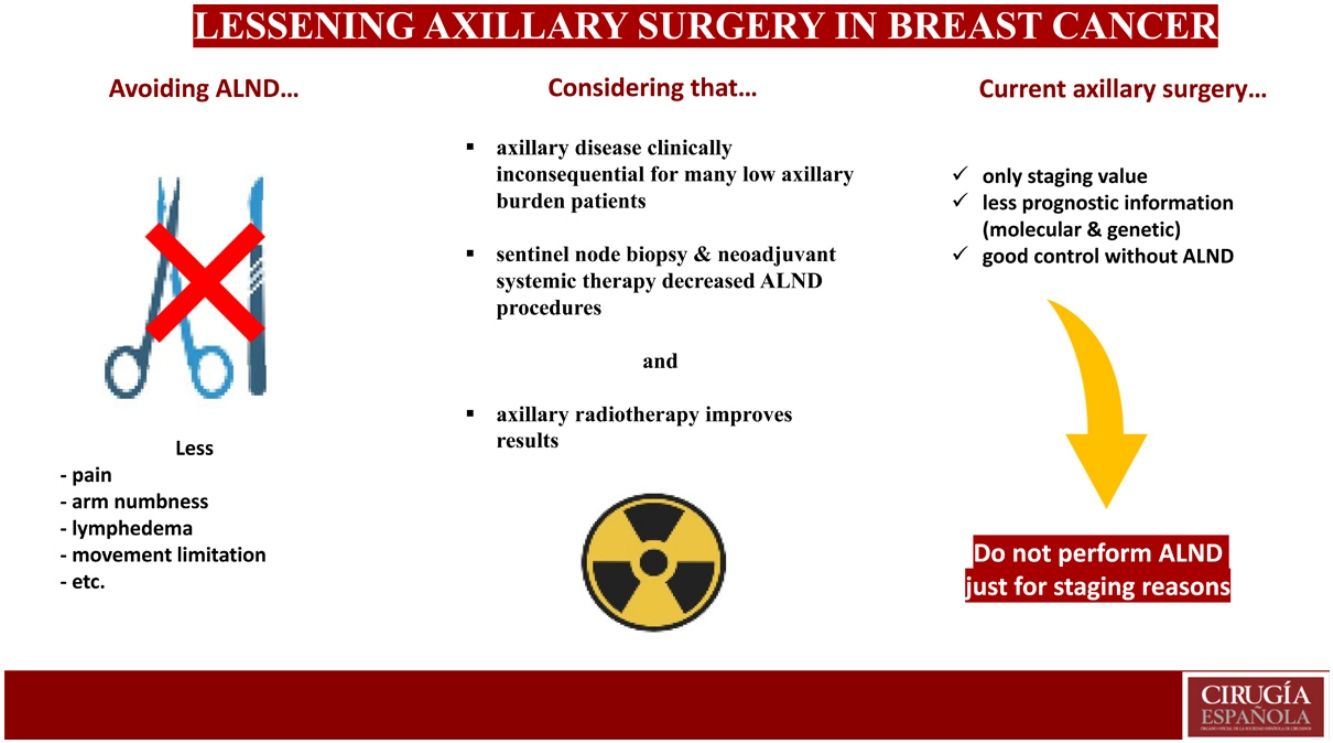
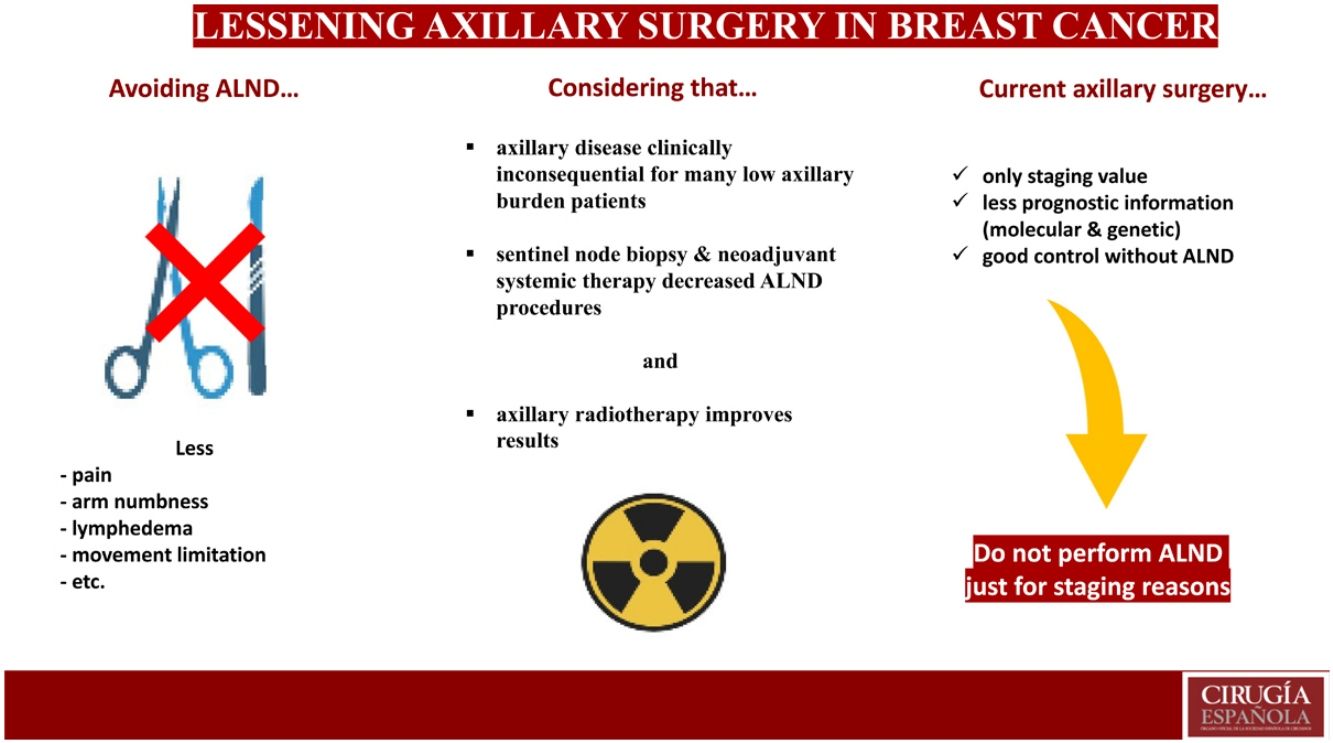
This article provides a brief account of the recent evolution of the highly controversial surgical management of the positive axilla in patients with breast cancer, an issue still open to disparate surgical procedures. This short review highlights the reports that supply the rationale for current trends in reducing the aggressiveness of this surgery and discusses the course of the trials still in progress pointing in the same direction, thus supporting the principle of not performing axillary lymph node dissection for staging purposes alone.
Este artículo es un breve resumen de la reciente evolución del controvertido tratamiento quirúrgico de la axila en pacientes con cáncer de mama, que sigue estando abierto a procedimientos quirúrgicos demasiado dispares. Esta corta revisión destaca las publicaciones que constituyen la base lógica de las tendencias actuales hacia la reducción de la agresividad quirúrgica y recalca los ensayos clínicos aún en progreso apuntando en esta misma dirección, apoyando así el principio de evitar la linfadenectomía axilar solo por razones de estadiaje.
For more than a century, axillary lymph node dissection (ALND) associated with breast cancer has caused high morbidity (overall, 70%).1 Pain, reduced arm motion, lymphedema, paresthesia (ranges: 27.5%–40%, 24%–29.8%, 3.5%–42% and 10.9%–63.2%, respectively), etc., have plagued thousands of patients, motivating healthcare professionals involved in the treatment of this disease to explore their mitigation.2–6 Since the 1990s, publications about the endoscopic axillary approach (with or without liposuction) have described advantages over the open technique (mainly, less postoperative pain) as well as certain drawbacks (e.g., a small number of port-site recurrences); as a result, the technique has not yet gained wide acceptance.7–9 ALND based on breast lymphatics level, called axillary reversed mapping, is a more recent technique also aimed at reducing the extent and morbidity of the procedure.10,11
Several assays including low-risk patient groups with absent palpable lymph nodes (i.e., low axillary nodal burden) have provided insight on axillary management by comparing ALND versus no axillary surgery. The NSABP-04, INT09/98, IBCSG 10–93 and AXIL95 Group trials, as well as other essays,12–17 have found no difference in disease-free or overall survival between these treatments, while also proving that axillary disease is clinically inconsequential in around half of these patients, even without adjuvant treatment. Adding systemic therapy and axillary radiotherapy was even able to further reduce the axillary recurrence rate to 1%.12,14,17
Sentinel lymph node biopsy (SLNB), although not free of morbidity,2 was the first of these great steps in the de-escalation of surgical aggressiveness. The NSABP B-32 trial showed that SLNB minimized the side effects of ALND, offering equivalent overall and disease-free survival rates and regional control.18 Initially, SLNB was indicated for cT1–3 N0 disease and ductal carcinoma in situ (DCIS) with suspicion of invasion or requiring mastectomy, but these indications rapidly expanded. SLNB may be considered in cases of multifocal or multicentric disease, prior breast or axillary surgery and pregnancy. The ACOSOG-Z0001 trial proved that ALND could be safely omitted in patients with fewer than 3 positive sentinel lymph nodes (SLN) (given a clinically negative axilla), breast tumor smaller than 5 cm, breast-conserving surgery (BCS) with whole-breast radiotherapy, and adjuvant treatment with hormone therapy or chemotherapy.19 These conditions for omitting ALND were later extended to SLN with micrometastases or isolated tumor cells,20 mastectomy for infiltrating cancer (including T4a-c), if axillary radiation is to be administered,21–24 and to the microscopic extracapsular extension of the SLN.15 SLNB is also feasible for patients with invasive local recurrence after BCS presenting with cN0, although the clinical significance of its results are not clear.21 In cases of positive axilla and ER+/PR+/HER2− tumor subtype (which have a low probability of response after neoadjuvant systemic therapy [NST]), primary surgery and SLNB with 1–2 positive nodes may avoid ALND. Furthermore, there seems to be no significant differences in outcome between patients with fewer than 3 positive macrometastases in SLNB receiving axillary radiotherapy compared to those with ALND, regardless of their immunohistochemical subtype or menopausal status.25–27
Currently, certain conditions have been accepted by several guidelines to omit axillary staging, including: cases in which staging will not change adjuvant therapy, pure DCIS with breast-conserving surgery, patients over the age of 70 years with hormone receptor positive T1–2 N0 tumors, prophylactic mastectomy, malignant phyllodes tumor and primary breast sarcoma.20
More recently, one more step has been provided by the increased use of NST, which can convert pN1 patients to clinically negative axillary disease (ycN0) in 41%–74% of patients.28–30 In these ypN0 patients, avoidance of ALND has been accepted by using SLNB with dual tracer and the retrieval of more than 2 negative SLN, by the retrieval of the pre-NST marked node alone (target lymph node biopsy or TLNB), or by the retrieval of the TLN with at least 2 SLN (targeted axillary dissection [TAD]). The false negative rates (FNR) of these techniques are below the consensus threshold of 10%, with TAD showing the lowest figures.31,32 Again, micrometastases and isolated tumor cells in these nodes, even after NST, do not lead to ALND whenever axillary radiotherapy is to be administered.24 To complicate matters, the need for adjuvant axillary radiotherapy for patients with a pathological complete response on SLNB or TAD is still debatable. Since the marked node is almost systematically affected in all patients who remain N positive after NST,33 the biopsy only of this node could be enough for axillary staging, with a higher FNR than TAD but still less than 10%.34
Nevertheless, even these 2 latter techniques aimed at reducing axillary aggressiveness in initially N1 patients remain controversial, since SLNB alone could lead to the same clinical results of low regional recurrence.35–37 Thus, reducing the FNR may have minimal clinical significance as the axillary recurrence rates of N1 patients undergoing SLNB are less than 2% in some long-term follow-up reports of randomized trials, observing no significant differences compared to N0 patients.38–40 In other words, false-negative SLNB does not result in regional recurrence for most patients, as occurs in patients with initial surgery.
In addition, the role of the axillary status to define disease treatment has been further limited by using information provided by the biological and genetic characteristics of the tumor cells from immunohistochemistry staining and genomics platforms in the management of invasive breast cancer. HER2-positive and triple-negative patients with tumors of a certain size are treated with neoadjuvant chemotherapy and biological therapies, regardless of their axillary extension, as adjuvant treatment is administered to patients showing a high risk of recurrence in the genetic profile of their tumors, not according to the axillary involvement.41
Notwithstanding these advances, indications for ALND, though less extensive, are still significant: patients with cN2–3 at presentation (although treatment of the negative axilla is unclear), cN0 patients with 3 or more positive SLNB,19,22,23 failed SLNB detection in high-risk patients (high grade, lymphovascular invasion, cT3–4, HER2 positive or triple negative tumors, multifocal/multicenter disease, premenopausal), N-positive patients unfit for NST or those who remain positive after the treatment (including occult breast cancer), inflammatory breast cancer, axillary recurrence and positive axilla in invasive local recurrence.
In the pursuit of further reduction of axillary dissection, many trials are underway. The A011202/MAC19 trial randomizes patients who are SLNB positive after NAC to ALND vs no further axillary surgery, then administering axillary radiotherapy to all patients.42 The SOUND (Sentinel Node versus Observation after Axillary Ultrasound), NAUTILUS, INSEMA (Intergroup-Sentinel-Mamma) and the BOOG 2013–08 trials43–46 seek to determine whether SLNB can be avoided in cN0 patients. The TAXIS trial (Tailored Axillary Surgery with or without ALND Followed by Radiation Therapy in Patients with Clinically Node-positive Breast Cancer), SENOMAC trial (Sentinel Node Biopsy in Breast Cancer: Omission of Axillary Clearance after Macrometastases) and AXSANA study47–49 search for further advances in the surgical de-escalation of the positive axilla.
We already know that the information about the axillary involvement of breast cancer only carries staging value, good local control can be obtained without ALND even in patients with positive SLNB, and prognostic information of the axillary status has lost importance due to the role of the biological characteristics of the disease (molecular subtypes and genetic platforms) in the treatment decision-making process. Consequently, the current guiding principle for most breast surgeons is not to perform ALND for staging reasons alone.
Conflict of interestThe authors declare that there is no conflict of interest.