level for the subsample without cancer (cut-off point ≥13). The HADS-A and HADS-D reach good or acceptable levels, in the total sample and in that of cancer patients, but HADS-D is deficient as a screening test in patients without cancer. The data from the AUCs confirm that HADS-T is the best screening test, which becomes excellent in the case of cancer patients, HADS-A shows good results for the total sample and the two subsamples, while HADS-D is deficient in the case of patients without cancer.
These results reproduce the data from a previous study by Cruzado et al.10 In the case of cancer patients, the data are similar to those reported by Schellekens et al. with patients with lung cancer (HADS-T cut-off point ≥15) for emotional disorders diagnosed by the Structured Clinical Interview for DSM-IV,29 Cruzado and Hernández in patients undergoing radiotherapy (HADS-T cut-off point ≥10) using the MINI Neuropsychiatric Interview as a criterion,25 or Vodermaier and Millman's review data that report that the best cut-off points for HADS-T were 10 or 11 (SE=0.80; SP=0.74).23
In the case of the DEPQ, it did not prove to be a good screening measure, as the SE is acceptable, but the SP is insufficient, and the AUC is only acceptable. These results are similar to those reported in Cruzado et al.10 but much lower than those found in patients with advanced or palliative cancer.30
As a limitation of this study, it should be noted that the sample is relatively small, especially in the case of the sample of patients without cancer, which is only 71 cases, so the lower accuracy of the diagnostic tests may be due to this fact.
ConclusionsPatients pending surgical intervention for a thoracic pathology with cancer and non-cancer presented psychological intervention needs in a significant percentage. No differences were found depending on the type of disease for which the surgery was indicated, cancer or non-cancer. Preoperative detection of patients who need psychological intervention is feasible with a simple screening test such as HADS-T, which achieves greater precision in cancer patients.
Conflict of interestNone declared.