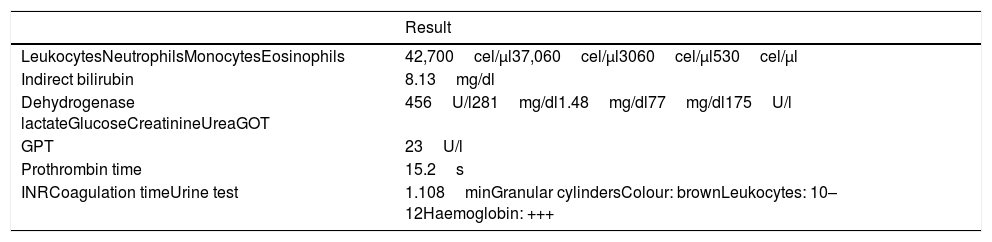
Loxoscelism is the clinical problem produced by the bite of a spider of the genus Loxosceles. The most severe presentation is systemic loxoscelism that can compromise the patient's life if it is not diagnosed and treated in time. There are no reports about how it presents in patients with an epilepsy diagnosis. We present the case of a 28-year-old male patient, with a prior history of epilepsy in treatment with anticonvulsants. He developed systemic loxoscelism after a spider bite in the posterior middle third of the right arm. However, the patient did not develop seizures despite the unfavourable course of his clinical symptoms.
El loxoscelismo es el cuadro clínico producido por la picadura de una araña del género Loxosceles. Tiene 2 presentaciones clínicas, siendo el loxoscelismo sistémico el cuadro más grave, que puede comprometer la vida del paciente si no es diagnosticada y tratada a tiempo. No existen reportes acerca de su presentación en pacientes con diagnóstico de epilepsia. Presentamos el caso de un paciente varón de 28 años, con historia previa de epilepsia en tratamiento con anticonvulsivantes que desarrolló loxoscelismo sistémico posterior a la picadura de una araña en el tercio medio posterior del brazo derecho. El paciente no desarrolló convulsiones pese al curso desfavorable del cuadro clínico.
Article
Diríjase al área privada de socios de la web de la SEDENE, (https://sedene.com/revista-de-sedene/ ) y autentifíquese.