We retrospectively reviewed a case of a 42-year-old woman with intravenous leiomyomatosis.
Clinical findingsThe present study describes a case of IVL extending into the right internal and common iliac veins.
DiagnosisThe patient was diagnosed by definitive pathological examination after a hysterectomy and double salpingectomy. Hypovolaemic shock due to delayed intraperitoneal bleeding from the ovarian vessels pedicle was observed. An emergent laparotomy for haemostasis was performed. A follow-up MRI, 2 months later, showed a polylobulated mass extending inside the right internal and common iliac veins.
Intervention and resultThe patient underwent a third laparotomic procedure with the removal of the right pelvic mass together with the involved veins. The postoperative course was uneventful, and the patient remains well at 3-month follow-up, with no signs of lower limb edema or venous disorders.
ConclusionIntracardiac leiomyomatosis is mostly diagnosed in premenopausal women. The most severe manifestation could be a vascular thrombosis or a right atrial tumor in the case of intracardiac involvement. Early and appropriate diagnosis is essential for optimal treatment. Surgery is the best treatment.
Presentamos el caso de una paciente de 42 años con leiomiomatosis intravenosa.
Hallazgos clínicosEl estudio presente describe un caso de IVL con afectación de las venas ilíaca común e interna derecha.
DiagnósticoLa paciente fue diagnosticada mediante el examen histológico definitivo tras una histerectomía total con doble salpingectomía. Se objetivó un shock hipovolémico por sangrado intraperitoneal tardío del pedículo de vasos ováricos. Se realizó una laparotomía urgente para hemostasia. Una RMN durante el seguimiento, 2 meses después, mostró una masa polilobulada con afectación de la vena ilíaca común y la vena ilíaca interna derecha.
Intervención y resultadoA la paciente se le realizó una tercera laparotomía con la extirpación de la masa pélvica derecha. El curso postoperatorio fue satisfactorio y la paciente permaneció asintomática a los 3 meses de seguimiento, sin signos de edema en extremidades inferiores ni otras afectaciones vasculares.
ConclusiónLa leiomiomatosis intracardíaca se diagnostica más frecuentemente en mujeres premenopáusicas. La forma de manifestación más severa sería una trombosis vascular o un tumor intracardíaco en la aurícula derecha, en el caso de afectación intracardíaca. Un diagnóstico precoz es esencial para un tratamiento óptimo. La cirugía es el mejor tratamiento.
Uterine leiomyomas are benign tumors originated from uterine smooth muscle cells. Their incidence moves from 50 to 70% of women.1 The known risk factors for leiomyomatosis are obesity, nulliparity and black race; while the use of oral contraceptive pill act as a protective factor.2
Most leiomyomas are asymptomatic however some can be symptomatic by causing hypermenorrhea (30%), pelvic pain or compressive symptoms (34%), infertility (27%) and recurrence pregnancy lost (3%).3
There exist a rare histological variety called intravascular leiomyomatosis (IVL). IVL is a uterine benign tumor that grows from smooth muscle veins cells and that has a characteristic intravascular growth.4
The incidence of IVL is very low, up to 2018 only 300 cases had been reported.5 IVL has a peculiarity endovascular invasion of myometrial vases which gives its harmful behavior.6 IVL has 2 different accesses to the systemic vascular system: the primary one through uterine vein and the secondary through ovarian vein.7 IVL can cause vascular collapse by extending across inferior vena cava, right cardiac cameras and pulmonary artery. The extension of IVL to the heart is known as Intracardiac leiomyomatosis (ICL).8,9 ICL can cause heart block and death.10,11
IVL typically appears in premenopausal woman aged between 28 and 80 years (average 45 years). Usually, patients with IVL, presents with a history of uterine myomas or hysterectomy.12 Gene recoding in chromosomes 12 and 14 [t (12; 14) (q15; q24)] and hyperexposure to estrogens can have an important role in the development of IVL.
In this paper we describe a case report of a patient diagnosed and treated for IVL and is also presented a bibliography review about it.
Patient informationA nulliparous 42-year-old woman, was admitted with abdominal distention due to a fast growing abdominal mass.
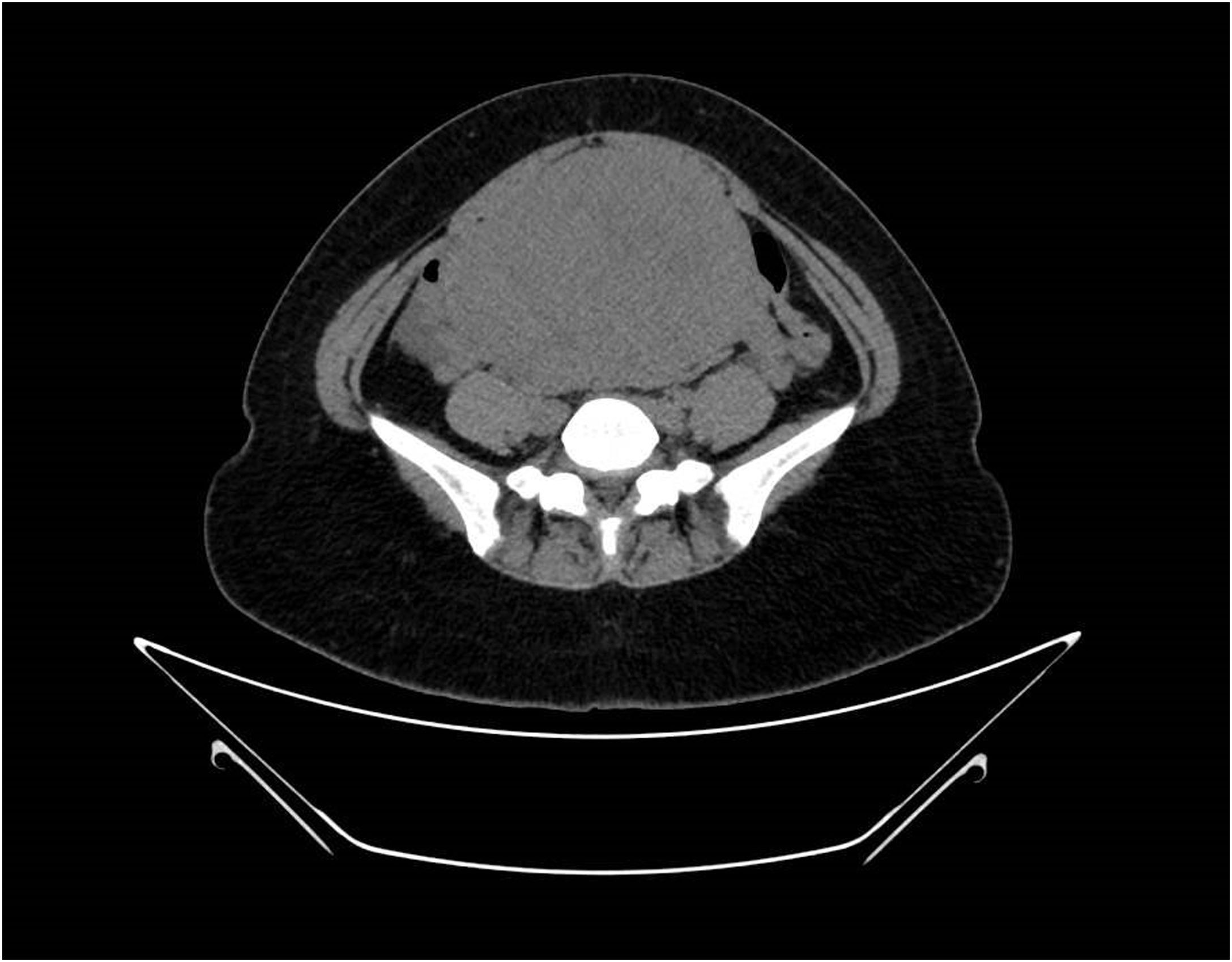
Clinical findingsGynecological ultrasound and Pelvic Magnetic Resonance revealed a huge tumor of about 15cm×10cm×17cm with a very clear boundary and highly vascularized consistent with myoma without malignancy signs. The study was completed with a Computed Tomography (CT) scan that confirmed the ultrasound and pelvic resonance findings. The mass generates an important collapse of the distal cava vein. Pelvic ovarian and hypogastric arteries seem to be dilated. No distant malignant masses are found.
Therapeutic interventionThe patient underwent a hysterectomy with double salpingectomy by laparotomy. During the operation, huge myomas were seen along the broad ligament. The postoperative course was complicated with a hypovolemic shock due to a delayed intraperitoneal bleeding from the ovarian vessels pedicle that led to an emergent laparotomy for haemostasis. The definitive pathological examination of the specimen showed typical leiomyomas with no atypia, coagulative tumor cell necrosis and scarce mitosis. A noticeable presence of mature smooth muscle growing inside the lumen of uterine and pelvic veins led to diagnosis of IVL.
The patient remained asymptomatic but a follow-up MRI, 2 months later, showed a polylobulated 84mm×48mm×35mm mass extending inside the right internal and common iliac veins. The tumor was isointense on T1-weighted imaging, with no restricted-diffusion pattern. Under the diagnosis of early relapse or progression of a previously missed intravascular leiomyoma the patient underwent a third laparotomic procedure with the removal of the right pelvic mass altogheter with the involved veins. Under heparin anticoagulation, the procedure involved the isolation of the mass with a careful dissection and ligation of the terminal branches of the right internal iliac vein, and the external iliac vein for the in-block resection of the tumor. The right common iliac vein was skletonized and proximally clamped to allow a safe removal by expression of the remaining tumor remaining in their lumen.
Follow-up and resultThe postoperative course was uneventful and the patient remains well at 3 months follow-up, with no signs of lower limb edema or venous disorders. The final pathology was consistent with IVL and no signs of malignancy were found.
DiscussionIVL is a weird situation and the diagnosis before the surgery is extremely difficult to make inearly stages when it is usually asymptomatic, causing just cause myoma-like symptoms. Pre-chirurgical diagnosis of intravascular myometrial growth is a big challenge, almost infeasible at initial stages.
At advanced stages, because of its extension to big vessels, the manifestations are more severe and then diagnose is easier.
Most patients (72%) diagnosed of IVL present a big pelvic mass (>20cm),13 and the most frequent localization is intra-ligamentary (77%).14 LMIV should be included as differential diagnosis in patients with gigantic myomas with intraligamentary growing.
Our patient developed IVL only 2 months after the hysterectomy, but usually it will take from 6 months to 20 years to develop it, as described by Harris et al.15
Ultrasound is the imaging technique more used to evaluate uterine masses, but it will not help to detect IVL at initial stages. In patients with cardiac involvement the echocardiography is the most sensitive technique. Computed Tomography, Arterial Computed Tomography, Magnetic Resonance are useful to evaluate the spread of the IVL and better plan the surgery (Figs. 1–3).
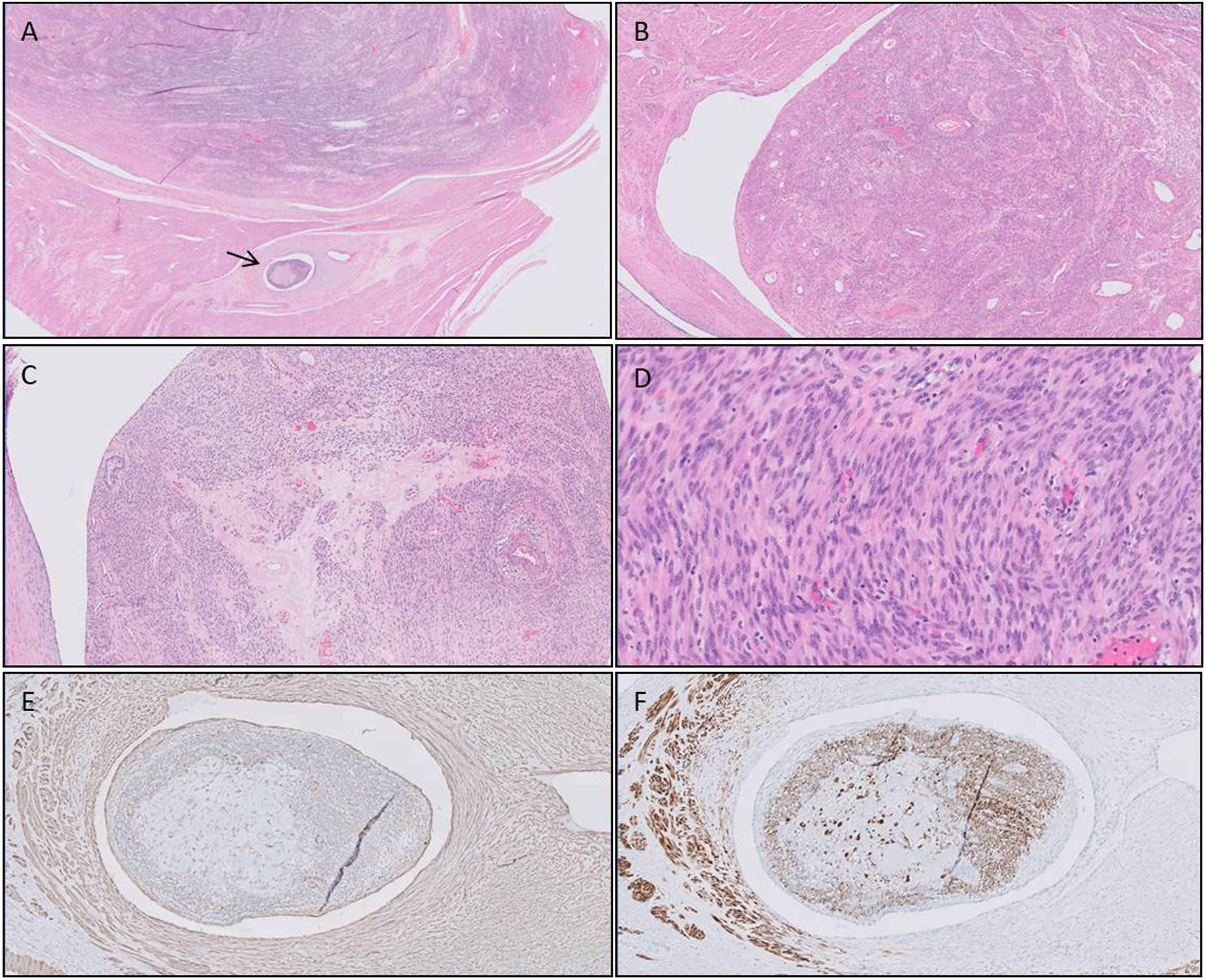
Pathological study of the surgical specimen. Hematoxylin–eosin staining. The arrow indicates the focal intravascular invasion of uterine leiomyomatosis. A: Hematoxylin–eosin staining (HE) (10×). Uterine leiomyomatosis showing focal vascular invasion (arrow). B: HE (20×). Venous wall with non atypical spindle cell growth in the lumen, resembling an ordinary leiomyoma. C: HE (50×). Intravascular smooth muscle with numerous thick-walled vessels, fibrosis and hialinization. D: HE (200×) Elongated spindle cells without atypia or necrosis and scarce mitotic activity. E, F: Positive immunostain for smooth muscle cells. E, actina (100×). F, desmina (100×).
Surgery is the best treatment for IVL. It can be practiced in a unique surgical act or in different surgical steps (according to patient tolerance, surgery required, the anatomy and the stretch of IVL).16,17
Because of overexpression of estrogen and progesterone receptors bilateral annexectomy is always recommended. Medical treatment is controversial, nevertheless GnRH analogs can help reduce the size of IVL. Other treatments such hast tamoxifene or medroxyprogesterone have not demonstrated benefit.18
The high recurrence rate after surgery (about 30%) makes it essential to carry out strict and close long-term follow up.19 The main factors that determinate the appearance of relapse are: early age of women at diagnosis, the initial size of the tumor, and the complete or incomplete surgical exeresis.20
We can conclude that ICL is an odd reality that will be mostly diagnosed in premenopausal women. The most severe form of manifestation could be a vascular thrombosis or a right auricular tumor in case of intracardiac involvement. Early and appropriate diagnosis is essential for an optimal treatment. Surgery will be the mean therapy than can be offered.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Informed consentThe authors declare that they have the informed consent of the patient.
FundingNo finance was received.
Conflict of interestThe author declares no interest conflict.