Current literature supports the claim that performing a cephalic pancreaticoduodenectomy (CPD) as treatment for pancreatic cancer (PC) is associated with an increase in median survival, both in octogenarian (≥80 years) patients as well as younger patients.
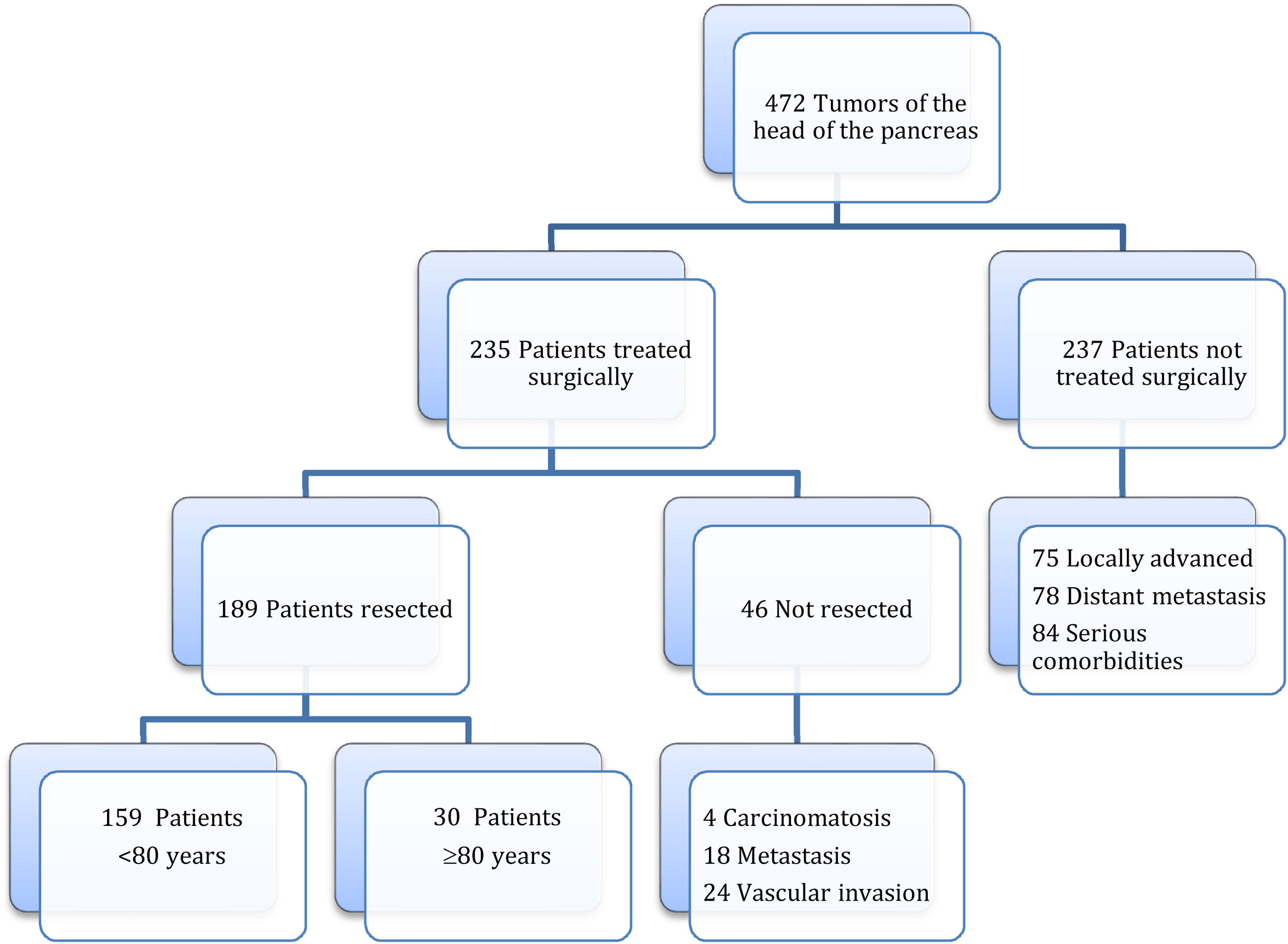
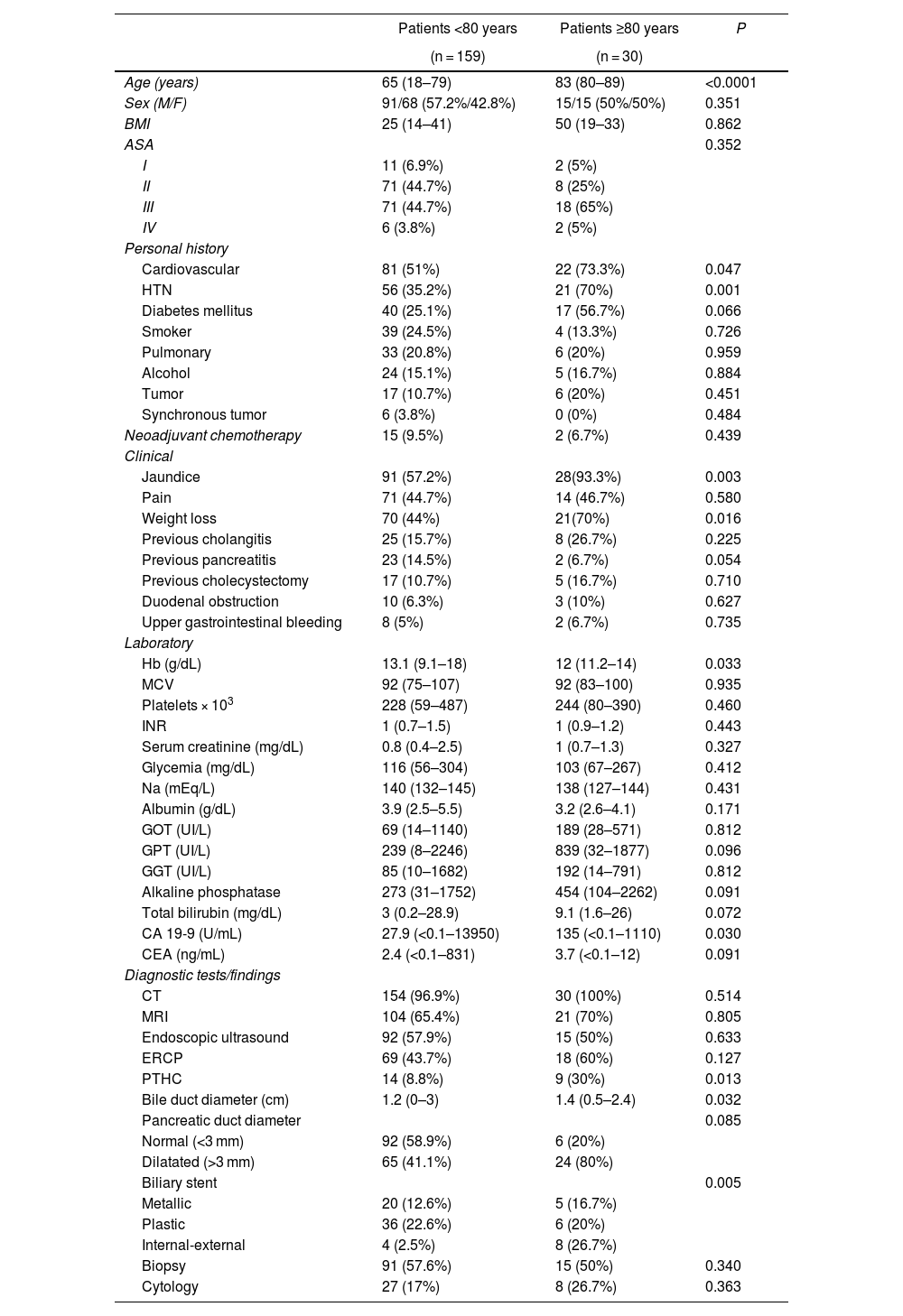
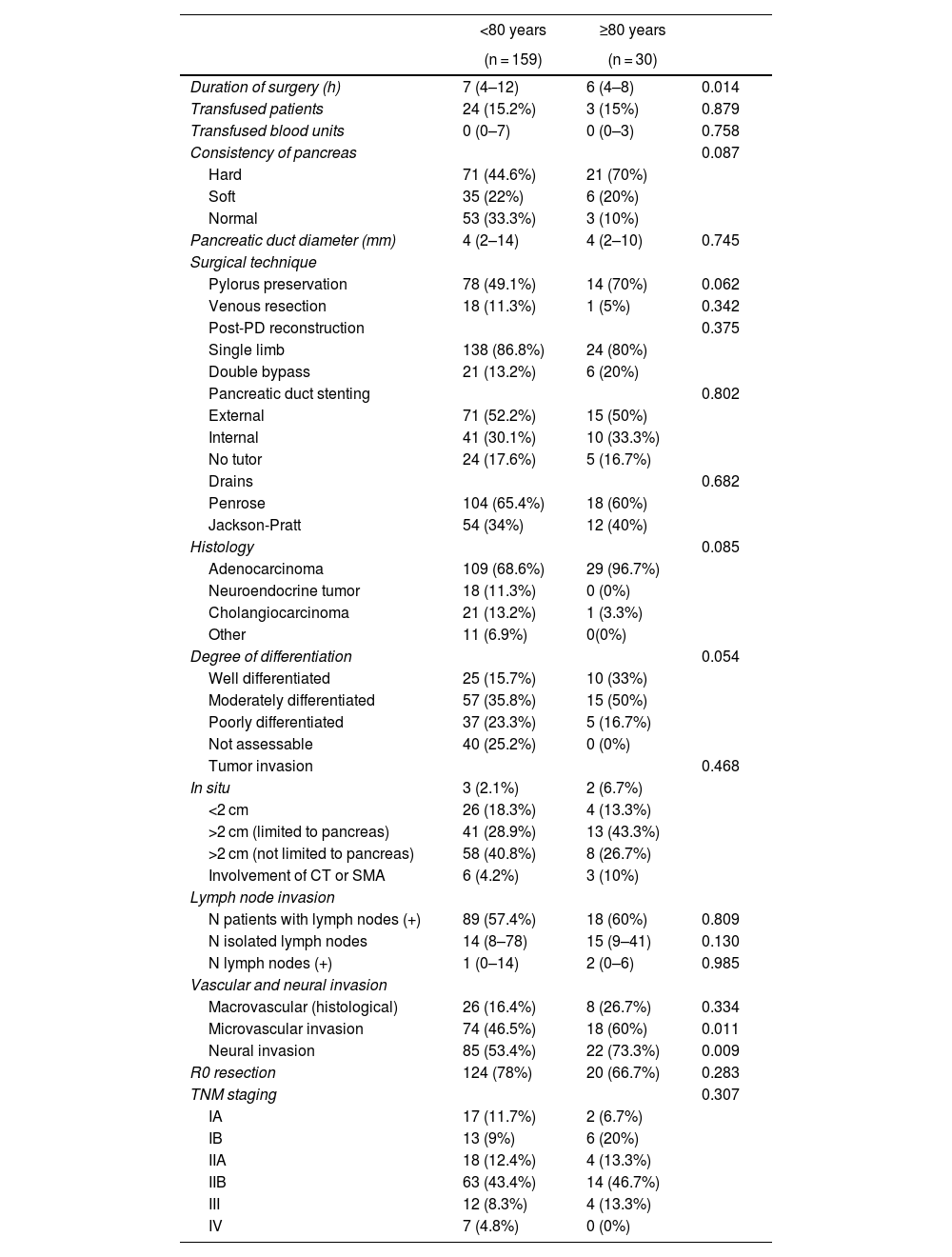
MethodsThis is a retrospective and comparative trial, comparing results for CPD performed on 30 patients ≥80 years with PC and 159 patients <80 years.
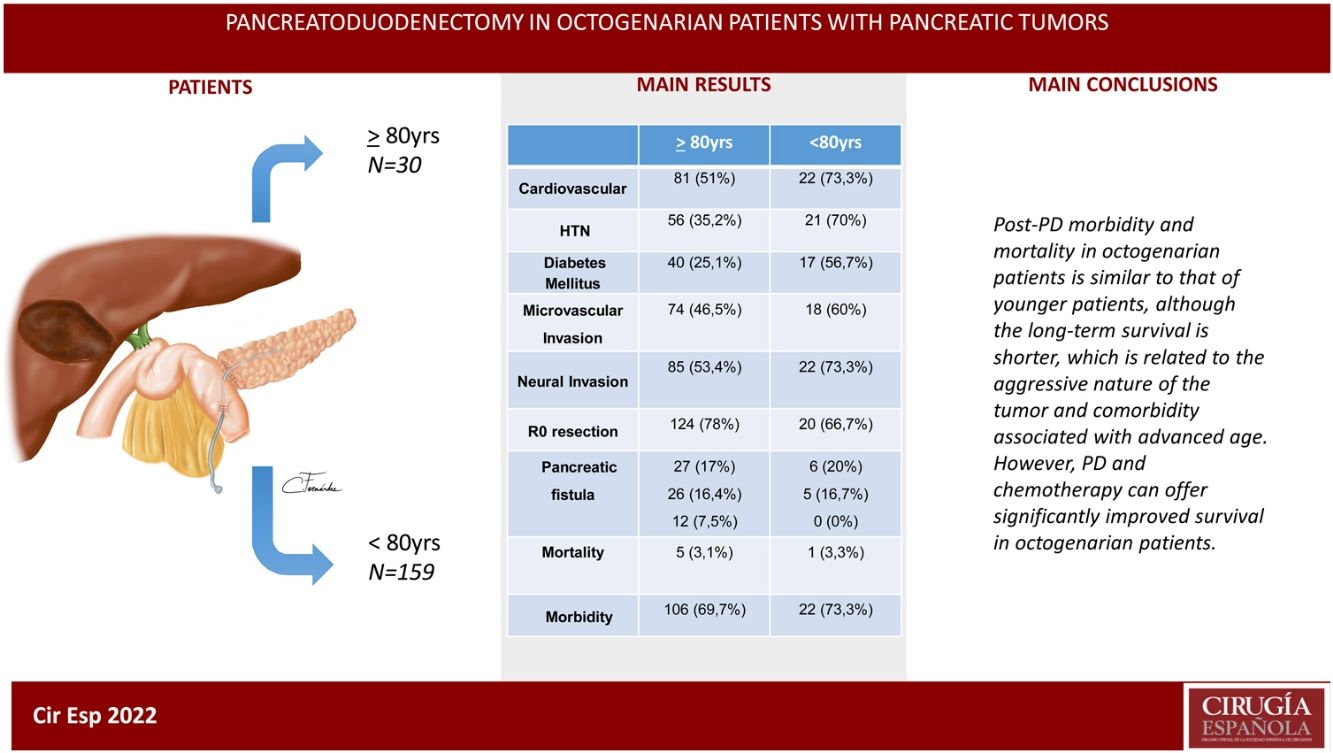
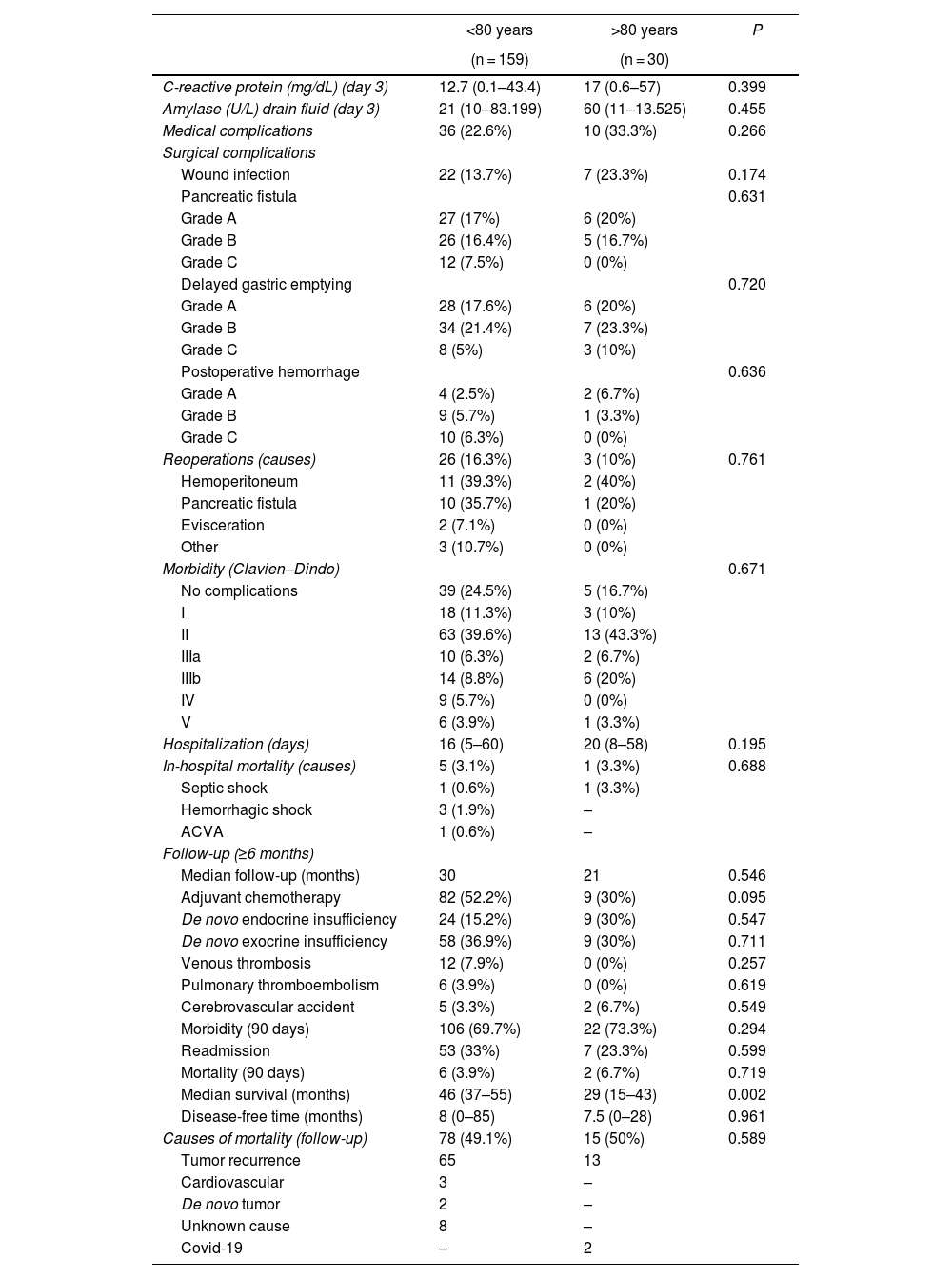
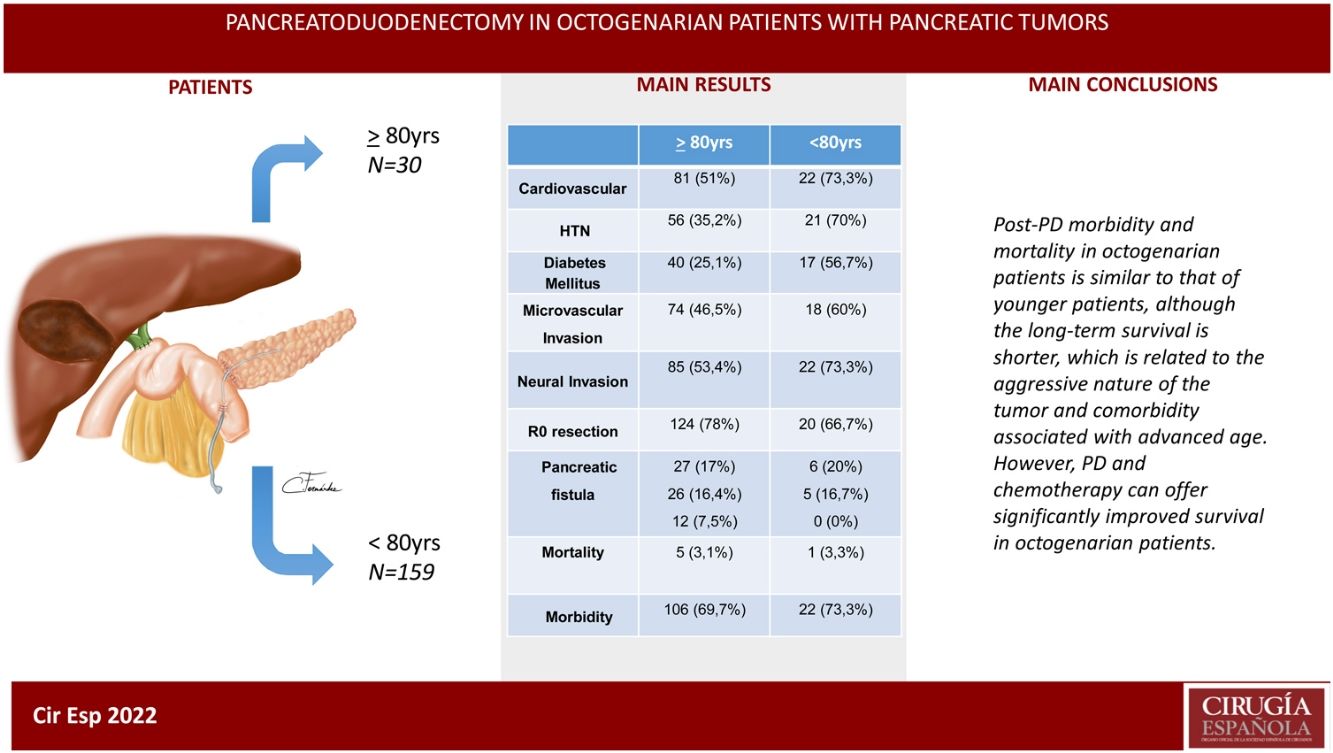
ResultsThe patients in the octogenarian group showed a significantly higher rate of preoperative cardiovascular morbidity and a more aggressive tumoral behaviour, including more significant preoperative anemia, jaundice and levels of CA 19-9, higher vascular and neural invasion, and a lower rate of R0 resection despite using the same surgical technique. There were no significant differences in terms of postoperative complications. Postoperative mortality was similar in both groups (3.3% in octogenarians vs 3.1% in patients <80 years). Mortality during follow-up was mainly due to tumour recurrence, cardiovascular complications and COVID-19 in 2 elderly patients.
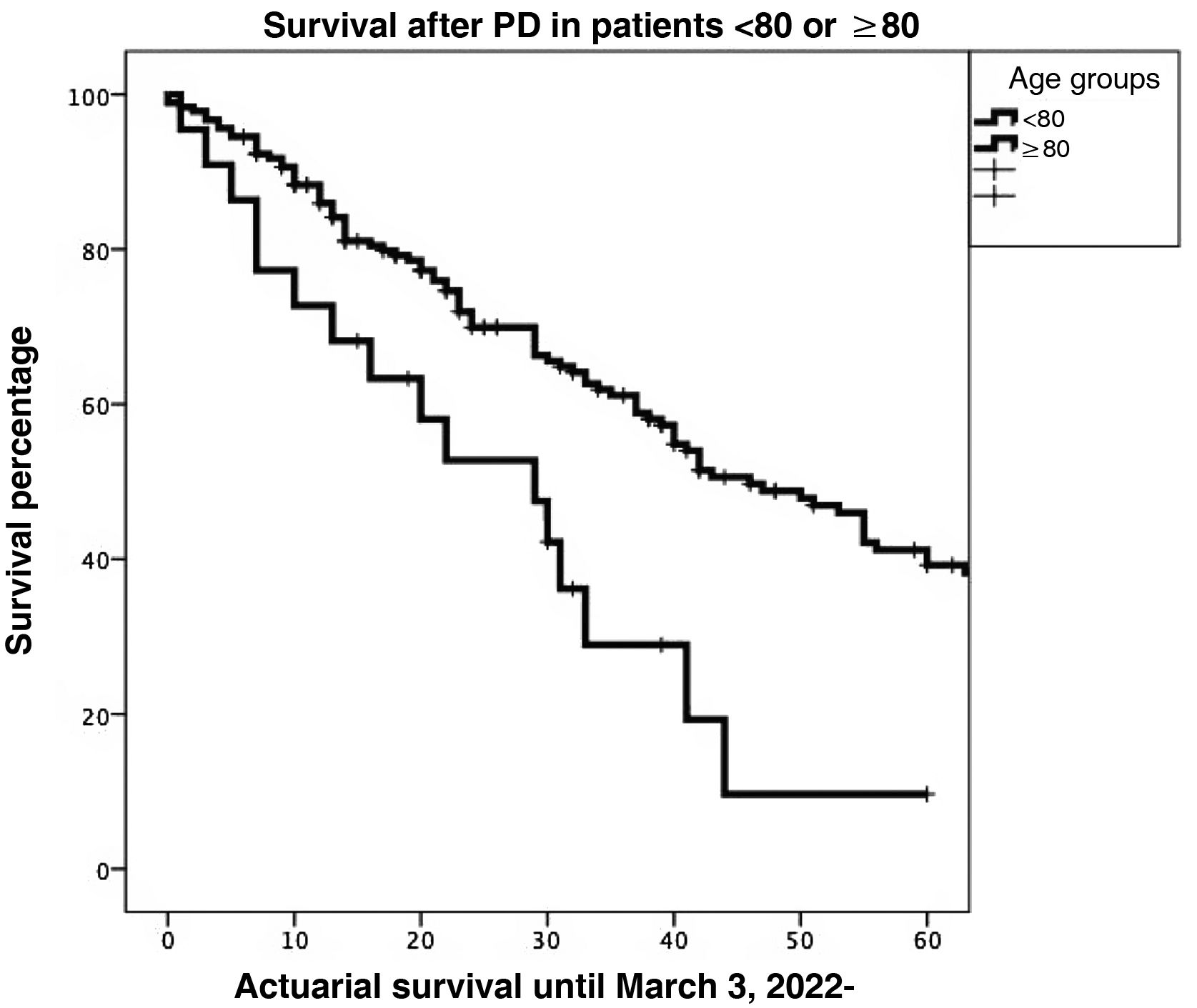
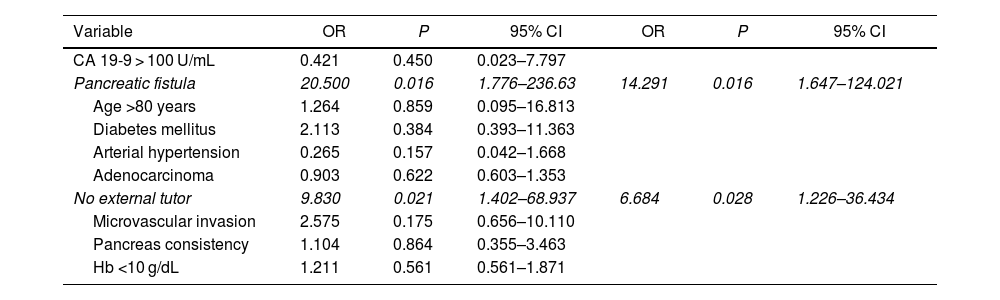
Actuarial survival at 1, 3 and 5 years was significantly larger for patients <80 years old, as compared to octogenarians (85.9%, 61.1% and 39.2% versus 72.7%, 28.9% and 9.6%, respectively; P = 0.001). The presence of a pancreatic fistula and not using external Wirsung stenting were significantly associated with 90-day postoperative mortality after a CPD.
ConclusionsMorbidity and mortality post-CPD is similar in octogenarians and patients younger than 80, although long-term survival is shorter due to more aggressive tumours and comorbidities associated with older age.
Según estudios previos, la duodenopancreatectomía cefálica (DPC) por cáncer de páncreas (CP) se asocia a un incremento de la supervivencia mediana tanto en pacientes octogenarios como en pacientes de menor edad.
MétodosEstudio retrospectivo y comparativo de la DPC realizada en 30 pacientes ≥ 80 con CP y en 159 pacientes < 80 años.
ResultadosLos pacientes octogenarios presentaban una tasa significativamente mayor de morbilidad cardiovascular preoperatoria y un comportamiento tumoral más agresivo (mayor anemia, ictericia y CA 19-9 preoperatorios, invasión vascular y neural y menor frecuencia de resección R0 a pesar de utilizar la misma técnica quirúrgica). No hubo diferencias significativas en cuanto a complicaciones postoperatorias. La mortalidad postoperatoria fue similar en ambos grupos (3,3% en octogenarios versus 3,1% en < 80 años). Las causas de mortalidad durante el seguimiento fueron fundamentalmente por recidiva tumoral, complicaciones cardiovasculares y COVID-19 (2 octogenarios).
La supervivencia actuarial a 1, 3 y 5 años fue significativamente mayor en pacientes < 80 años que en octogenarios (el 85,9%, el 61,1 y el 39,2% versus el 72,7, el 28,9 y el 9,6%, respectivamente; p = 0,001). En el estudio multivariable, la presencia de una fístula pancreática y la no utilización de tutor externo del Wirsung influyeron de forma estadísticamente significativa sobre la mortalidad a 90 días post-DPC.
ConclusionesLa morbimortalidad post-DPC es similar en octogenarios y < 80 años, aunque la supervivencia a largo plazo es menor por la agresividad tumoral y comorbilidad asociada a la edad avanzada.