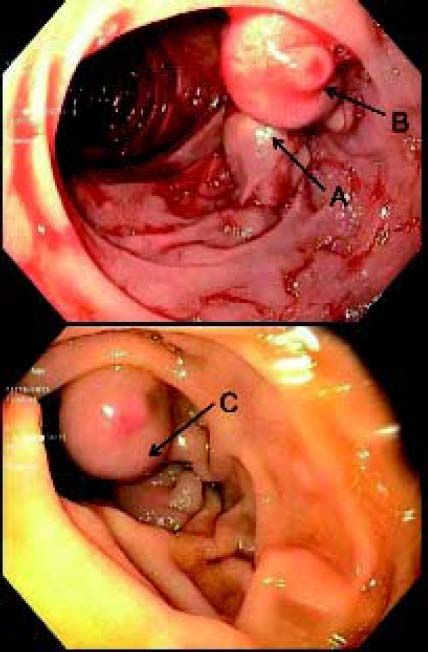
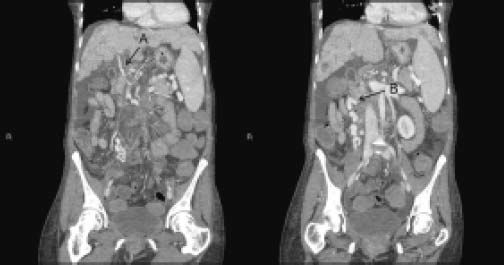
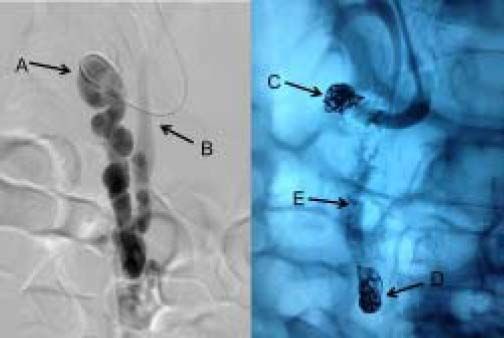
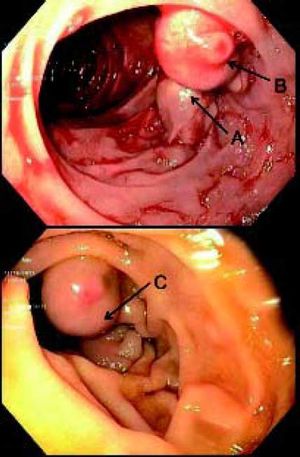
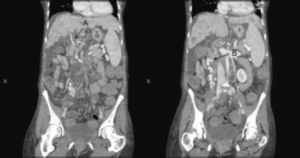
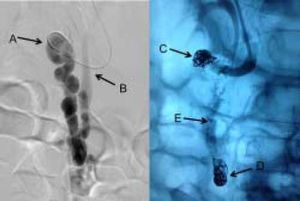
A 50 yo female with PSC and a bleeding duodenal varix (DV) was evaluated for possible enbucrilate therapy. Endoscopically (Figure 1), the DV was high risk for rebleeding but the relative in-flow and out-flow were uncertain. CT (Figure 2) showed portal vein thrombosis (PVT) and the vascular anatomy of the DV to consist of inflow from the superior mesenteric vein (SMV) with outflow through the DV and the right gonadal vein. Moreover, the more distal and narrower aspect of the varix was seen to constitute the constricted outflow of the varix rather than a small caliber inflow channel. Endoscopic enbucrilate was deemed to carry high risk of varix rupture or mesenteric venous occlusion and bowel ischemia. An angiographic approach was elected to open the portal outflow through a TIPs and once outflow was established to embolize the duodenal varix internally through balloon occluded antegrade transvenous obliteration (BATO).1 Angiography confirmed that splenic and mesenteric in flow was directed to the duodenal varix (Figure 3, arrow A) in a superior to inferior direction with ‘downward’ outflow through the gonadal vein (Figure 3, arrow B). Once the TIPS was established to provide a low resistance pathway, the outflow track to the gonadal vein was occluded using metallic coils and the varix was sclerosed using a mixture of sotradecol, Lipiodol, and air foam. The catheter was then withdrawn further and the inflow to the DV was occluded with metallic coils and a vascular plug (Figure 3, arrows C & D). The PVT was then thrombolysed using a mechanical approach and scant tPA and the small TIPS shunt was left in place due to increased HVPG. Subsequently, endoscopy revealed an occluded duodenal varix (Figure 1, arrow C) confirmed by Doppler probe. Management of ectopic varices can be very difficult as evidenced in this case.2 Careful evaluation of the underlying vascular anatomy and subsequent analysis of the concepts of vascular flow and resistance are essential to guide optimal therapy whether by one approach or another or by a combined approach.3
The endoscopic appearance of the bleeding duodenal varix before treatment (top panel) and after treatment (bottom panel). A. The outflow track of the duodenal varix through the right gonadal vein. B. The inflow track to the duodenal varix from the SMV and the high risk area where bleeding occurred. C. The duodenal varixpost-treatment. Note the palor and the diminution of the outfow track.
The fluoroscopic appearance of the duodenal varix before treatment (left panel) and after treatment (right panel). A. The inflow to the varix from the SMV. B. The outflow of the varix through the gonadal vain. C. The coil at the inflow track. D. The coil at the outflow track. E. Arrow pointing to the location of the duodenal varix.
- •
BATO: balloon occluded antegrade transvenous obliteration.
- •
DV: duodenal varix.
- •
HVPG: hepatic venous pressure gradient.
- •
PSC: primary sclerosing cholangitis.
- •
PVT: portal vein thrombosis.
- •
SMV: superior mesenteric vein.
- •
TIPS: transjugular intrahepatic portosystemic shunt.