This observational retrospective study aimed to analyse the mortality trends of Parkinson's disease (PD) in Spain from 1999 to 2021, by autonomous community and sex.
MethodsThe study collected PD mortality data from 1999 to 2021 from the National Statistics Institute of Spain. Age-standardised mortality rates were analysed by sex and age group, using joinpoint analysis to identify significant trends.
ResultsOver the study period, 72907 deaths due to PD were recorded in Spain, with 51% occurring in men and 49% in women. Both men and women showed a consistent upward trend in PD mortality rates at the national level, with annual increases of 2.1% for men and 2.0% for women. Joinpoint analysis revealed significant changes in trends within specific regions. Among men, rates in Catalonia stabilised after an initial increase, whereas Madrid showed a significant increase after a period of stability. Conversely, La Rioja exhibited a notable decrease after a period of increase. Similar patterns were observed for women, with certain regions showing stable rates while others displayed an upward trend. Cantabria, Galicia, and Valencia stabilised after an initial significant increase, Madrid showed a significant increase after a period of stability, and Andalusia demonstrated an acceleration after an initial increase.
ConclusionsOur findings underscore the significance of monitoring PD mortality trends and their varying impact across different regions and sexes. This valuable information can play a crucial role in shaping future healthcare policies and designing effective prevention strategies.
Este estudio observacional retrospectivo tuvo como objetivo analizar las tendencias de mortalidad por enfermedad de Parkinson (EP) en España desde 1999 hasta 2021 por comunidades autónomas y sexo.
MétodosEl estudio recogió datos de mortalidad por EP de 1999 a 2021 del Instituto Nacional de Estadística de España. Las tasas de mortalidad estandarizadas por edad se analizaron por grupos de edad y sexo, utilizando un análisis joinpoint para identificar tendencias significativas.
ResultadosDurante el periodo de estudio, España registró 72.907 muertes por EP, de las cuales el 51% se produjeron en hombres y el 49% en mujeres. Tanto hombres como mujeres mostraron una consistente tendencia al alza en las tasas de mortalidad relacionadas con la EP a nivel nacional, con incrementos anuales del 2,1% para los hombres y del 2,0% para las mujeres. El análisis Joinpoint reveló cambios significativos en las tendencias dentro de regiones específicas. En el caso de los hombres, las tasas de Cataluña se estabilizaron tras un aumento inicial, mientras que Madrid experimentó un aumento significativo tras un periodo de estabilidad. Por el contrario, La Rioja experimentó un notable descenso tras un periodo de aumento. En el caso de las mujeres se observaron pautas similares, ya que algunas regiones mostraron tasas estables, mientras que otras mostraron una tendencia al alza. Cantabria, Galicia y Valencia se estabilizaron tras un aumento significativo inicial, Madrid mostró un aumento significativo tras un periodo de estabilidad y Andalucía mostró una aceleración tras un aumento inicial.
ConclusionesNuestros hallazgos subrayan la importancia de monitorizar las tendencias de mortalidad por EP y su impacto variable en diferentes regiones y sexos. Esta valiosa información puede desempeñar un papel crucial en la configuración de futuras políticas sanitarias y en el diseño de estrategias de prevención eficaces.
Parkinson's disease (PD) presents a significant global health challenge, ranking as the second most common neurodegenerative disorder worldwide, following Alzheimer disease.1 Its prevalence is increasing, making it a leading cause of disability worldwide.2 In 2016, there were 6.1 million PD patients worldwide, representing a 21.7% increase in age-standardised prevalence since 1990.3 A recent study from 1990 to 2019 indicates a consistent growth in PD incidence, prevalence, and years lived with disability, particularly among patients aged over 65 years, with a notable increase in those over 80 years old.1
PD prevalence and incidence vary significantly across different regions globally. Europe and the United States generally exhibit higher prevalence rates compared to Asia, Latin America, and Africa. PD rates are lowest in Africa due to specific population factors and limited economic resources leading to higher mortality rates.4
In Spain, PD shows similar incidence and prevalence rates to the rest of Europe, significantly impacting patients’ quality of life and nearly doubling patient mortality. Moreover, the disease poses substantial costs, which are expected to rise with population ageing and the emergence of new therapies.5 Notably, PD hospitalisations in Spain have been on a steady incline from 1997 to 2019, with a higher prevalence among older men with comorbidities.6
A recent study published in Neurologia7 revealed a significant increase in PD mortality rates in Spain from 1981 to 2020, affecting both sexes. However, there is a lack of research specifically examining PD mortality at the autonomous community (AC) level in Spain. Although studies at the provincial8 and municipal9 levels have provided valuable insights into the geographical distribution and potential risk factors of PD mortality, more comprehensive investigations at the AC level are necessary to gain a broader understanding of the disease's impact in different regions of the country. By monitoring PD mortality trends at the regional level, we can gather valuable information on the epidemiology and public health impact of this disease.
Taking into account all of the above, our study aims to present an updated, comprehensive analysis of PD mortality rates in Spain, covering the period from 1999 to 2021, and also considering variations by sex and AC. In doing so, we hope to provide essential information to improve the understanding and management of PD in Spain.
Materials and methodsData sourceThe data used for this study were sourced from the Spanish National Statistics Institute. We obtained data on the population, estimated on 1 July each year, and mortality for the period 1999–2021. These datasets were disaggregated based on age, sex, and calendar period, providing a comprehensive foundation for our analysis. Deaths due to PD were classified with International Classification of Diseases 10th Revision (ICD-10) code G20. Specifically, we included only those cases in which this code was listed as the underlying cause of death.
Statistical analysis:Age-standardised mortality rates (ASMR) for all age groups were estimated and reported as rates per 100000 population. These rates were calculated using the direct method, with the European Standard Population 2013 serving as the reference population.14
Estimation and analysis of ASMR trends for PD was performed with the Joinpoint regression software (version 5.0.2).15 The software default settings were used to specify the appropriate modelling method, criteria for determining the location of inflection points in the correlated error options, and the method for selecting the model.16
The annual percentage change (APC) for each segment was estimated by fitting a regression line to the natural logarithm of the rate, with the calendar year as the independent variable. To assess the significance of inflection points, the analysis commenced with the minimum number of points (i.e., 0 points, representing a straight line).
To quantify the overall trend over the entire study period (1999–2021) and facilitate comparisons between different calendar periods, we calculated the average annual percentage change (AAPC). This was accomplished by computing a geometrically weighted average of the different APCs derived from the joinpoint regression analysis, with weights corresponding to the length of each segment during the specified time interval (1999–2021).
To determine the direction of change in mortality rates, we adopted the following criteria: rates were considered to be increasing if the slope of the trend (APC or AAPC) was greater than zero (P<.05), decreasing if the slope was less than zero (P<.05), and stable otherwise.
We followed the Guidelines for Accurate and Transparent Health Estimates Reporting standards.10
Ethical considerationsThis study did not require ethics or institutional review board approval, as we used publicly available aggregated data without identifying individual patients.
ResultsBetween 1999 and 2021, a total of 72907 deaths due to PD were recorded in Spain, with 51% (37367 deaths) occurring in men and 49% (35540 deaths) in women. The proportion of deaths among individuals aged 75 years and older increased considerably over the study period, with consistently higher percentages observed in women than in men. For men, this proportion rose from 78.2% in 1999 to 85.1% in 2021, with an average annual proportion of 84.5%. Similarly, for women, the proportion increased from 84.5% in 1999 to 90.8% in 2021, with an average annual proportion of 89.9%.
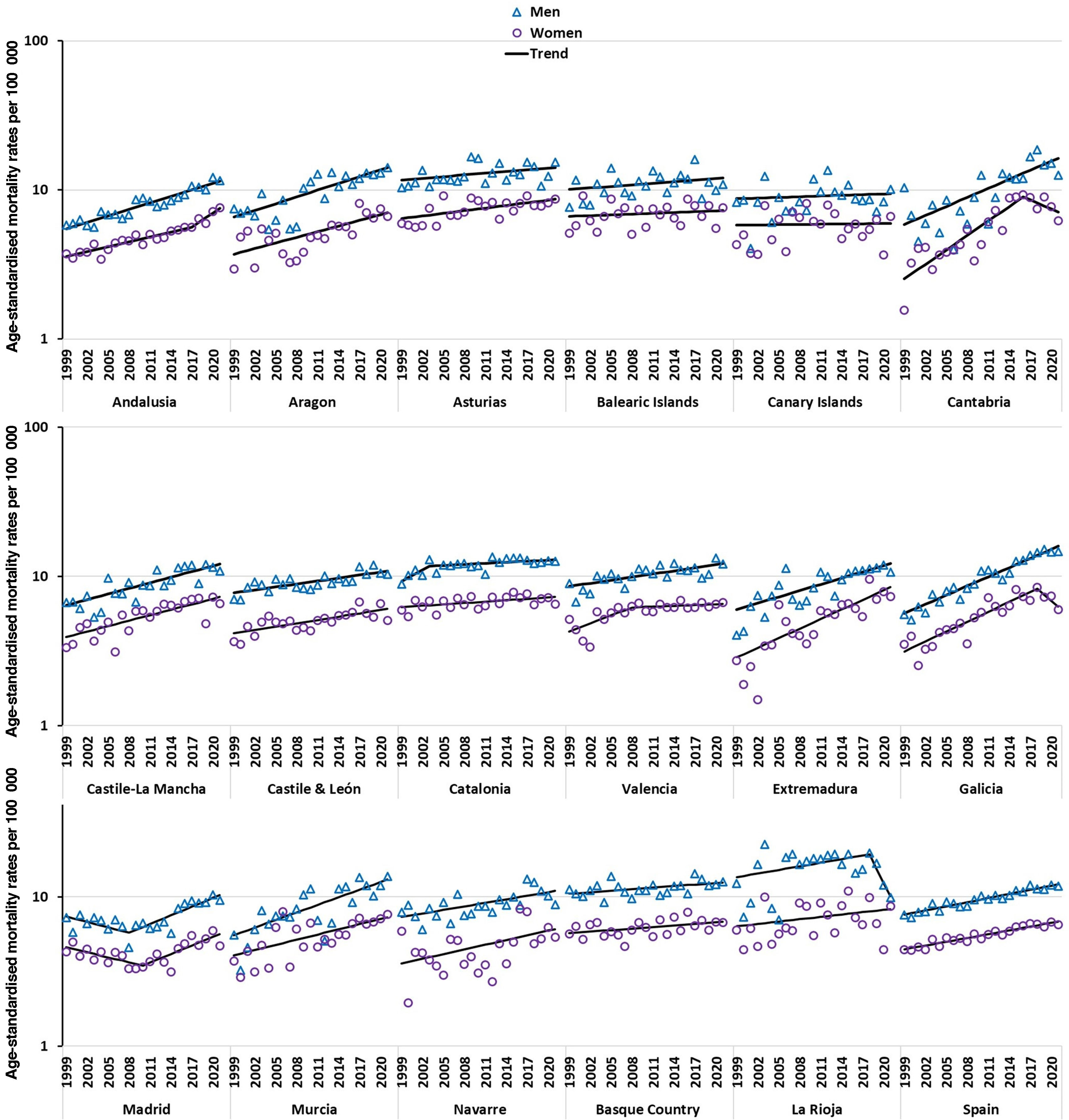
Fig. 1 presents the age-standardised rates, segregated by sex, both at the national level and for each autonomous community, alongside the estimated trends derived from the joinpoint analysis. The results demonstrate compelling evidence of a continuous upward trend in PD mortality rates for both men and women across the entire country from 1999 to 2021. Notably, the data reveal a parallel annual increase in mortality rates of 2.1% for men and 2.0% for women during this period.
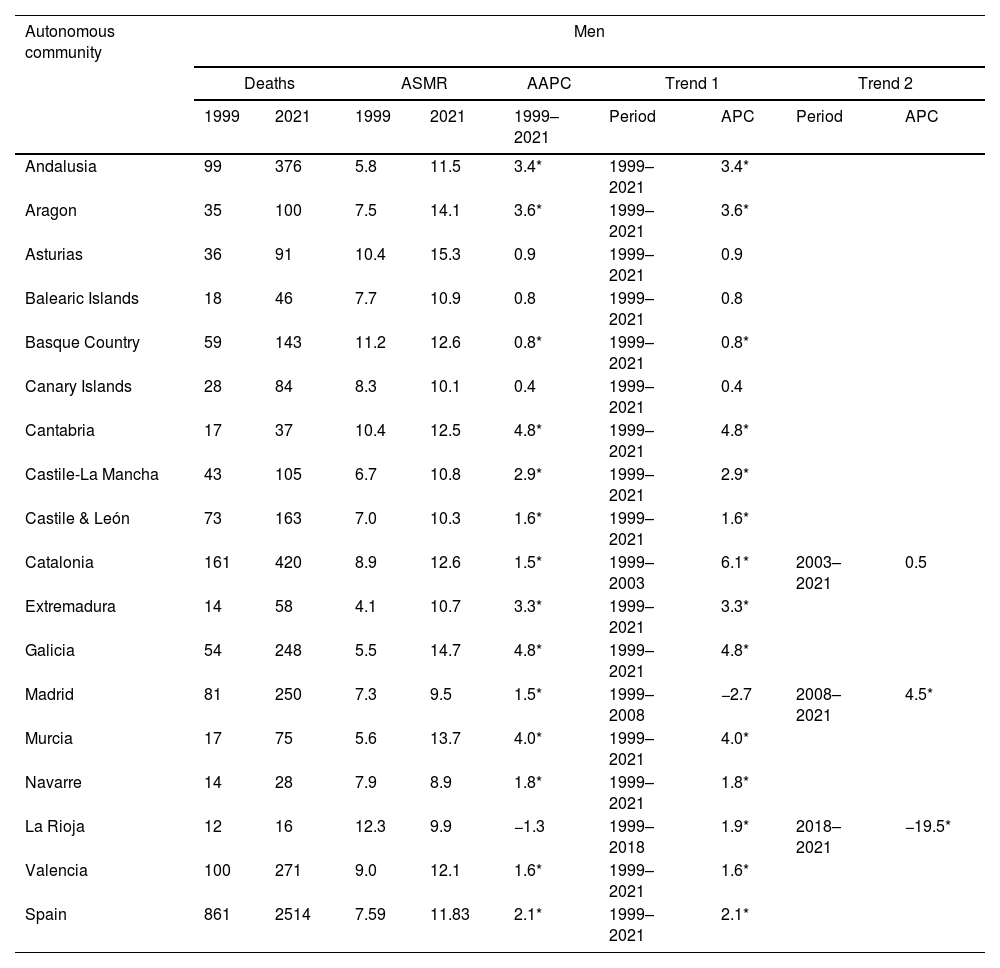
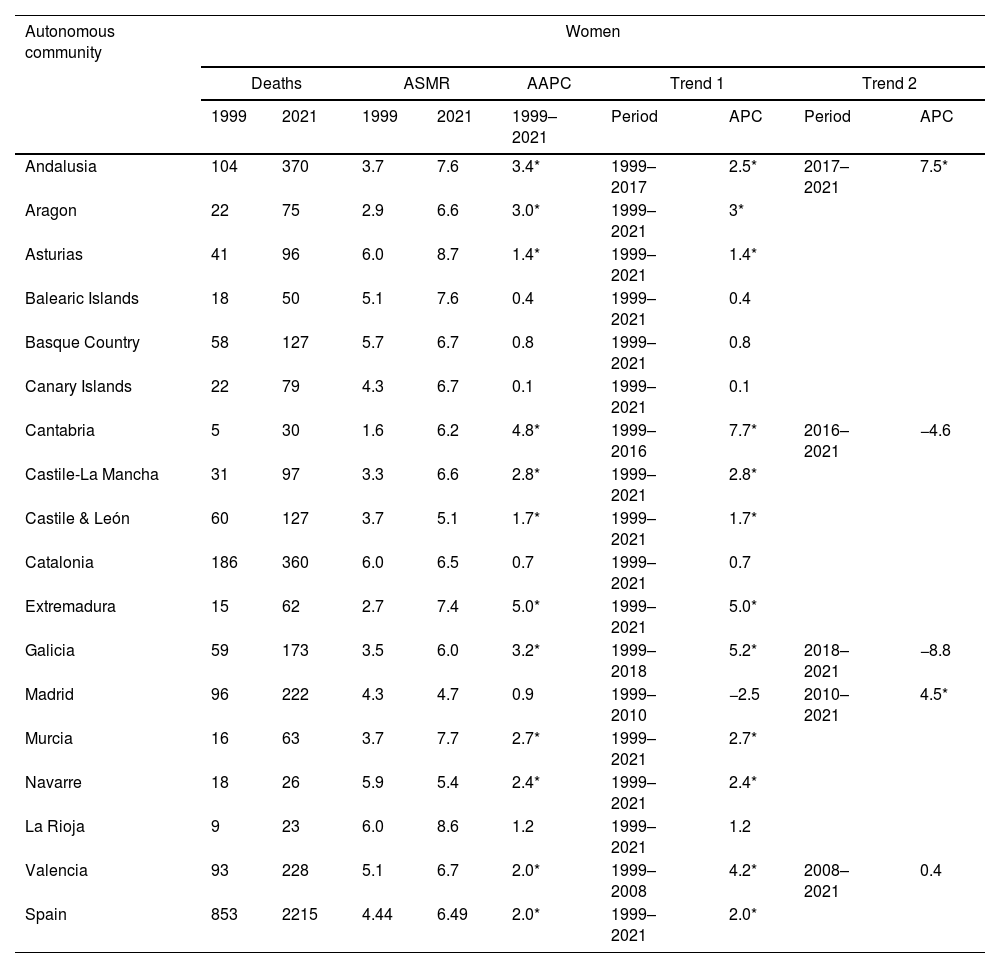
Tables 1 and 2 offer a detailed and comprehensive analysis of PD mortality in 1999 and 2021, providing insights into age-standardised mortality rates, AAPC, and trends identified through joinpoint analysis for both men and women. Data are presented separately for each AC in Spain, as well as for the country as a whole.
Deaths and age-standardised mortality rates (all ages) for the years 1999 and 2021, as well as the average annual percentage change (AAPC) for the period (1999–2021) and joinpoint results in men for each autonomous community and for Spain as a whole.
| Autonomous community | Men | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Deaths | ASMR | AAPC | Trend 1 | Trend 2 | |||||
| 1999 | 2021 | 1999 | 2021 | 1999–2021 | Period | APC | Period | APC | |
| Andalusia | 99 | 376 | 5.8 | 11.5 | 3.4* | 1999–2021 | 3.4* | ||
| Aragon | 35 | 100 | 7.5 | 14.1 | 3.6* | 1999–2021 | 3.6* | ||
| Asturias | 36 | 91 | 10.4 | 15.3 | 0.9 | 1999–2021 | 0.9 | ||
| Balearic Islands | 18 | 46 | 7.7 | 10.9 | 0.8 | 1999–2021 | 0.8 | ||
| Basque Country | 59 | 143 | 11.2 | 12.6 | 0.8* | 1999–2021 | 0.8* | ||
| Canary Islands | 28 | 84 | 8.3 | 10.1 | 0.4 | 1999–2021 | 0.4 | ||
| Cantabria | 17 | 37 | 10.4 | 12.5 | 4.8* | 1999–2021 | 4.8* | ||
| Castile-La Mancha | 43 | 105 | 6.7 | 10.8 | 2.9* | 1999–2021 | 2.9* | ||
| Castile & León | 73 | 163 | 7.0 | 10.3 | 1.6* | 1999–2021 | 1.6* | ||
| Catalonia | 161 | 420 | 8.9 | 12.6 | 1.5* | 1999–2003 | 6.1* | 2003–2021 | 0.5 |
| Extremadura | 14 | 58 | 4.1 | 10.7 | 3.3* | 1999–2021 | 3.3* | ||
| Galicia | 54 | 248 | 5.5 | 14.7 | 4.8* | 1999–2021 | 4.8* | ||
| Madrid | 81 | 250 | 7.3 | 9.5 | 1.5* | 1999–2008 | −2.7 | 2008–2021 | 4.5* |
| Murcia | 17 | 75 | 5.6 | 13.7 | 4.0* | 1999–2021 | 4.0* | ||
| Navarre | 14 | 28 | 7.9 | 8.9 | 1.8* | 1999–2021 | 1.8* | ||
| La Rioja | 12 | 16 | 12.3 | 9.9 | −1.3 | 1999–2018 | 1.9* | 2018–2021 | −19.5* |
| Valencia | 100 | 271 | 9.0 | 12.1 | 1.6* | 1999–2021 | 1.6* | ||
| Spain | 861 | 2514 | 7.59 | 11.83 | 2.1* | 1999–2021 | 2.1* | ||
AAPC: average annual percentage change; APC: annual percentage change; ASMR: age-standardised mortality rates per 100000.
Deaths and age-standardised mortality rates (all ages) for the years 1999 and 2021, as well as the average annual percentage change (AAPC) for the period (1999–2021) and joinpoint results in women for each autonomous community and for Spain as a whole.
| Autonomous community | Women | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Deaths | ASMR | AAPC | Trend 1 | Trend 2 | |||||
| 1999 | 2021 | 1999 | 2021 | 1999–2021 | Period | APC | Period | APC | |
| Andalusia | 104 | 370 | 3.7 | 7.6 | 3.4* | 1999–2017 | 2.5* | 2017–2021 | 7.5* |
| Aragon | 22 | 75 | 2.9 | 6.6 | 3.0* | 1999–2021 | 3* | ||
| Asturias | 41 | 96 | 6.0 | 8.7 | 1.4* | 1999–2021 | 1.4* | ||
| Balearic Islands | 18 | 50 | 5.1 | 7.6 | 0.4 | 1999–2021 | 0.4 | ||
| Basque Country | 58 | 127 | 5.7 | 6.7 | 0.8 | 1999–2021 | 0.8 | ||
| Canary Islands | 22 | 79 | 4.3 | 6.7 | 0.1 | 1999–2021 | 0.1 | ||
| Cantabria | 5 | 30 | 1.6 | 6.2 | 4.8* | 1999–2016 | 7.7* | 2016–2021 | −4.6 |
| Castile-La Mancha | 31 | 97 | 3.3 | 6.6 | 2.8* | 1999–2021 | 2.8* | ||
| Castile & León | 60 | 127 | 3.7 | 5.1 | 1.7* | 1999–2021 | 1.7* | ||
| Catalonia | 186 | 360 | 6.0 | 6.5 | 0.7 | 1999–2021 | 0.7 | ||
| Extremadura | 15 | 62 | 2.7 | 7.4 | 5.0* | 1999–2021 | 5.0* | ||
| Galicia | 59 | 173 | 3.5 | 6.0 | 3.2* | 1999–2018 | 5.2* | 2018–2021 | −8.8 |
| Madrid | 96 | 222 | 4.3 | 4.7 | 0.9 | 1999–2010 | −2.5 | 2010–2021 | 4.5* |
| Murcia | 16 | 63 | 3.7 | 7.7 | 2.7* | 1999–2021 | 2.7* | ||
| Navarre | 18 | 26 | 5.9 | 5.4 | 2.4* | 1999–2021 | 2.4* | ||
| La Rioja | 9 | 23 | 6.0 | 8.6 | 1.2 | 1999–2021 | 1.2 | ||
| Valencia | 93 | 228 | 5.1 | 6.7 | 2.0* | 1999–2008 | 4.2* | 2008–2021 | 0.4 |
| Spain | 853 | 2215 | 4.44 | 6.49 | 2.0* | 1999–2021 | 2.0* | ||
AAPC: average annual percentage change; APC: annual percentage change; ASMR: age-standardised mortality rates per 100000.
We observed an annual increase in the number of deaths in men at both the national level (8% per year) and in each AC. The magnitude of this increase varied across different regions, ranging from 1% in La Rioja to 16% in Galicia.
Our study reveals that, at both the national and AC levels, men consistently exhibited slightly higher PD mortality rates than women. In the year 2021, the male-to-female ratio for PD mortality varied across regions, with La Rioja having a ratio of 1.15, whereas Galicia showed the highest ratio, at 2.45.
Over the study period, national ASMRs for PD consistently showed a significant upward trend. However, when analysing the data at the AC level, we identified two distinct patterns. Some regions, namely Asturias, the Balearic Islands, the Canary Islands, and La Rioja, exhibited stable rates with no significant changes in trends. On the other hand, the remaining ACs presented increasing rates, with APC ranging from 0.8% in the Basque Country to 4.8% in Cantabria and Galicia.
The joinpoint analysis conducted did not reveal any significant changes in the trend at the AC level, except in specific regions. Among men, in Catalonia, the rates stabilised after a period of increase from 1999 to 2003 (APC: 6.1%, P<.05), whereas from 2003 to 2021, rates showed a non-significant APC of 0.5%. Similarly, in Madrid, there was a significant increase in rates after a period of stable rates from 1999 to 2008 (APC: −2.7%, non-significant), with an APC of 4.5% from 2008 to 2021 (P<.05). In La Rioja, rates exhibited a substantial decrease following a period of increase from 1999 to 2018 (APC: 1.9%, P<.05), with a significant APC of −19.5% from 2018 to 2021 (P<.05).
Among women, we also observed an annual increase in the number of deaths due to PD, both nationally (7% per year) and within each AC. The magnitude of this increase varied between regions, ranging from 2% per year in Navarre to 22% per year in Cantabria.
Similar to men, the national ASMRs for PD among women showed a consistent upward trend throughout the study period. At the AC level, we identified two different patterns. Stable rates were observed in the Balearic Islands, the Canary Islands, Catalonia, Madrid, the Basque Country, and La Rioja. On the other hand, the remaining ACs exhibited increasing rates, with annual percentage variations ranging from 1.4% in Asturias to 5.0% in Extremadura.
The joinpoint analysis conducted did not reveal any significant changes in the trend at the AC level, except in specific regions. For instance, in Cantabria, Galicia, and Valencia, rates stabilised after an initial period of significant increase. Meanwhile, in Madrid, rates increased significantly after an initial period of stability, and in Andalusia, rates accelerated after an initial period of increase.
DiscussionThe findings of our nationwide study are consistent with the recent literature, underscoring a substantial increase in PD mortality rates on a global scale.11 Notably, countries such as the United States,12 China,13 and Italy14 have presented significant upward trends in PD mortality rates.
Our study findings demonstrate a significant disparity in PD mortality rates between men and women, with higher rates observed in men; this is consistent with previous research.7,15 These disparities in the male-to-female ratios suggest potential variations in PD prevalence, risk factors, or use of health services, and emphasise the need for further investigation to better understand the underlying factors contributing to these differences.
The exact reasons for this difference remain unclear, but several factors have been suggested that may contribute to this phenomenon. These include hormonal influences,16 genetic factors,17 use of health services,18,19 lifestyle aspects,20 and responses to treatment.21 Recent studies have highlighted the importance of biological sex in the development and expression of PD.19,22 While men are more likely to develop PD than women, women with PD tend to present more rapid disease progression and higher mortality rates than men with PD.15 Understanding these sex-related differences in PD is crucial as they have implications for disease management and treatment. Tailored interventions and innovative programmes that consider the distinct needs of men and women with PD can potentially improve patient care.22
While the precise cause of PD remains unknown, the observed increase in mortality rates can be attributed to multiple factors. Firstly, population ageing plays a significant role, as PD is more prevalent among elderly individuals. Although women generally have a longer life expectancy than men, a counterintuitive pattern emerges when examining rates of mortality due to PD in individuals over the age of 75 years. While the mortality rate for PD is higher in men than in women in this age group, a significantly higher proportion of women in this age range die from PD than men. Moreover, our data demonstrate a progressive increase in this proportion over time, highlighting the ongoing importance of monitoring and understanding the impact of PD mortality trends. This shift in the age of death indicates an improvement in the survival of PD patients, potentially due to advances in social and healthcare conditions over time. However, it is also plausible that the increased incidence of PD in older age groups, resulting from progressive population ageing, might contribute to this trend. Secondly, improved awareness and diagnosis of PD have led to better identification and recording of cases. Thirdly, advances in diagnostic methods have facilitated early detection of PD and more accurate reporting of PD deaths. Additionally, medication-related effects and the occurrence of earlier onset and cognitive impairment in certain cases (as supported by previous studies)23,24 may contribute to the observed increase in mortality rates.
Furthermore, our study reveals regional variations in PD mortality rates, emphasising the importance of considering local factors and healthcare disparities in public health interventions. Understanding stable rates, recent declines, and significant increases aids in comprehending the geographical distribution of PD and its associated factors. Tailoring interventions based on these factors can promote positive health outcomes. Additionally, investigating declines in specific areas, such as La Rioja for men, provides crucial insights for effective targeted interventions. Conversely, examining increases in PD mortality reveals emerging risk factors and health disparities that require urgent attention to reduce the disease burden and improve health outcomes.
Pre-existing neurological conditions such as PD significantly impact COVID-19 severity and mortality.25 Despite the pandemic's impact on the general population, COVID-19 did not significantly affect mortality and hospitalisation rates among elderly patients with PD, according to a recent study.26 However, the pandemic did lead to notable increases in PD mortality in specific regions, as observed in recent studies.27,28 Our comprehensive study, which took place during the critical years of the COVID-19 pandemic, identified striking deviations from the typical PD mortality trends. These deviations are highlighted in Tables 1 and 2 and Fig. 1. Specifically, we observed notable shifts in certain areas, such as a reversal of rising mortality rates in men in La Rioja and an acceleration among women in Andalusia. The reasons for these regional disparities and the potential link to the pandemic remain to be elucidated.
Although our study provides valuable insights, it is important to acknowledge its limitations. Firstly, the use of death certificates as a source for acquiring mortality data may not be the ideal procedure for estimating the distribution of PD cases. However, it is worth noting that this method has been widely accepted as sufficiently accurate in Spain due to the homogeneity of the treatment, processing, and validation methods of the certificates throughout the country. This standardisation enables meaningful comparisons between different regions.29 Nevertheless, a major concern in PD research is the unreliable diagnoses leading to death, as PD is often underreported as an underlying cause of death on death certificates. In fact, in the NEDICES study,30 PD was registered as the underlying cause of death in only 14.6% of PD patients, indicating significant under-reporting. This under-reporting underscores the lack of awareness regarding the true impact of PD as a cause of death. To improve the accuracy of PD mortality data and address the issue of under-reporting, it is crucial to raise awareness among medical professionals and enhance their understanding of PD as a significant cause of death. Targeted education initiatives and continuing medical education programmes can play a vital role in achieving this goal.
Caution must also be exercised when interpreting our findings as causal relationships, as our study is descriptive in nature. This could lead to the ecological fallacy, wherein inferences about individuals are drawn from group-level data.
Despite these limitations, our study also has several strengths. Our rigorous approach employs a robust, evidence-based analysis that significantly contributes to the understanding of PD mortality trends in Spain.
One of the notable strengths of our study is the utilisation of the latest available mortality data and appropriate statistical methods to analyse trends over a span of 23 years. This comprehensive timeframe enabled us to identify significant changes in mortality rates and generate hypotheses regarding the factors contributing to these trends. Policymakers can leverage this information to effectively address the underlying causes of PD deaths.
Furthermore, the selection of the study period from 1999 to 2021 was carefully considered due to crucial advances made in PD research and management in Spain during this time. Significant improvements in disease identification and accurate mortality data were observed, thanks to the implementation of standardised diagnostic criteria. Additionally, the adoption of standardised treatment regimens and evidence-based management guidelines for PD led to notable impacts on healthcare practices and disease-related deaths. The use of the ICD-10 for mortality data ensured data consistency and comparability, further enhancing the reliability of our findings.
The future of PD management promises important advances in diagnostic and monitoring capabilities, with a focus on multidisciplinary approaches and innovative treatments. The incorporation of new technologies and biomarker studies will revolutionise PD management, enabling more accurate diagnosis, prognosis, and personalised therapies. Despite these improvements, the socioeconomic impact of the disease will still be significant in 2030, especially for patients in advanced stages.31
In conclusion, our findings underscore the significance of monitoring PD mortality trends and their varying impact across different regions and genders. This valuable information can play a crucial role in shaping future health policies and designing effective prevention strategies.
CRediT authorship contribution statementAll authors contributed to the conception and design of the study; the acquisition, analysis, and interpretation of data; drafting the manuscript and critically reviewing it for important intellectual content; approved the version to be published; and are responsible for all aspects of the study in ensuring that questions related to the accuracy or integrity of any part of the study are properly investigated and resolved.
Ethics statementBecause the data extracted from the Spanish National Statistics Institute were anonymised, following the principles of good clinical practice and the Declaration of Helsinki, the participants were not identified, and no personal information was accessed. Therefore, this study did not require patient consent or approval from the ethics committee (Spanish Law 14/2007, 3 July, on biomedical research [Spanish official State Gazette, 4 July 2007]) – PubMed, https://pubmed.ncbi.nlm.nih.gov/18201045/ (accessed 27 February 2023).
FundingThis research has not received specific support from public sector institutions, the commercial sector, or non-profit organisations.
Declaration of competing interestsThe authors declare no conflicts of interest concerning the content of this manuscript.