Aspergillus fumigatus can cause a wide variety of clinical syndromes, especially in the three largest immunocompromised groups, such as HIV-infected patients. Primary renal aspergillosis is an extremely rare entity.
AimsWe report an unusual case of renal abscess due to Aspergillus fumigatus in a patient with AIDS.
MethodsWe review clinical and laboratory records, and provide follow up of the patient.
ResultsA 38-year-old man, HIV seropositive, was admitted to our hospital with fever, lumbar pain and respiratory symptoms. Abdominal ultrasound and computerised tomography showed a single and large lesion consistent with an abscess located in the left kidney. Aspergillus fumigatus was isolated from clinical sample obtained by ultrasound-guided needle aspiration. Despite a correct treatment based on amphotericin B and drainage of the abscess, surgery was necessary and nephrectomy was carried out. Histopathological examination of the surgical specimen confirmed the diagnosis of renal aspergillosis. Systemic antifungal therapy based on intravenous and oral voriconazole and highly active antiretroviral therapy was started after surgery. The patient had a good response to the established treatment and he remains in a good clinical condition at one year of follow up.
ConclusionsCombined medical and surgical treatment is the elective therapy for renal abscesses due to Aspergillus when percutaneous drainage and the administration of systemic antifungal drugs, such as amphotericin B and/or oral voriconazole or itraconazole, fail. This case emphasizes renal fungal infections should be included in the differential diagnosis of kidney abscesses in AIDS patients.
Aspergillus fumigatus puede provocar un amplio espectro de síndromes clínicos en diversos grupos de pacientes inmunodeficientes, como los infectados por el VIH. La aspergilosis renal primaria es una entidad extremadamente rara.
ObjetivoComunicar un caso infrecuente de absceso renal por Aspergillus fumigatus en un paciente con SIDA.
MétodosRevisión de ficha clínica y seguimiento del paciente.
ResultadosSe presenta el caso de un paciente de 38 años, VIH positivo, quien ingresa en el hospital por presentar fiebre, lumbalgia izquierda y síntomas respiratorios. Los estudios de imagen revelaron la existencia de una gran lesión en el riñón izquierdo compatible con un absceso. La biopsia por aspiración dirigida por ecografía logró la obtención de una muestra clínica que permitió el aislamiento de Aspergillus fumigatus. A pesar del tratamiento con anfotericina B desoxicolato y el drenaje del absceso, el cuadro no mostró mejoría por lo cual se realizó la nefrectomía. El examen histopatológico de la pieza quirúrgica confirmó el diagnóstico de aspergilosis renal. Tras la exéresis se instauró tratamiento con voriconazol por vía intravenosa y oral en forma secuencial, asociado al tratamiento antirretroviral de gran actividad. El paciente mostró una buena respuesta al esquema terapéutico y continuaba en buena condición clínica un año después de su egreso hospitalario.
ConclusionesLa aspergilosis debe incluirse en el diagnóstico diferencial del compromiso renal en pacientes con sida. En el caso que se presenta, el inicio precoz del tratamiento con AMB y luego voriconazol seguido por la nefrectomía permitió la recuperación del paciente con estabilización del cuadro durante el período de seguimiento.
Primary renal aspergillosis is a very rare complication of AIDS and it is associated with a poor prognosis and a high mortality rate1,6. Aspergillosis is unfrequent in AIDS patients. Its incidence has increased during the last years and it has become an important and commonly fatal complication in advanced HIV disease5. Only a few cases have been described in AIDS patients. We report a case of an AIDS patient who developed a unilateral renal abscess due to Aspergillus fumigatus as the only manifestation of disseminated aspergillosis.
A 38-year-old HIV positive heterosexual man, with history of recurrent pneumonia, disseminated tuberculosis, syphilis, drug abuse, chronic hepatitis due to HCV (AIDS C3), was admitted to our unit on account of persistent fever, weight loss, dorsal and lumbar pain, cough and expectoration. On admission he was alert and oriented. Relevant laboratory findings included: hemoglobin 7.4g/dL; hematocrit 21%; white cells count 9700/mm3; platelets count 322,000/mm3; alkaline phosphatase 389U/L (N=90–240U/L); lactate dehydrogenase 376U/L, CD4T cell count 14 cells/μL (2%). Microscopic examination of sputum was positive for acid fast bacilli. Localized radiological opacity in middle lung zones were found as radiographic abnormalities.
Antibacterial therapy using first-line antituberculous drugs (isoniazid, rifampin, pyrazinamide, and ethambutol) was started. Bacteriologic, mycologic and mycobacterial blood cultures were negative. Abdominal ultrasonography scan and computerized tomography scan disclosed liver enlargement and a hypoecoic lesion (45×34×24mm.) in the left kidney, consistent with an abscess (Figs. 1 and 2). Computerized tomography cerebral scan showed no abnormality but cortical brain atrophy. The patient developed left lumbar pain, renal impairment with microhematuria and granulous casts. Culture of sputum obtained on admission showed Mycobacterium tuberculosis mycobacteria other than Mycobacterium tuberculosis. Ciprofloxacin and clarithromycin were added to the first therapeutic regimen.
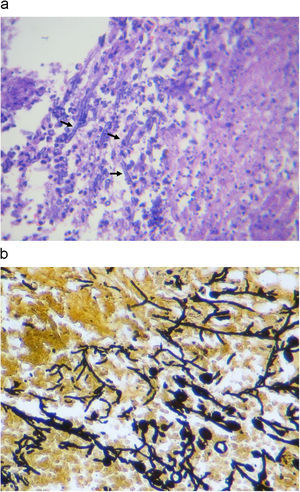
Ultrasonographic percutaneous-guided fine needle drainage of the abscess was performed. Ziehl-Neelsen and Gram stains of the material obtained were negative, but septate hyaline filamentous forms were observed while, in the culture, Aspergillus fumigatus grew. No lesion was found in the echocardiogram. Amphotericin B desoxycholate was prescribed up to an accumulative dose of 180mg, and was discontinued in favor of voriconazole (100mg bid, adjusted to patient's weight) on account of renal impairment and anemia (creatinine clearance 15.6mL/min (N: 70–140), hemoglobin 6.2gr/dL). Finally, a change to pyrazinamide, ethambutol, ofloxacin, clarithromycin (plus voriconazole) was made because of drug interaction between rifampin and voriconazole and M. tuberculosis resistance to isoniazid. The patient's condition worsen despite appropriate antimicrobial therapy, with persistence of the renal abscess and perinephric effusion. Accordingly, a nephrectomy was performed. Histopathological examination of the surgical specimen revealed a cavitary structure inside a necrotic mass. Fungal elements were evident in the necrotic material (Fig. 3a and b). Culture of the specimen showed Aspegillus fumigatus colonies (Fig. 4). Antifungal therapy based on intravenous voriconazole (6mg/kg twice a day as an initial dose followed by 4mg/kg) and highly active antiretroviral therapy was started. After 2 weeks, intravenous voriconazole was replaced by the oral formulation at doses of 200mg twice a day. During one year follow up period the patient had normal renal function with no evidence of recurrence, resolution of pulmonary mycobacteriosis, and immune reconstitution.
Aspergillus species are ubiquitous fungi, some of which can cause a wide variety of clinical manifestations ranging from colonization to severe and invasive disease.7
Only a few species of Aspergillus can cause human illness. The most common is Aspergillus fumigatus and to a lesser extent these infections are caused by Aspergillus flavus, Aspergillus niger and Aspergillus terreus.7,8
Clinical manifestations of Aspergillus infections vary depending on circumstances but can include respiratory involvement, allergic bronchopulmonary aspergillosis, intracavitary aspergilloma, chronic forms of pulmonary aspergillosis, acute invasive aspergillosis, tracheobronchitis and rinosinusitis. The most severe clinical presentation is the acute invasive form. The lung usually is the portal of entry through which the pathogen may disseminate to every organ. Invasive or disseminated aspergillosis mortality rate reaches almost 100%, especially when the central nervous system is infected.9,10
The most common underlying conditions for invasive aspergillosis include immunosuppression for solid organ transplantation, cytotoxic chemotherapy resulting in neutropenia, prolonged therapy with corticosteroids, diabetes and, most recently, advanced HIV/AIDS disease.8,10
Aspergillus abscesses of the kidneys are very rare complications of advanced HIV/AIDS disease and they usually have a fatal outcome.5 It usually occurs in patients with severe immunodeficiency, as in the case we describe. Most rare in this group of patients is infection limited to the kidneys as was shown in our case.3 The hematogenous spread of the Aspergillus infection acquired by inhalation of spores should be attributed to the loss of normal immune mechanisms, due to the retroviral infection in this case.
Clinical diagnosis of renal aspergillosis includes imaging techniques, histopathology, and microbiological examinations. At ultrasonography, renal abscesses due to Aspergillus sp. appear as hypoechoic or anechoic lesions. Computerized tomography scan shows an hypodense and well-defined lesions with ring enhancement, as in our patient. Computerized tomography or ultrasonography guided fine needle aspiration biopsy is the gold standard method to diagnose renal abscess due to Aspergillus.11
Laboratory diagnostic methods of aspergillosis include histopathological evidence of tissue invasion by fungal hyphae and identification of the microorganism by direct microscopy and cultures.7,8
Treatment of renal abscesses due to Aspergillus species includes percutaneous drainage and the administration of systemic antifungal drugs such as amphotericin B, followed by oral voriconazole or itraconazole. In the last five years, voriconazole has become the drug of choice for invasive aspergillosis treatment.4,12 When this strategy fails, as in our patient, nephrectomy followed by a prolonged antifungal systemic therapy is the treatment of choice.2
Conclusions: Nephrectomy followed by a prolonged antifungal systemic therapy is the treatment of choice of renal abscesses due to Aspergillus species when percutaneous drainage and the administration of systemic antifungal drugs such as amphotericin B and/or oral voriconazole or itraconazole fail.
This case emphasizes the fact that renal fungal infection should be included in the differential diagnosis of kidney abscesses in AIDS patients.
Conflict of interestThe authors declare that they do not have any conflict of interest.