Digital evolution represents an opportunity for ophthalmology to adapt to new care models. This study aimed to find out how the pandemic has modified the clinical practice and training activities of the ophthalmologist specialised in ocular surface, as well as to analyse emerging trends and needs.
Materials and methodsThis study was carried out through an online survey. A committee of 3 specialists developed a questionnaire of 25 questions structured in: 1) Participant profile; 2) Impact of the pandemic on patient management and professional activities; 3) Trends and needs.
Results68 clinical ophthalmologists participated. There was a high degree of agreement (90%) that the pandemic has delayed ophthalmological follow-up visits and diagnosis. The participants agreed that the frequency of patients with dry eye disease (75%), stye/chalazion (62%) and blepharitis (60%) has increased. According to 28%, remote monitoring of pathologies such as dry eye, glaucoma, diabetes, conjunctivitis, hyposphagmas, styes, etc., will be common, especially in the young population. This will be especially relevant in chronic or mild pathologies of the ocular surface, and in the follow-up of patients after cataract and diabetic retinopathy interventions.
ConclusionsDuring the pandemic, an increase in the incidence of certain ocular surface diseases has been perceived. The telematic follow-up of chronic or mild pathologies of the ocular surface entails the need to provide specific training for both the patient and the healthcare professional, in addition to screening and referral protocols that would optimise the flow of care.
La evolución digital supone una oportunidad para que la oftalmología se adapte a nuevos modelos asistenciales. Este estudio tuvo como objetivo conocer cómo la pandemia ha modificado la práctica clínica y actividades formativas del oftalmólogo especializado en superficie ocular, y analizar tendencias y necesidades emergentes.
Materiales y métodosEstudio realizado mediante encuesta online. Un comité de 3 especialistas diseñó un cuestionario de 25 preguntas estructurado en: 1) Perfil del participante; 2) Impacto de la pandemia en el manejo del paciente y las actividades profesionales; 3) Tendencias y necesidades.
ResultadosParticiparon 68 oftalmólogos clínicos. Hubo un alto grado de acuerdo (90%) en que la pandemia demoró las visitas de seguimiento oftalmológico y el diagnóstico. Los participantes coincidieron en que aumentó la frecuencia de pacientes con enfermedad de ojo seco (75%), orzuelo/chalazión (62%) y blefaritis (60%). Según un 28%, será habitual el teleseguimiento mediante teleconsulta de patologías como ojo seco, glaucoma, diabetes, conjuntivitis, hiposfagmas, orzuelos, etc., especialmente en población joven. Esto será especialmente relevante en las patologías crónicas o leves de la superficie ocular, y en el seguimiento de pacientes tras operación de cataratas y retinopatía diabética.
ConclusionesDurante la pandemia se ha percibido un aumento de la incidencia de ciertas enfermedades de superficie ocular. El seguimiento de patologías crónicas o leves de la superficie ocular se vincula a la necesidad de proporcionar formación específica tanto para el paciente como para el profesional que lo atiende, además de protocolos de cribado y derivación que optimicen el flujo asistencial.
COVID-19 has had serious health consequences worldwide1. In Spain, its impact on the public health budget (12.3% of health expenditure) exceeds the cost of multiple sclerosis, diabetes and cancer2.
Ophthalmology has been greatly affected by the pandemic. García Lorente et al. investigated the use of ophthalmology emergency services during the lockdown and compared the cases treated at the University Hospital of Málaga during the closure period from March to June 2020 with those corresponding to the same period in 2017. The number of cases treated was reduced by 65%, with a differentiation depending on the stage of lockdown3. During strict isolation the number of consultations decreased, with the majority of cases being serious and urgent. In the second stage, with relaxed isolation measures, there was a delay in the diagnosis of other equally serious illnesses, probably due to patients' fear of going to hospital. At the same time, however, the number of ophthalmology patients tripled and the diagnosis of mild conditions prevailed3.
Ophthalmology is often at the forefront of technology. Tele-ophthalmology is one of the leading fields in telemedicine and includes the integration of new devices using artificial intelligence to aid remote patient assessment and screening4. There is an unprecedented opportunity for ophthalmology to successfully adapt to new models of care1.
This study was conducted with the aim of understanding how the COVID-19 pandemic has changed the routine clinical practice and training activities of the ocular surface ophthalmologist, as well as to analyse trends in the specialty and identify emerging needs for the future.
Material and methodsStudy designA quantitative and qualitative study was conducted between May and July 2021, on the impact of the COVID-19 pandemic on the practice of ophthalmology. A scientific committee comprising 3 ophthalmology specialists was in charge of selecting the topics to be addressed and preparing the 25-question survey structured in 3 sections: 1) Participant profile; 2) Impact of the pandemic on patient management and professional activities; 3) Future trends and needs in the next 10 years.
The first section included 9 questions aimed at characterising the professional qualifications and experience of participants in order to ensure that they met the selection criteria. The second section consisted of 9 closed questions to analyse the changes experienced in their care and training practice. The last section comprised 7 questions (5 closed and 2 open). The survey was conducted through an online platform that guaranteed data anonymity and confidentiality.
For the purposes of this analysis, the pandemic period was defined as the period from autumn 2019 to autumn 2020.
Selection of participants and completion of the surveySpecialists were invited to participate if they met the following criteria: being a public or private specialist ophthalmologist in anterior segment, ocular surface and cornea as main or exclusive dedication, with at least 5 years of experience in this speciality and who attended more than 40 patients/week with ocular surface and corneal problems.
Analysis and interpretation of the resultsDescriptive statistical analysis was performed with the SPSS programme® (version 26, IBM, USA). Nominal variables were represented by frequency tables, and continuous variables by measures of central tendency and dispersion. Percentages of agreement were rounded to absolute numbers. To interpret Likert-type ordinal scale items, responses were grouped into 3 levels: 1–3 (disagree/not relevant), 4–6 (neutral) and 7–9 (agree/relevant). When the mean score of a statement was ≥7 the item was considered "agree or relevant", and when it was ≤3 "disagree/irrelevant". Open-ended questions were analysed qualitatively.
ResultsSixty-eight of the 74 ophthalmologists invited agreed to participate, corresponding to the autonomous communities of Catalonia (25%), Madrid (17.6%), Andalusia (17%), Valencia (8.8%), Castilla-La Mancha (7.4%), Castilla y León (5.9%), Canary Islands (4.4%), Cantabria (4.4%), Balearic Islands (2.9%), Murcia (2.9%), Aragón (1.7%) and Asturias (1.5%). Sixty-two percent of respondents were male, and 47% were aged 30–40 years.
Overall, 74% of participants were ocular surface specialists, 64% were anterior segment specialists, 50% were corneal specialists and 52% were also specialists in general ophthalmology; 53% were members of the Spanish Society of Ophthalmology (SEO) and 35% of the Spanish Society of Ocular and Refractive Surgery (SECOIR). Sixty percent of participants worked in both public and private practice. 78% saw more than 100 patients per week, with a weekly average of 80 patients with ocular surface or corneal complaints.
Impact of the pandemic on ophthalmology and ocular surface patient managementComparing autumn 2020 with the same season of the previous year, the total average number of patients seen in ophthalmology practices decreased by 26.8%. Per month, the average number of patients seen via virtual visits increased by 121.7%, much more sharply in the public sector (316.7%), while the number of patients seen in person decreased by 34.6%.
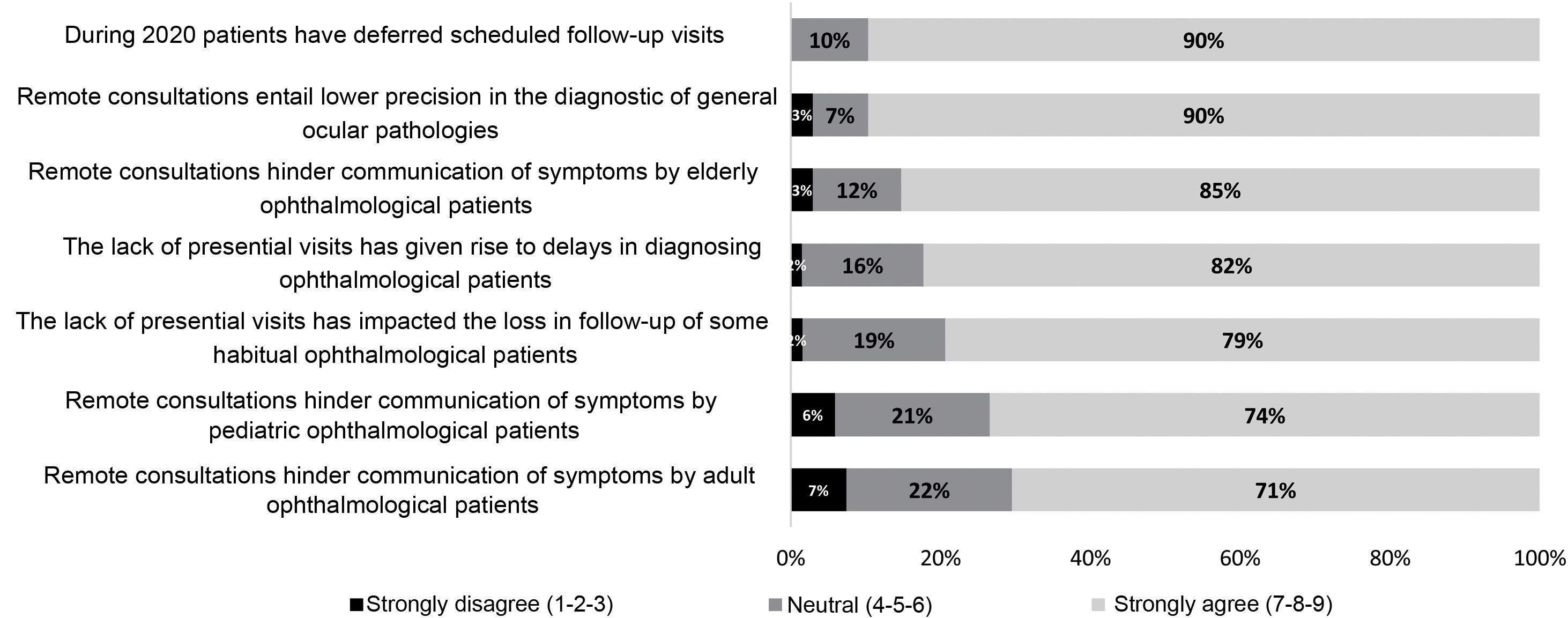
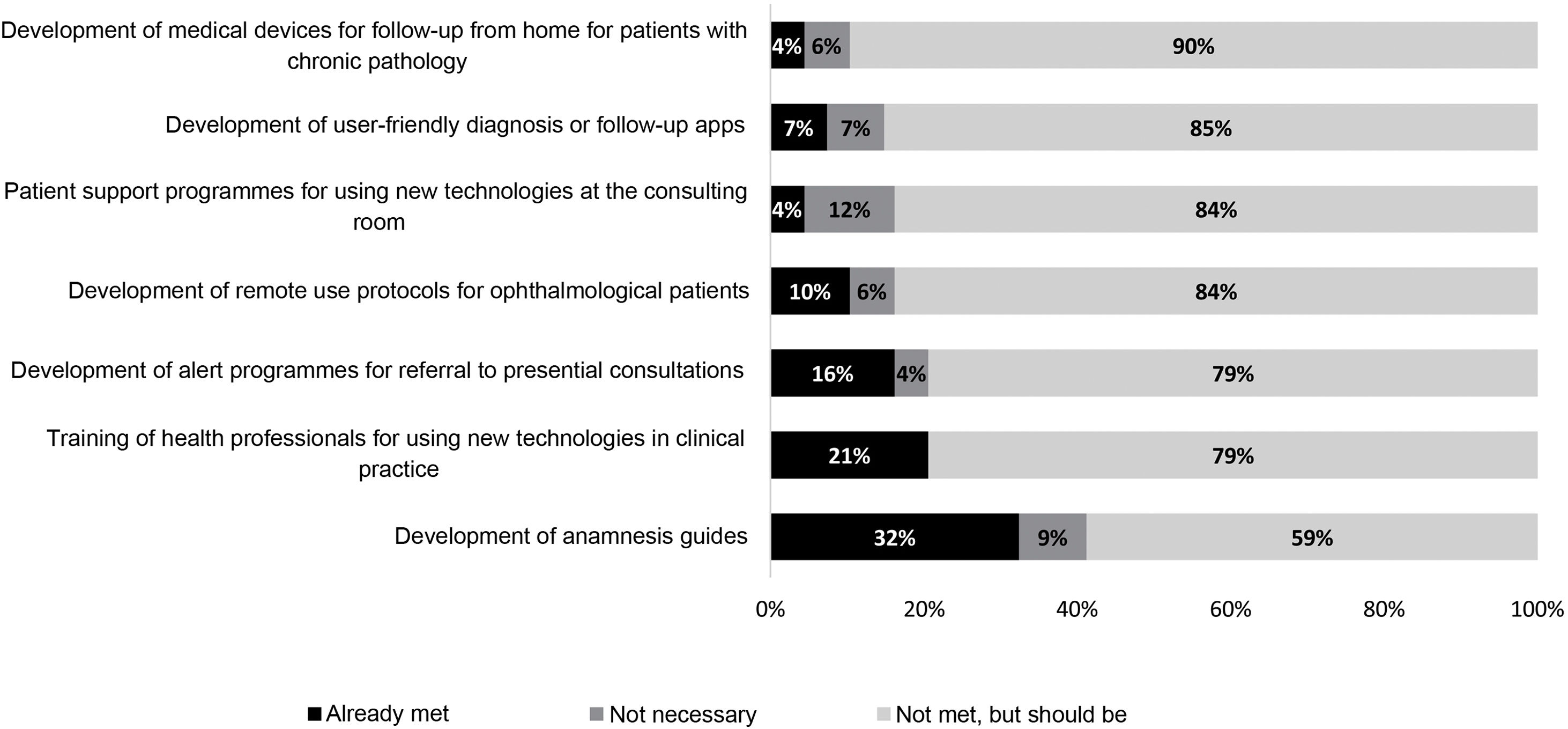
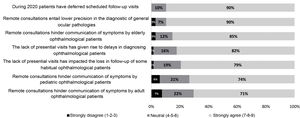
There was a high degree of agreement that the pandemic delayed ophthalmic follow-up visits, with delays in diagnosis and monitoring (Fig. 1). There was a significant increase of 96% in the percentage of patients cancelling a scheduled presential visit (184% in the public sector and 14% in the private sector). In the public sector, there was a significant reduction in the monthly average number of patients referred (33.65%).
In the opinion of participants, the main reason for fewer patient visits was reluctance on the part of the patient (79 and 94% of respondents in public and private settings, respectively). Other reasons were fewer referrals (54 and 26%, respectively) and limited consultation hours (48 and 37%, respectively).
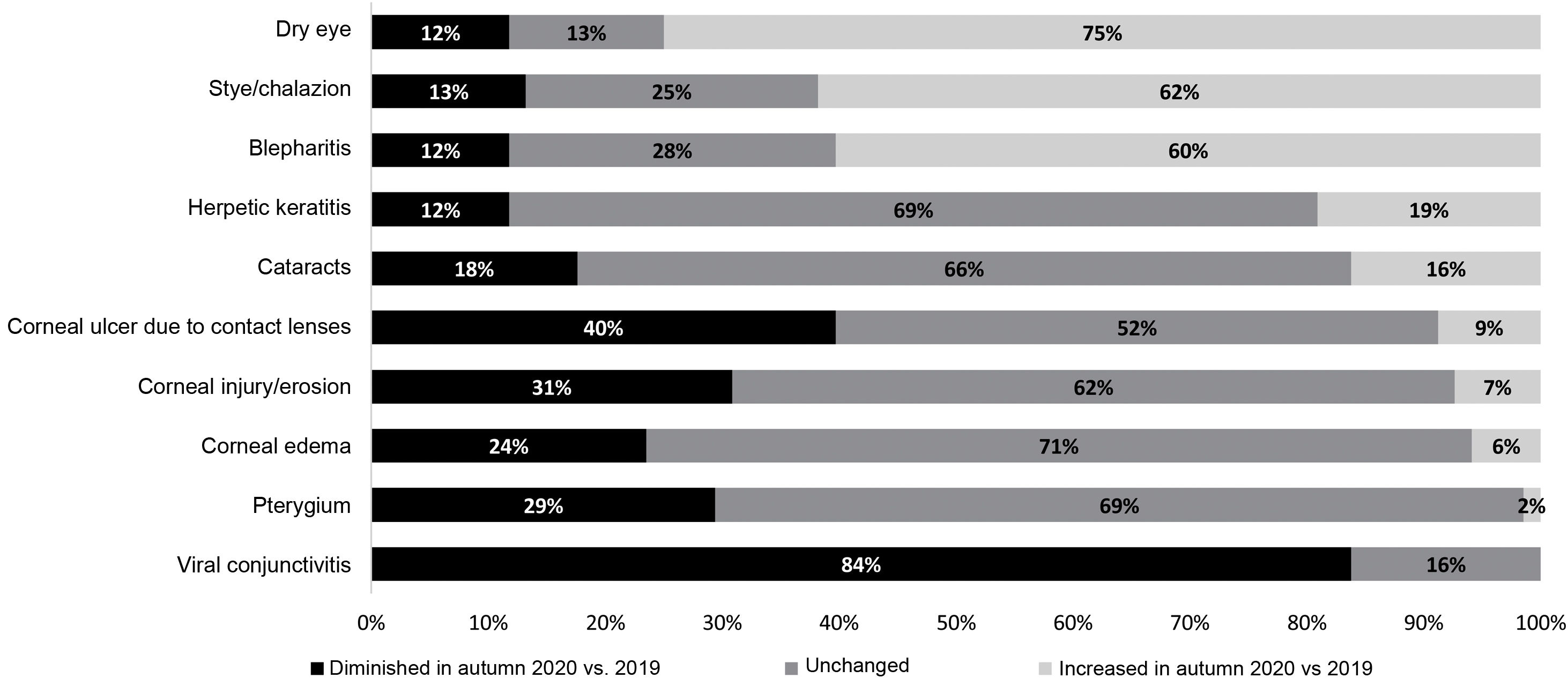
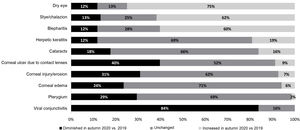
Overall, 65% of the experts stated that the situation of patients seen in ophthalmology practices has worsened after the pandemic. There was a neutral-high degree of agreement (50–66%) that there is evidence of a causal relationship between COVID-19 and ocular manifestations such as dry eye and conjunctivitis. Participants agreed that there has been an increase in the frequency of patients with dry eye disease (75%), stye/chalazion (62%) and blepharitis (60%) (Fig. 2). The incidence of dry eye disease was found to be increased in older adults (77% agreement), over 65 years (75%) and young adults (71%). This increase was attributed to increased exposure to screens or digital devices and prolonged mask use (96% and 87% of participants, respectively).
Impact of the pandemic on professional aspects of ophthalmologyThe average number of congresses attended during 2020 grew significantly, by 71% compared to 2019, with a clear trend towards a virtual format. The same trend was observed for professional meetings. Forty-four percent of participants felt that the pandemic has negatively affected communication between professionals. Despite 84% of ophthalmologists agreeing on the usefulness of digital tools, 56% stressed that face-to-face meetings are still necessary.
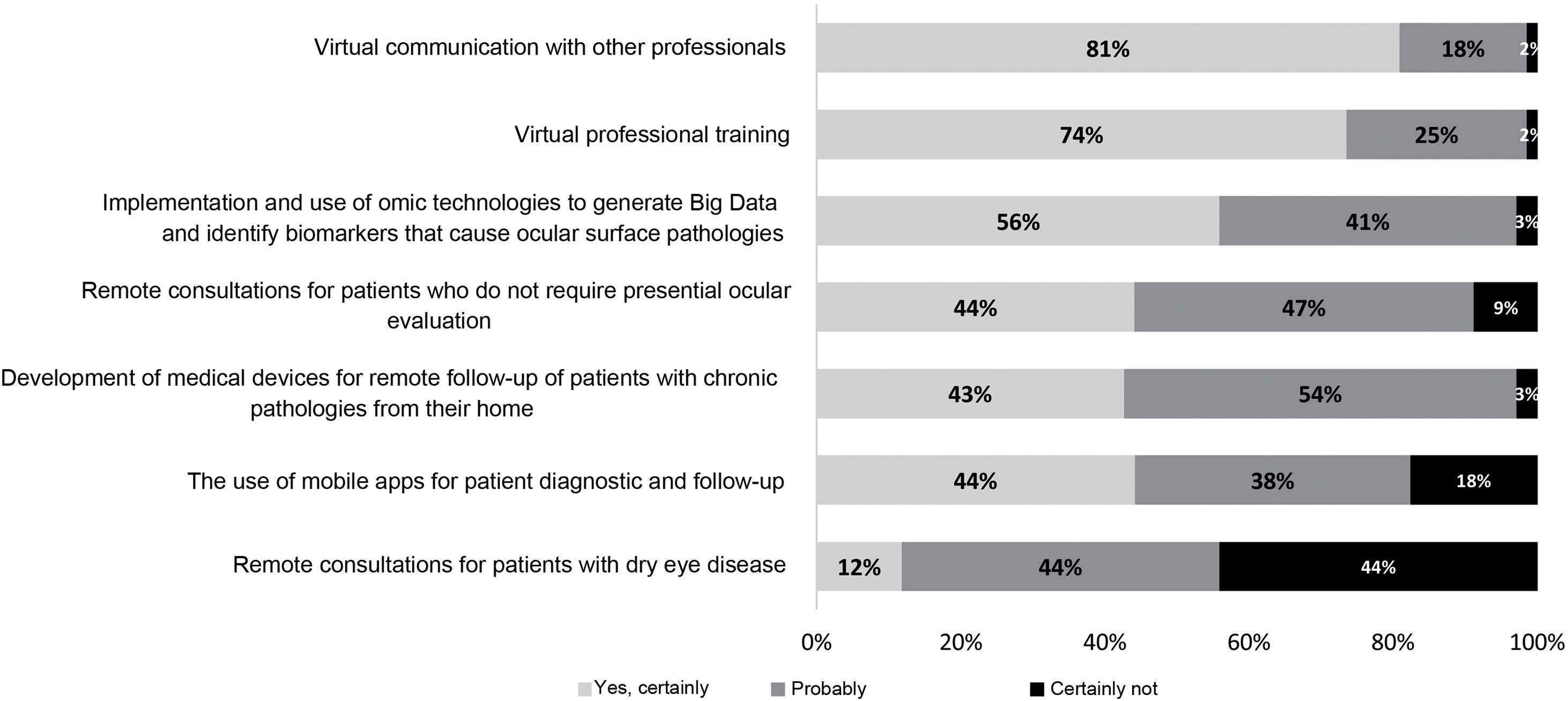
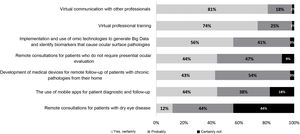
Future trends in ophthalmology and the ocular surfaceSeveral future trends were expressed (Fig. 3). Regarding the disease, 90% agreed that the number of patients with dry eye disease will increase. Virtual consultations will increase, according to 66% of the experts. Regarding the number and frequency of presential visits, they were of the opinion that they will remain the same (54% and 52% of participants, respectively).
The qualitative analysis revealed that, according to 28% of participants, teleconsultation follow-up of patients with conditions such as dry eye, glaucoma, diabetes, conjunctivitis, hyposphagmas, sties, etc. will be common, especially in the young population. This will be particularly important in patients with chronic or non-severe ocular surface disease, and in the follow-up of patients after cataract surgery and diabetic retinopathy. In patients with dry eye, telematic monitoring will be possible through online imaging and always after a face-to-face assessment in which treatment has been instituted. For glaucoma patients, intraocular pressure controls or optical coherence tomography can be monitored remotely. In patients with diabetic retinopathy it will be possible to perform a macular optical coherence tomography and wide-field retinography telematically for annual monitoring.
On the other hand, 43% of ophthalmologists anticipated diagnostic improvements thanks to biomarker-based methods or telematic diagnostic imaging, which may allow initial screening of patients and thus reduce the burden of care. This will require protocols for the correct use of these technologies, which may include new camera for ocular globe scans or the development of apps integrating subjective surveys and images. Fifty-seven percent of participants thought that new treatments are on the way, including improvements in artificial tears.
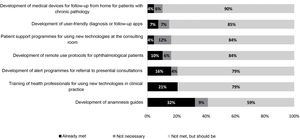
Future needsFig. 4 details the needs in ophthalmology that should be covered in the future. The development of devices for monitoring patients with chronic disease or apps for diagnosis and monitoring were the most frequently expressed needs. Respondents also expressed the need of a simple tool to support daily practice in primary care (PC), as well as applications for shared diagnosis of complex cases. It was suggested to establish protocols for referral to specialised care, implementing fluid communication channels and training PC physicians to advance in the diagnosis and treatment of milder diseases.
The role of artificial intelligence in ophthalmology was highlighted, which could be linked to the use of images to generate algorithms or medical decision support systems. Technological training for professionals was considered necessary, as well as training for patients in self-care strategies and communication with the healthcare professional.
DiscussionThe present study provides insight into the perception of 68 Spanish ocular surface specialists on how the COVID-19 pandemic has changed the clinical practice of ophthalmologists. It reveals new ways of interacting with patients and new technological challenges.
Our study found that during the pandemic the average number of examined patients decreased by almost 27%. This is consistent with a recent survey of 504 ophthalmology residents from 32 countries. According to most respondents, clinical activity during the pandemic decreased by 50% and surgical activity by 75%5. This survey analysed the changes experienced in terms of clinical activity, surgical practice and teaching, as well as the perception of the impact on their current and future training. More than 50% of residents felt that the pandemic drastically influenced their specialty5.
Participants in our study agreed that during the pandemic the frequency of patients with dry eye disease, stye/chalazion and blepharitis has increased. Pandemic-related factors, such as increased use of screens or face masks have been described as contributing to the increase in dry eye cases6–8.
It is worth recalling that interest in teleophthalmology predates the pandemic. In 2018, the Telemedicine Task Force of the American Ophthalmological Society published a policy paper on the development and implementation of this format, including validation of a teleophthalmology programme, different requirements on data acquisition and devices used, qualification of the personnel involved, and quality assurance and data protection9.
Successful examples of tele-ophthalmology have been reported in different countries for the detection and monitoring of diabetic retinopathy, age-related macular degeneration, retinopathy of prematurity, or anterior segment diseases10–14. According to 28% of participants in this study, telemonitoring via teleconsultation of patients with conditions such as dry eye, glaucoma, diabetes, conjunctivitis, hyposphagmas, sties, etc. will be common in the future. More than 40% anticipated diagnostic improvements thanks to biomarker-based methods or telematic diagnostic imaging. With continued improvements in image processing and integration with patient medical history, tele-ophthalmology could expand its clinical applications15 and patients could benefit from better detection and earlier treatment4.
Medical and lifestyle data collected through apps are becoming the cornerstone of big data and are being used for individualised diagnosis and treatment, as is already the case for dry eye disease16,17. It could also be used to predict disease progression or response to treatment1,18.
There are unmet needs in this field. Survey participants expressed needs such as technological training for professionals or the availability of apps in PC that allow for correct screening and referral of patients to specialised care. The training of healthcare professionals such as nurses, optometrists and technicians by ophthalmologists would help to share the tele-ophthalmology workload, which would allow more complex cases to be referred to ophthalmologists and optimise the process. This model has already been adopted in several countries12,19–21.
However, there are barriers to overcome for widespread adoption of said model, such as validation of safety and efficacy for patients, reluctance on the part of doctors and patients, the need to acquire technological skills, or legal regulations1,22.
It is essential to promote health education to raise public awareness and distinguish serious problems that require urgent attention from those that do not, optimising the use of medical services. Given the world's ageing population, artificial intelligence and telemedicine can help alleviate the relative shortage of professionals due to an increase in the number of patients, as well as having the potential to transform access to and delivery of healthcare. We are confident that the results of this study will contribute to progress in this regard.
ConclusionsParticipants in this study have expressed that, during the pandemic, an increase in the incidence of ocular surface diseases such as dry eye disease has been observed, mainly due to increased exposure to screens and the use of masks, a trend that is likely to continue in the future.
Although there has been a clear increase in the virtual format, presential visits are still necessary.
The possibility of telematic monitoring via teleconsultation or remote monitoring of patients with certain chronic or mild ocular surface diseases is linked not only to the need for technological training, but also to investment in technology to make this possible, as well as screening protocols and referral from PC to ophthalmology specialists to increase dialogue between both. In addition, training should be designed to raise patient awareness of the importance of ocular surface disorders and to improve the management of their disease, thus optimising the quality of care.
FundingThis work has been funded by Angelini Pharma España.
Conflict of interestJMBC declares having received fees from Angelini Pharma España during the conduct of the study and from Alcon, Allergan, Brill Pharma, Lumenis, Novartis, Santen Pharmaceutical Spain and Thea.
NAA declares having received fees from Angelini Pharma España during the conduct of the study and from Alcon, Esteve, Rayner, GSK, Bausch & Lomb, Johnson & Johnson, AJL, Medical Mix and 2Eyes Vision.
IH declares having received fees from Angelini Pharma España during the conduct of the study.
MPF reports the existence of an employment contract, now terminated, with Angelini Pharma España during the period of the study.
MÁ reports the existence of a professional contract with Angelini Pharma España and Adelphi Targis for the performance of this work.