Migrants, a population vulnerable to communicable diseases, face multiple barriers in access to immunization programs. Individual studies suggest that they suffer immunization inequity compared to non-migrants, but the gap in vaccination has not been quantified. This systematic review assessed quantitatively the level of vaccination coverage among migrants, in comparison with non-migrants, collating the published literature.
MethodsReview protocol was prospectively registered (PROSPERO CRD42021228061). A literature search without language restrictions was conducted in PubMed, Scopus and Web of Science, from database inception to February 2021. This review included observational studies that provided the vaccination rates among migrant and non-migrant groups. Study quality was assessed using Newcastle-Ottawa scale. Data were synthesized pooling data from individual studies to generate summary odds ratio (OR) with 95% confidence interval (CI) using random effects model, assessing heterogeneity with I2 statistic and publication bias with funnel asymmetry analysis.
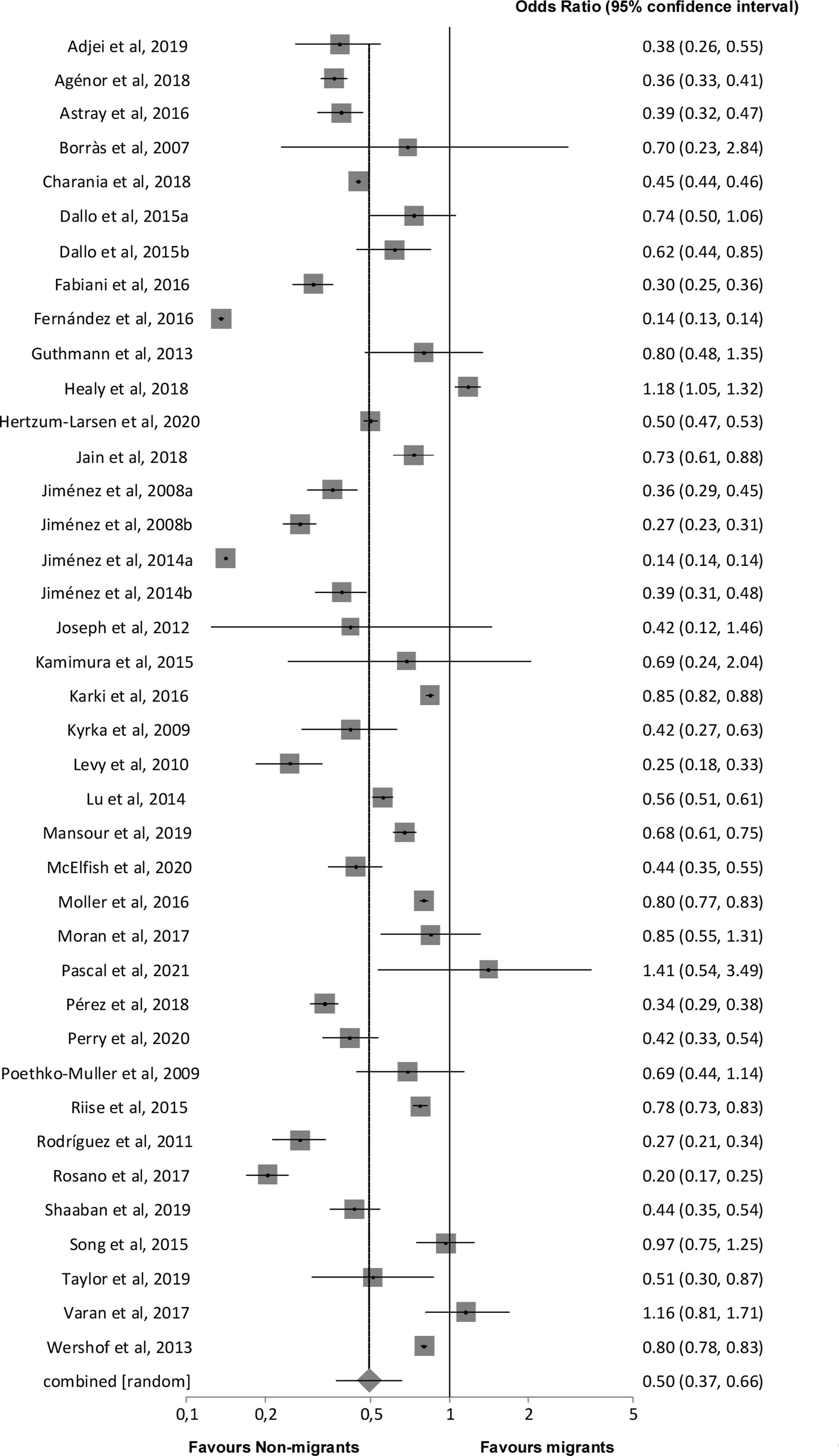
FindingsThere were 44 relevant studies (7,937,996 participants). Overall risk of bias was low in 13 (30%), moderate in 22 (50%) and high in 9 (20%) studies. Point estimates of individual ORs showed lower vaccination coverage among migrants in 36 of 39 meta-analyzable studies. Overall, the odds of vaccination coverage among migrants were lower compared to non-migrants (7,375,184 participants; summary OR 0.50; 95% CI 0.37–0.66; I2 99.9%). There was no funnel asymmetry.
InterpretationMigrants are half as often vaccinated compared to non-migrants. Public health prevention programs need to prioritize vaccination equity, not just to protect migrants but also to protect the host communities.
Los migrantes, una población vulnerable a enfermedades transmisibles, se enfrentan a múltiples barreras en el acceso a los programas de inmunización. Estudios individuales sugieren que este colectivo poblacional sufre desigualdad en la cobertura de inmunización, en comparación con población no migrante; sin embargo, hasta el momento no se ha cuantificado la brecha en la cobertura de vacunación. Esta revisión sistemática evaluó cuantitativamente el nivel de cobertura de vacunación entre los migrantes, en comparación con los no migrantes, recopilando la literatura publicada.
MétodosEl protocolo de revisión fue registrado prospectivamente (PROSPERO CRD42021228061). Se realizó una búsqueda de literatura sin restricciones de idioma en PubMed, Scopus y Web of Science, desde el inicio de las bases de datos hasta febrero de 2021. Esta revisión incluyó estudios observacionales que proporcionaran coberturas de vacunación entre grupos de migrantes y no migrantes. La calidad de los estudios se evaluó mediante la escala Newcastle-Ottawa. Los datos se sintetizaron y se extrajeron los valores de odds ratio (OR) e intervalo de confianza (IC) del 95%, utilizando un modelo de efectos aleatorios para cada uno de los estudios incluidos. Finalmente, se evaluó la heterogeneidad de los mismos con la prueba estadística de I2 y, el sesgo de publicación con el análisis de asimetría de embudo.
ResultadosHubo 44 estudios relevantes (7.937.996 participantes). El riesgo de sesgo fue bajo en 13 (30%), moderado en 22 (50%) y alto en nueve (20%) estudios. Las estimaciones puntuales de las OR individuales mostraron una menor cobertura de vacunación entre los migrantes en 36 de 39 estudios metaanalizables. En general, las probabilidades de cobertura de vacunación entre los migrantes fueron menores, en comparación con los no migrantes (7.375.184 participantes; OR resumen 0,50; IC 95%: 0,37-0,66; I2 99,9%). No hubo asimetría de embudo.
InterpretaciónLos migrantes se vacunan la mitad de veces que los no migrantes. Los programas de prevención en salud pública deben priorizar la equidad en la vacunación, no solo para proteger a los migrantes, sino también a las comunidades nativas de acogida.
The migratory phenomenon has increased considerably with approximately 272 million people residing outside their country of birth.1 Migrants may be relatively healthy upon arrival in a new country,2,3 but they tend to become vulnerable with a higher risk of contracting infectious diseases.4 Thus, they are considered a priority group for prevention and control.5–7 Access to health services is one of the challenges faced by migrants in their host countries.8–10 This is a particular issue with respect to immunization programs.1 In their countries of origin vaccination coverage may have been affected by factors such as interruption of immunization services,11 low socioeconomic status, and poor level of knowledge and awareness.10,12 Providing vaccination services to this vulnerable population is crucial, not just to protect migrants but also to protect the host communities.13
Previous systematic reviews have suggested that migrant groups generally experience lower immunization rates,13–15 but they have several limitations according to evidence synthesis quality assessment tools.16 One of the reviews14 applied language restrictions, risking overlooking relevant publications. Other reviews had geographical limitations, in one focusing on Europe13 and in another on three low-income and middle-income countries.15 A comprehensive systematic review of the worldwide literature is required.
Given the above background, the objective of this systematic review was to quantitatively determine the level of vaccination coverage among migrants compared to non-migrants, collating the published observational studies.
MethodsThe protocol of the systematic review was prospectively registered (registration number CRD42021228061; www.crd.york.ac.uk/PROSPERO). We followed MOOSE reporting guideline.17
Search strategy and study selectionBibliographic searches were carried out in PubMed, Scopus and Web of Science databases, without language or publication date restrictions from inception to February 2021. The search term combination was: ((vaccin*) OR (immuniz*) OR (immunis*)) AND ((coverage) OR (uptake) OR (access) OR (accept) OR (choice) OR (agreed)) AND ((migrant) OR (immigrant) OR (refugee) OR (asylum seeker*) OR (foreign born) OR (newcomer) OR (newcomer)) AND ((non-migrant) OR (indigenous) OR (native)) OR (locally born)). Reference lists of previous reviews were collated. All citations found were exported to Mendeley, where duplicates were removed.
Initially, the titles and abstracts of the articles were examined and those that met the following requirements were included: comparison of migrants with non-migrants, vaccination coverage for both groups, and observational study design. Studies without quantitative results were excluded. To address citations and articles published in languages other than English and Spanish we used translation by online means. One reviewer screened the titles and abstracts, and evaluated the full text of the articles to select studies to be included in the review. All study eligibility decisions were double checked by another reviewer and any disputes resolved by discussion or arbitration by the third reviewer.
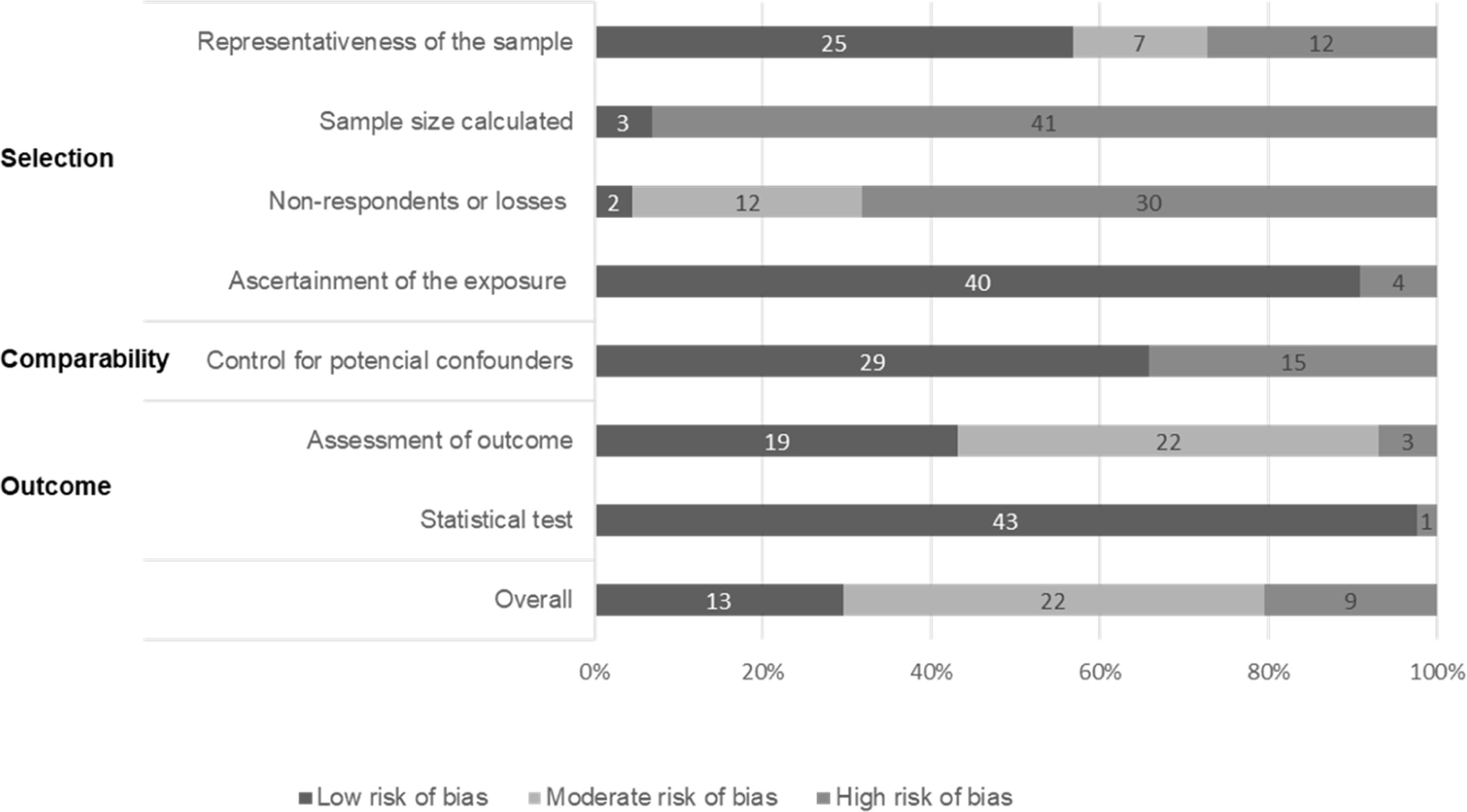
Data extraction and study quality assessmentData were extracted and the quality of the selected articles was assessed. The information extraction was recorded in Microsoft Excel, including the following parameters: Author, publication year, study year, location, study design, sample size, population and vaccine. Migrants were people who had moved from their country of birth to another country. Non-migrants were native or indigenous people of the host country. Some studies reported findings for several migrant groups. To assess risk of bias, quality of the studies was assessed with a modified Newcastle-Ottawa scale.18 The following quality aspects were evaluated: Selection (representativeness of the sample, sample size, non-respondents or losses and ascertainment of the exposure); comparability (control for potential confounders); and, outcome (assessment of outcome and statistical testing). Overall score was calculated ranging from 0 to10 points and classified for risk of bias as follows: low 7–10 points; moderate 5–6 points; and high 0–4 points. Studies were not excluded from the review on the basis of quality.
Data synthesisFrom the numerical data reported, we constructed 2×2 tables of vaccine coverage among migrants and non-migrants for each vaccine individually per study. The point estimates of all the crude odds ratios (OR) were plotted. From each study a single 2×2 table with the largest total sample, the largest number of doses, and the smallest difference in vaccine coverage was selected for meta-analysis to maximize precision and to produce the most conservative estimate of the association. Where data for more than one type of migrant groups were reported in a study, we used the most vulnerable group for comparison with non-migrants. We assessed heterogeneity using I2 statistic and applied random effects model for pooling results to generate summary OR with 95% confidence interval (CI).19 We assessed for publication and related biases using funnel asymmetry analysis.20
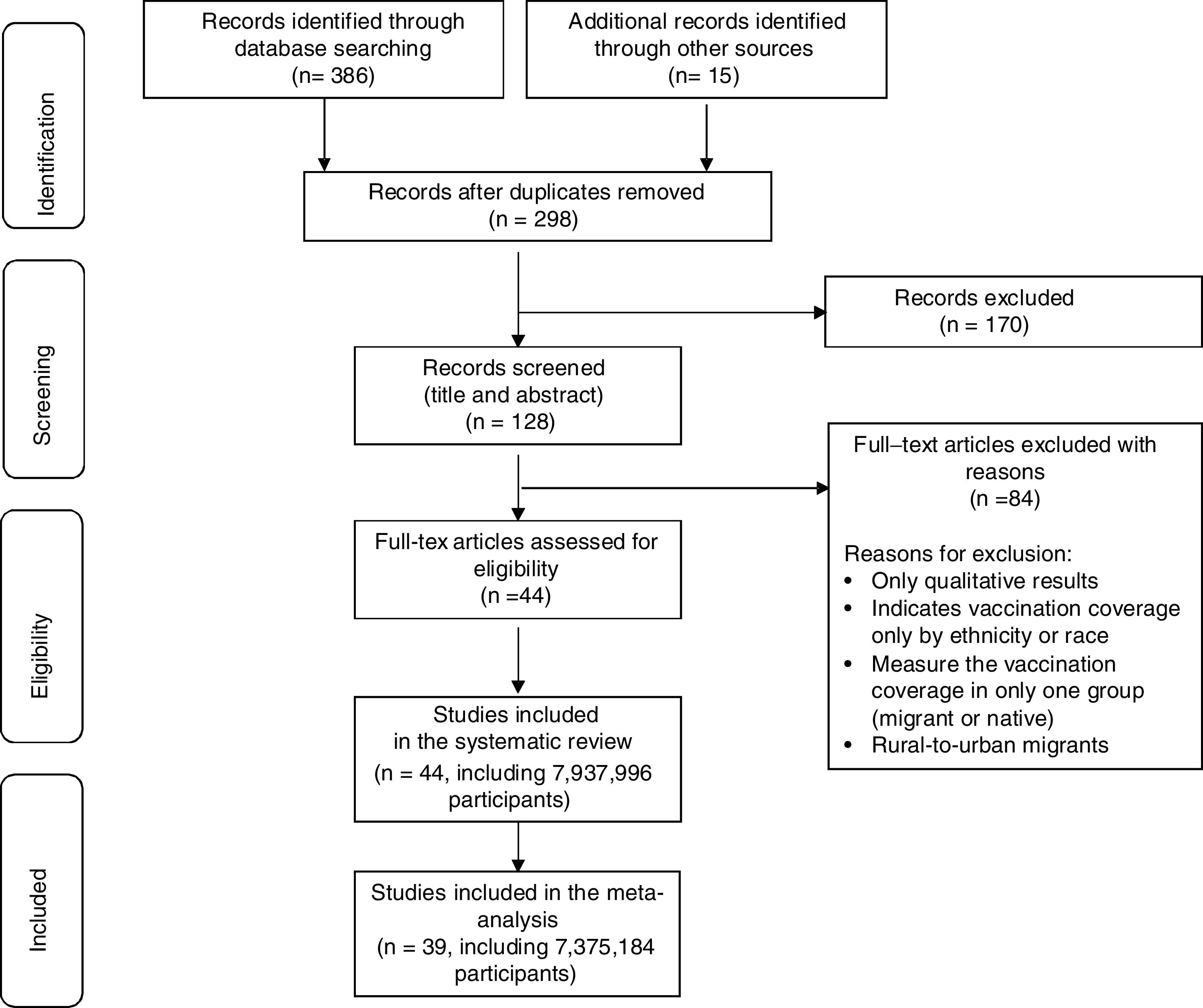
ResultsThe search yielded 401 citations. After removal of duplicates, 298 citations remained for title and abstract screening. We excluded 170 citations that did not meet the selection criteria, leaving 128 studies for review of full-text articles. Forty-four studies with 7,937,996 participants were eligible (Fig. 1).
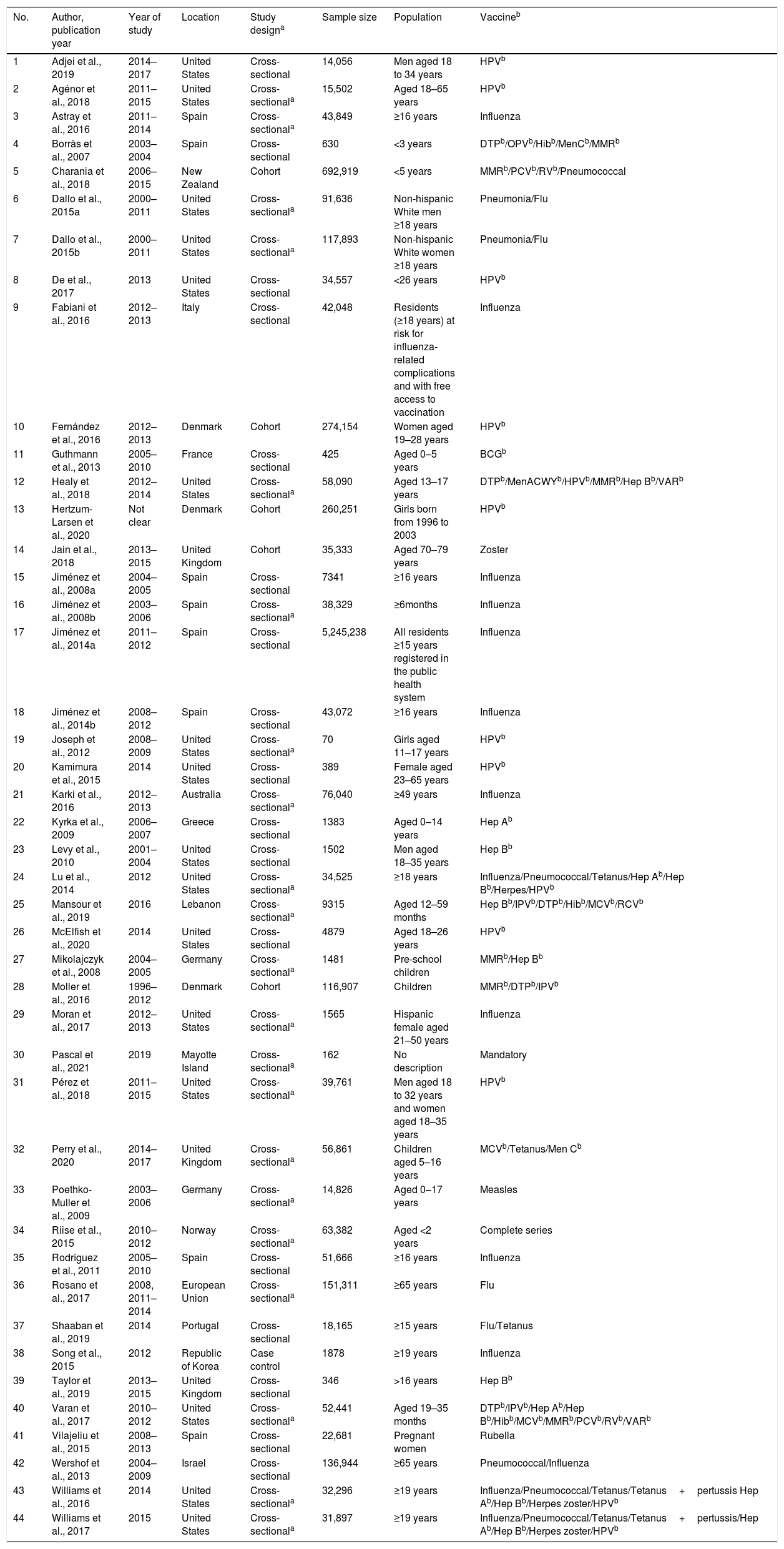
Study characteristics and qualityThe study characteristics are given in Table 1. Of the 44 studies, 16 (36%) were from the USA, 8 (18%) from Spain, 3 (7%) from the UK, 3 (7%) from Denmark, 2 (5%) from Germany and the rest were conducted in Australia, Israel, Italy, Lebanon, Mayotte Island, New Zealand, Portugal, Norway, Republic of Korea, France, Greece and European Union. Thirty-eight studies (87%) were cross-sectional, five (11%) were cohort and one (2%) was a case-control in design. Sample sizes ranged from 70 to 5,245,238 participants. Fig. 2 and Appendix 1 show study quality details. Overall risk of bias was low in 13 (30%), moderate in 22 (50%) and high in 9 (20%) studies.
Characteristics of studies included in the review of vaccination coverage among migrants.
| No. | Author, publication year | Year of study | Location | Study designa | Sample size | Population | Vaccineb |
|---|---|---|---|---|---|---|---|
| 1 | Adjei et al., 2019 | 2014–2017 | United States | Cross-sectional | 14,056 | Men aged 18 to 34 years | HPVb |
| 2 | Agénor et al., 2018 | 2011–2015 | United States | Cross-sectionala | 15,502 | Aged 18–65 years | HPVb |
| 3 | Astray et al., 2016 | 2011–2014 | Spain | Cross-sectionala | 43,849 | ≥16 years | Influenza |
| 4 | Borràs et al., 2007 | 2003–2004 | Spain | Cross-sectional | 630 | <3 years | DTPb/OPVb/Hibb/MenCb/MMRb |
| 5 | Charania et al., 2018 | 2006–2015 | New Zealand | Cohort | 692,919 | <5 years | MMRb/PCVb/RVb/Pneumococcal |
| 6 | Dallo et al., 2015a | 2000–2011 | United States | Cross-sectionala | 91,636 | Non-hispanic White men ≥18 years | Pneumonia/Flu |
| 7 | Dallo et al., 2015b | 2000–2011 | United States | Cross-sectionala | 117,893 | Non-hispanic White women ≥18 years | Pneumonia/Flu |
| 8 | De et al., 2017 | 2013 | United States | Cross-sectional | 34,557 | <26 years | HPVb |
| 9 | Fabiani et al., 2016 | 2012–2013 | Italy | Cross-sectional | 42,048 | Residents (≥18 years) at risk for influenza-related complications and with free access to vaccination | Influenza |
| 10 | Fernández et al., 2016 | 2012–2013 | Denmark | Cohort | 274,154 | Women aged 19–28 years | HPVb |
| 11 | Guthmann et al., 2013 | 2005–2010 | France | Cross-sectional | 425 | Aged 0–5 years | BCGb |
| 12 | Healy et al., 2018 | 2012–2014 | United States | Cross-sectionala | 58,090 | Aged 13–17 years | DTPb/MenACWYb/HPVb/MMRb/Hep Bb/VARb |
| 13 | Hertzum-Larsen et al., 2020 | Not clear | Denmark | Cohort | 260,251 | Girls born from 1996 to 2003 | HPVb |
| 14 | Jain et al., 2018 | 2013–2015 | United Kingdom | Cohort | 35,333 | Aged 70–79 years | Zoster |
| 15 | Jiménez et al., 2008a | 2004–2005 | Spain | Cross-sectional | 7341 | ≥16 years | Influenza |
| 16 | Jiménez et al., 2008b | 2003–2006 | Spain | Cross-sectionala | 38,329 | ≥6months | Influenza |
| 17 | Jiménez et al., 2014a | 2011–2012 | Spain | Cross-sectional | 5,245,238 | All residents ≥15 years registered in the public health system | Influenza |
| 18 | Jiménez et al., 2014b | 2008–2012 | Spain | Cross-sectional | 43,072 | ≥16 years | Influenza |
| 19 | Joseph et al., 2012 | 2008–2009 | United States | Cross-sectionala | 70 | Girls aged 11–17 years | HPVb |
| 20 | Kamimura et al., 2015 | 2014 | United States | Cross-sectional | 389 | Female aged 23–65 years | HPVb |
| 21 | Karki et al., 2016 | 2012–2013 | Australia | Cross-sectionala | 76,040 | ≥49 years | Influenza |
| 22 | Kyrka et al., 2009 | 2006–2007 | Greece | Cross-sectional | 1383 | Aged 0–14 years | Hep Ab |
| 23 | Levy et al., 2010 | 2001–2004 | United States | Cross-sectional | 1502 | Men aged 18–35 years | Hep Bb |
| 24 | Lu et al., 2014 | 2012 | United States | Cross-sectionala | 34,525 | ≥18 years | Influenza/Pneumococcal/Tetanus/Hep Ab/Hep Bb/Herpes/HPVb |
| 25 | Mansour et al., 2019 | 2016 | Lebanon | Cross-sectionala | 9315 | Aged 12–59 months | Hep Bb/IPVb/DTPb/Hibb/MCVb/RCVb |
| 26 | McElfish et al., 2020 | 2014 | United States | Cross-sectional | 4879 | Aged 18–26 years | HPVb |
| 27 | Mikolajczyk et al., 2008 | 2004–2005 | Germany | Cross-sectionala | 1481 | Pre-school children | MMRb/Hep Bb |
| 28 | Moller et al., 2016 | 1996–2012 | Denmark | Cohort | 116,907 | Children | MMRb/DTPb/IPVb |
| 29 | Moran et al., 2017 | 2012–2013 | United States | Cross-sectionala | 1565 | Hispanic female aged 21–50 years | Influenza |
| 30 | Pascal et al., 2021 | 2019 | Mayotte Island | Cross-sectionala | 162 | No description | Mandatory |
| 31 | Pérez et al., 2018 | 2011–2015 | United States | Cross-sectionala | 39,761 | Men aged 18 to 32 years and women aged 18–35 years | HPVb |
| 32 | Perry et al., 2020 | 2014–2017 | United Kingdom | Cross-sectionala | 56,861 | Children aged 5–16 years | MCVb/Tetanus/Men Cb |
| 33 | Poethko-Muller et al., 2009 | 2003–2006 | Germany | Cross-sectionala | 14,826 | Aged 0–17 years | Measles |
| 34 | Riise et al., 2015 | 2010–2012 | Norway | Cross-sectionala | 63,382 | Aged <2 years | Complete series |
| 35 | Rodríguez et al., 2011 | 2005–2010 | Spain | Cross-sectional | 51,666 | ≥16 years | Influenza |
| 36 | Rosano et al., 2017 | 2008, 2011–2014 | European Union | Cross-sectionala | 151,311 | ≥65 years | Flu |
| 37 | Shaaban et al., 2019 | 2014 | Portugal | Cross-sectional | 18,165 | ≥15 years | Flu/Tetanus |
| 38 | Song et al., 2015 | 2012 | Republic of Korea | Case control | 1878 | ≥19 years | Influenza |
| 39 | Taylor et al., 2019 | 2013–2015 | United Kingdom | Cross-sectional | 346 | >16 years | Hep Bb |
| 40 | Varan et al., 2017 | 2010–2012 | United States | Cross-sectionala | 52,441 | Aged 19–35 months | DTPb/IPVb/Hep Ab/Hep Bb/Hibb/MCVb/MMRb/PCVb/RVb/VARb |
| 41 | Vilajeliu et al., 2015 | 2008–2013 | Spain | Cross-sectional | 22,681 | Pregnant women | Rubella |
| 42 | Wershof et al., 2013 | 2004–2009 | Israel | Cross-sectional | 136,944 | ≥65 years | Pneumococcal/Influenza |
| 43 | Williams et al., 2016 | 2014 | United States | Cross-sectionala | 32,296 | ≥19 years | Influenza/Pneumococcal/Tetanus/Tetanus+pertussis Hep Ab/Hep Bb/Herpes zoster/HPVb |
| 44 | Williams et al., 2017 | 2015 | United States | Cross-sectionala | 31,897 | ≥19 years | Influenza/Pneumococcal/Tetanus/Tetanus+pertussis/Hep Ab/Hep Bb/Herpes zoster/HPVb |
a Studies without reporting of specific design; design assigned by reviewers.
HPV: human papillomavirus vaccine. DPT: diphtheria–tetanus–pertussis vaccine. OPV: trivalent oral polio vaccine. Hib: hemophilus influenzae type b. Men C: meningococcal serogroup C vaccine. MMR: measles–mumps–rubella. PCV: pertussis-containing vaccine. RV: rotavirus vaccine. BCG: Bacillus Calmette–Guérin vaccine. MenACWY: quadrivalent meningococcal conjugate vaccine. Hep B: hepatitis B. VAR: varicella vaccine. Hep A: hepatitis A. IPV: poliovirus vaccine. MCV: measles vaccine. RCV: rubella-containing vaccine.
Five articles did not have enough information to construct the 2×2 table (Fig. 1). Appendix 2 contains the details of the data tables. The meta-analysis was based on 39 studies. Together these studies comprised data on a total of 7,375,184 participants of whom 6,449,102 (87%) were non-migrants and 926,082 (13%) were migrants. Point estimates of individual ORs showed lower vaccination coverage among migrants in 36 studies as shown in the forest plot in Fig. 3. The meta-analysis produced a summary OR of 0.50 (95% CI: 0.37–0.66). There was a high level of heterogeneity with an I2 value of 99.9% (chi-square test for heterogeneity X2=22.96, df=1, P<0.0001). Appendix 4 shows the funnel plot, where there was no funnel asymmetry (Egger's test P=0.0511).
DiscussionThis meta-analysis, the first of its kind to our knowledge, quantified the relationship between vaccination coverage and migration status. The quality of the included studies was diverse, predominantly moderate. A wide range of vaccinations were covered in the included studies. High level of heterogeneity was found in the pooled results, though the majority of the studies showed lower vaccination coverage among migrants. This is probably related to the different vaccination policies among the countries included in the review. Our findings showed that migrants were half as often vaccinated compared to non-migrants, so vaccination coverage related to migrant status should be an important public health issue. This is crucial for the current vaccination campaign in the coronavirus pandemic era worldwide.
This systematic review and meta-analysis followed a robust methodology so as to attempt to reduce the possibility of various forms of errors and biases. The global search without language and date restrictions yielded sufficient numbers of studies with a high number of participants to facilitate precise estimation of the association. Although contact with authors or migrant organizations may have led to further information, the summary result was reliable with narrow confidence interval. However, one perceived limitation of this study may be related to the fact that there is no universally accepted definition of a migrant at the international level. The lack of clarity about this general term leaves the interpretation somewhat open, generating issues in generalizability of our findings. With respect to the observed heterogeneity, it's possible that legal migrants as well as some specific ethnic or racial groups may have been over-represented in the exposure group. However, the heterogeneity observed represented differences in size of the association with migratory status rather than differences in direction of the association. This type of heterogeneity may be unavoidable, and given the large size of association our observation merits careful consideration. Regarding the designs included, the studies were largely cross-sectional self-report surveys, which may have been susceptible to nonresponse bias and recall bias.22 There is no standardized way to measure the vaccination coverage, and medical records reviews may be more accurate. Self-reported coverage may overestimate the coverage of vaccination records,23 and validity of the comparisons may be affected by sociodemographic variables such as age, gender or migratory status.21 In case of differential reporting related to migratory status, there is a risk of bias in the observed findings. However, in our view, the size of the summary result obtained and its precision provides protection against a spurious conclusion.
The results of our meta-analysis are in accordance generally with the previously published narrative reviews.13–15 Moreover, we were able to quantify the extent to which migrant groups experience lower immunization rates than native-born groups in the evidence collated without geographic restriction. Thus our review provides the current best quantitative evidence synthesis, and it underpins the needs for public health prevention programs to prioritize vaccination equity. In addition, health workers must develop skills and knowledge for the care of immigrants, in order to successfully face the cultural, language and medical differences of this population.24 At this time as we vaccinate against coronavirus, immunization program planning needs to focus on vaccinating migrants, something that will be crucial for the benefit of the entire population.13
In conclusion, migrants are significantly less often vaccinated compared to non-migrants, and public health prevention programs need to prioritize vaccination equity.
ContributorsAll authors contributed in the conception of the research question and designed the study. MR did the literature search, study selection and data extraction, and double checked by NC. MR and KK did the statistical analysis. The figures, tables and appendices were designed by MR and KK. All authors contributed to the drafts and final version of the manuscript.
FundingNo source of funding.
Conflict of interestAll other authors declare no conflict of interest.
KSK is Distinguished Investigator at University of Granada funded by the Beatriz Galindo (senior modality) Program of the Spanish Ministry of Education.