Epilepsy is a neurological disease consisting of abnormal electrical discharges in the brain that produce a clinical condition, affecting 1–3% of the population. The Multidisciplinary Epilepsy Unit of the Hospital Universitario y Politécnico La Fe de Valencia, since 2006, has conducted studies with prolonged video-EEG monitoring of patients diagnosed with refractory epilepsy. The role of the unit is to provide these patients with both a diagnostic and a treatment solution.
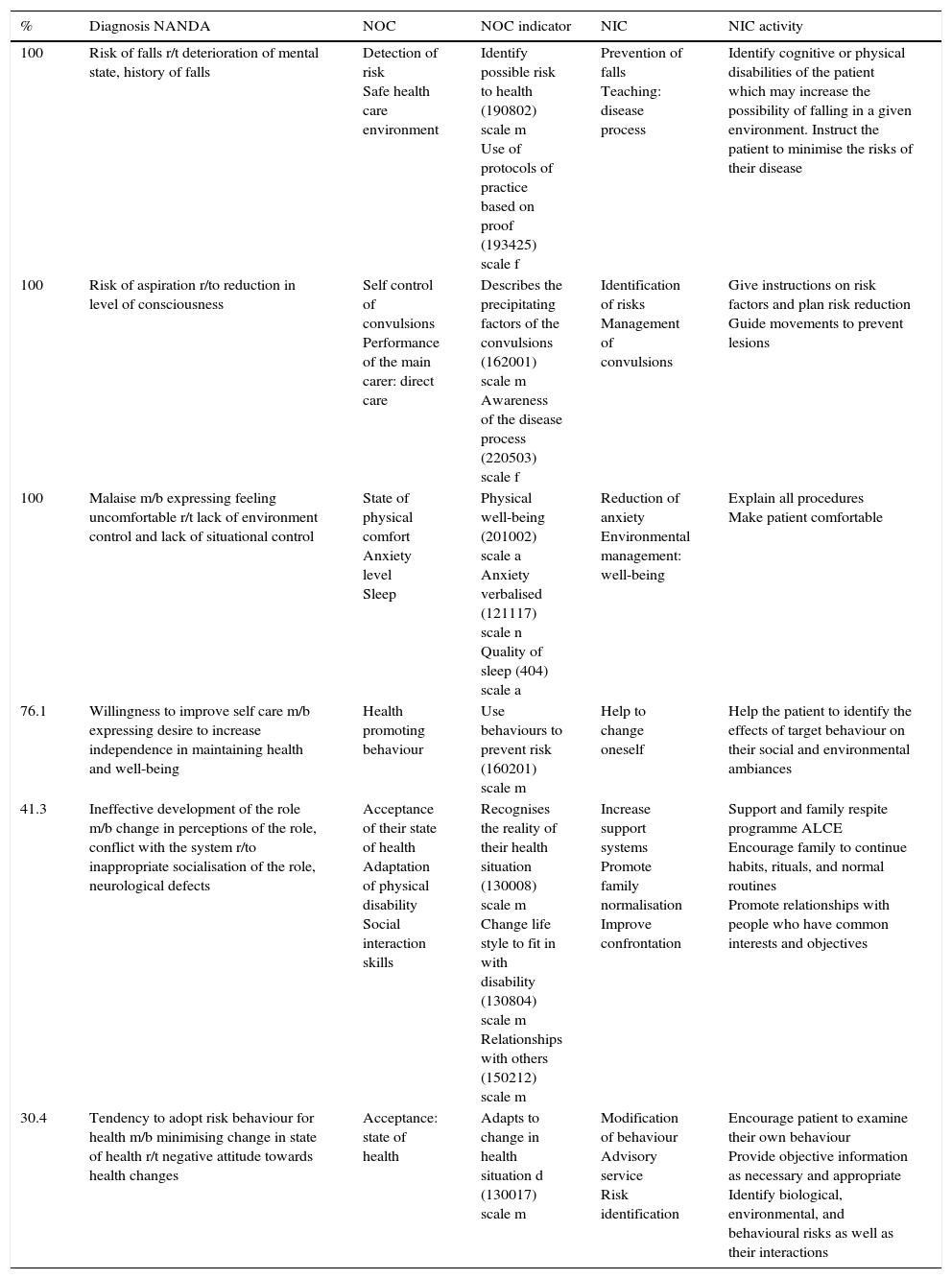
ObjectiveThis study aims to determine, using NANDA-NIC-NOC language, the basic needs of these patients and to assess how the quality of nursing care can be improved in this type of patient, during their admission and afterwards.
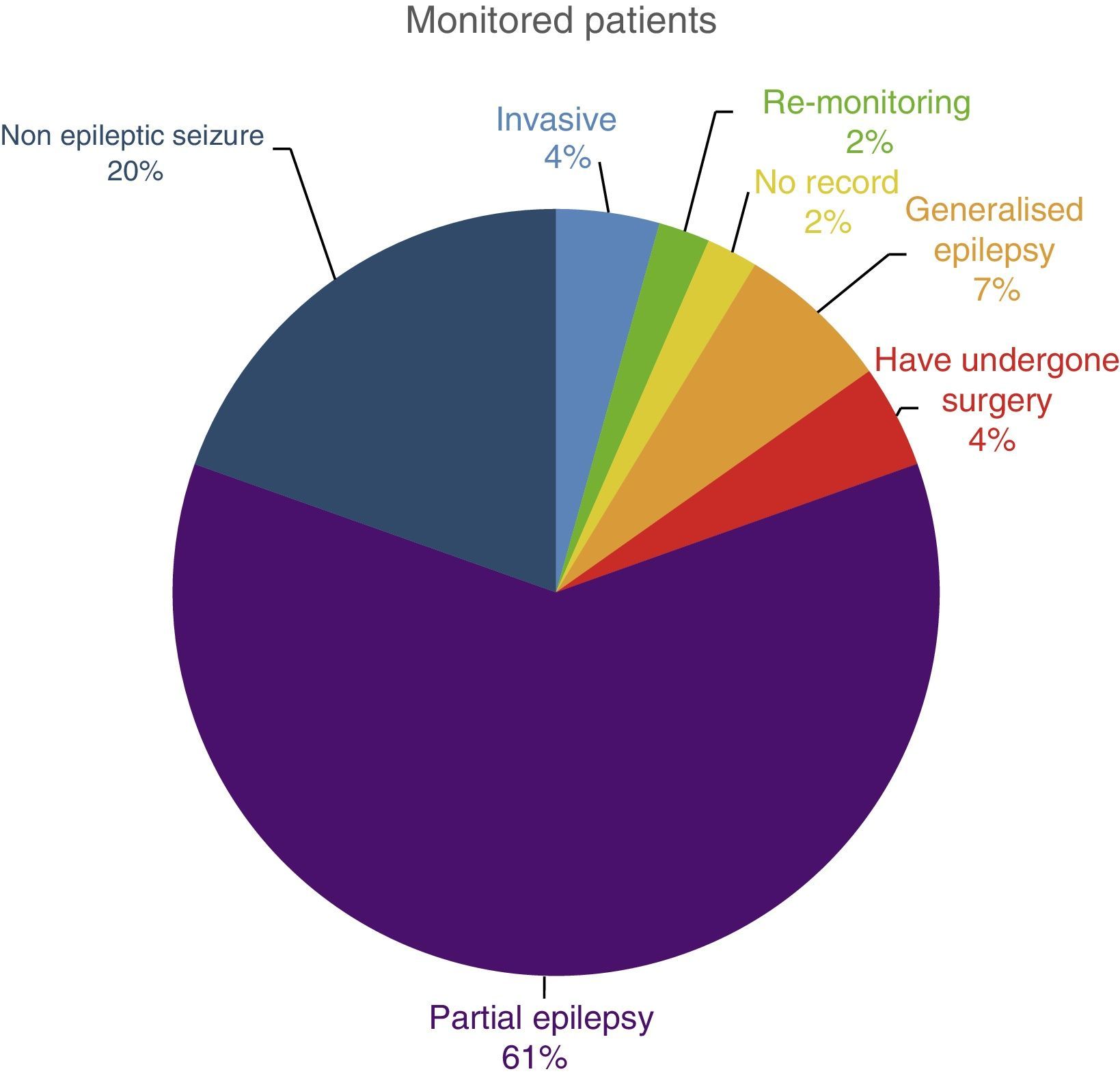
MethodologyData were collected from a sample of 46 patients monitored in the unit between May and September 2013, and by using nursing assessment, data was obtained on the percentage occurrence of diagnosis.
Results and conclusionsThe patients are very limited socially and occupationally, with added risks specific to the disease that we must not forget. The nursing role should be to standardise their situation as much as possible so that they can lead as full a life as possible, have proper health education, and prevent further injuries during admission (falls, etc.). From our experience, the epileptic patient support program from the Epilepsy Association of the Community of Valencia, and its incorporation into the Programa Respira for admission to the monitoring unit, gives good results.
La epilepsia es una enfermedad neurológica consistente en descargas eléctricas del cerebro de forma anormal que producen una clínica, llegando a afectar a entre un 1-3% de la población. La Unidad Multidisciplinar de Epilepsia del Hospital Universitario y Politécnico La Fe de Valencia realiza, desde el 2006, estudios con monitorización prolongada por videoelectroencefalograma a pacientes diagnosticados de epilepsia refractaria. Desde la unidad, se busca dar una solución a estos pacientes tanto en el diagnóstico como en el tratamiento.
ObjetivoCon este estudio se pretende dejar constancia, mediante el lenguaje NANDA-NIC-NOC, de cuáles son las necesidades fundamentales de estos pacientes y valorar en qué se podría mejorar la calidad asistencial enfermera en ellos, tanto durante el ingreso como después del mismo.
MetodologíaSe recogieron datos en una muestra (N=46) de pacientes monitorizados en la unidad entre mayo y septiembre 2013, a través de la valoración de enfermería, obteniendo datos de porcentaje de aparición del diagnóstico.
Resultado y conclusionesSon pacientes muy limitados social y laboralmente, con unos riesgos añadidos propios de la enfermedad que no debemos olvidar, y la función de la enfermera debería ir encaminada a normalizar lo más posible su situación para que puedan llevar una vida lo más plena posible, hacer una correcta educación en salud y evitar daños mayores durante el ingreso (caídas, etc.). Desde nuestra experiencia, el programa de apoyo al paciente epiléptico desde la Asociación de Epilepsia de la Comunidad Valenciana y su consolidación en el programa respira durante el ingreso en la Unidad de monitorización, da buenos resultados.
Article
Diríjase al área privada de socios de la web de la SEDENE, (https://sedene.com/revista-de-sedene/ ) y autentifíquese.