To determine the prevalence of frailty in elderly people living in the community with and without cerebrovascular disease (CVD) and describe the main sociodemographic and clinical characteristics of these patients.
Material and methodDescriptive and cross-sectional study carried out between January and July 2016 in elderly people living in two specific areas of northern Portugal. Data were collected using a sociodemographic and clinical questionnaire. The existence of previous CVD was evaluated through an initial assessment and application of the Charlson Comorbidity Index. Frailty was assessed using the criteria of phenotypic methodology.
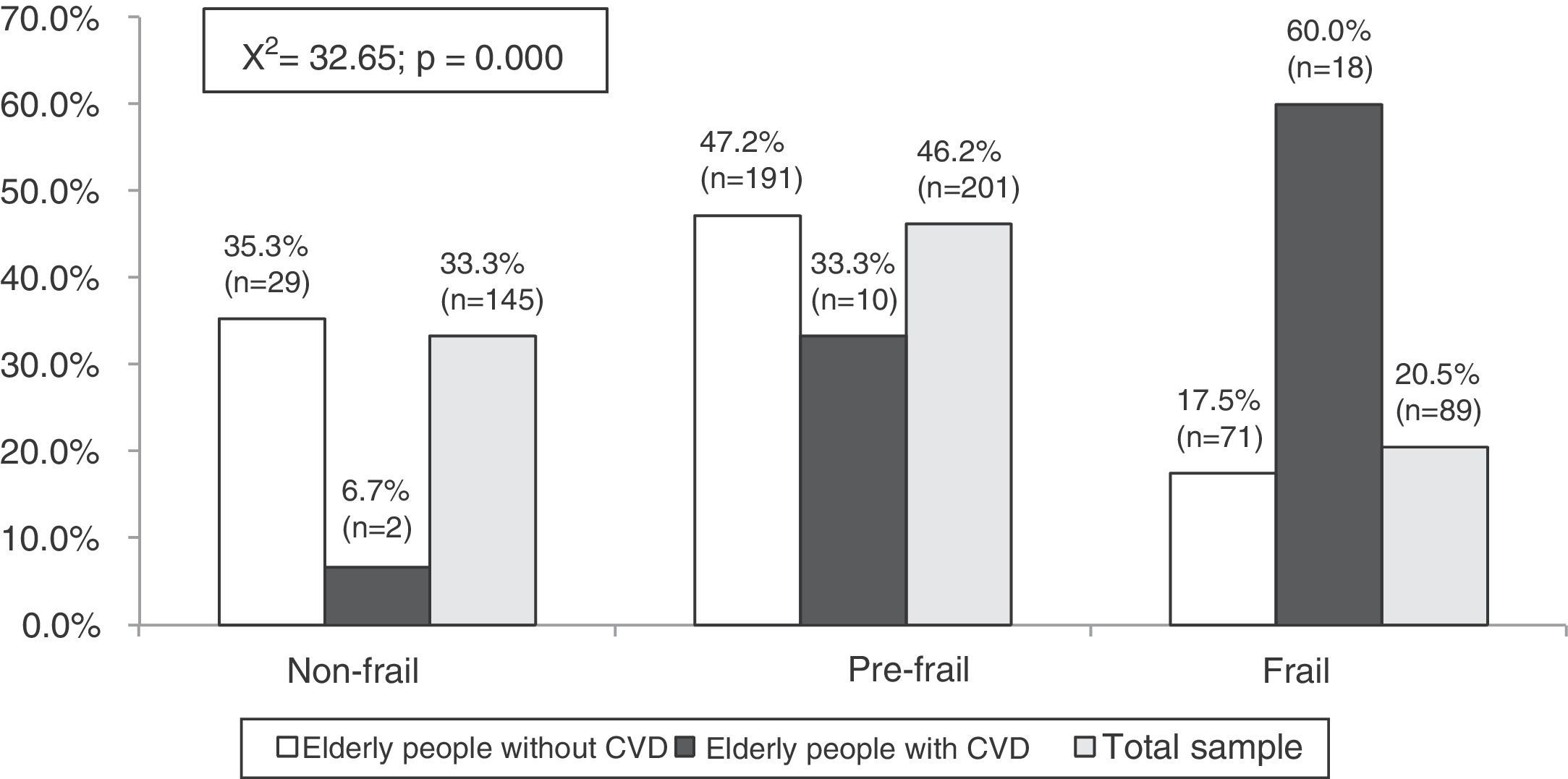
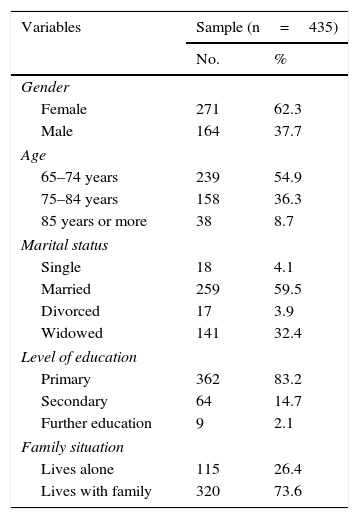
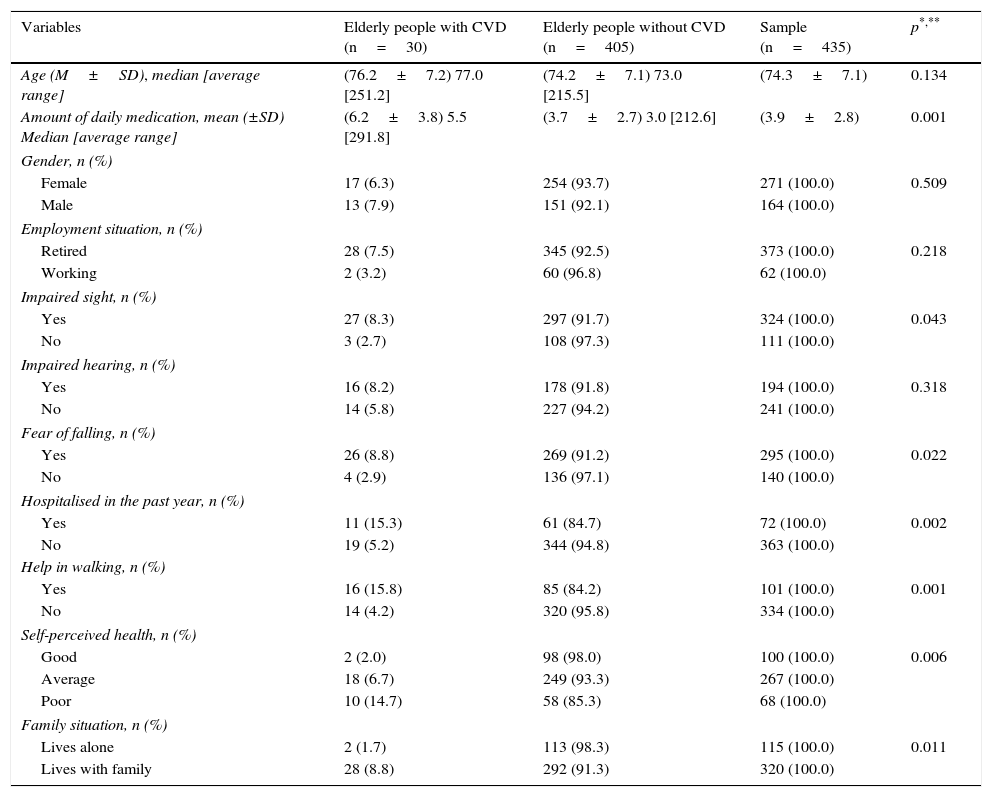
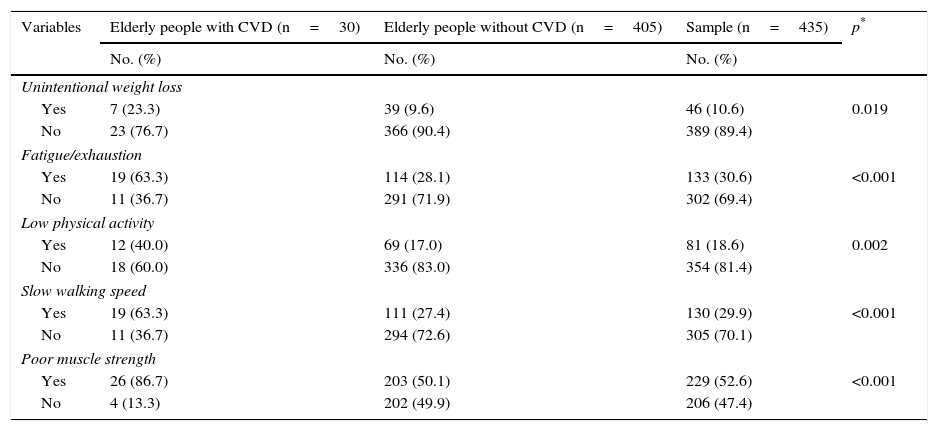
ResultsA total of 435 participants, aged >65 years (mean=74.3 years), mostly women (62.3%), were studied. Six point nine percent of the elderly people had a history of CVD. The prevalence of frailty syndrome was 60.0% in the elderly people with a history of CVD, and 20.5% in the other cases (p<0.05). Statistically significant relationships (p<0.05) were found between CVD and vision problems, fear of falling, hospitalisations in the last year, use of walking aids and perception of health status.
ConclusionMost of the elderly with a history of CVD were frail. According to the phenotypic theory, frailty is a state that precedes total dependence. The diagnosis and management of frailty may help to prevent adverse events that precipitate the institutionalisation of the elderly with CVD.
Determinar la prevalencia de fragilidad en ancianos que viven en la comunidad con y sin enfermedad cerebrovascular (ECV) y describir las principales características sociodemográficas y clínicas que presentan dichos pacientes.
Material y métodoEstudio descriptivo y transversal realizado entre enero y julio de 2016 en personas mayores residentes en 2 zonas concretas del Norte de Portugal. Los datos se han recogido mediante un cuestionario sociodemográfico y clínico. La existencia de ECV previa se evaluó a través de una valoración inicial y aplicación del Índice de comorbilidad de Charlson, y la fragilidad utilizando los criterios de la metodología fenotípica.
ResultadosSe estudiaron 435 participantes, de edad>65 años (media=74,3 años), siendo en su mayoría mujeres (62,3%). El 6,9% de los ancianos tenía antecedentes de ECV. La prevalencia del síndrome de fragilidad fue de 60,0% en los ancianos con antecedentes de ECV y 20,5% en los restantes casos (p<0,05). Relaciones estadísticamente significativas (p<0,05) fueron encontradas entre ECV y problemas de visión, miedo a caer, hospitalizaciones en el último año, uso de ayudas para caminar y percepción del estado de salud.
ConclusiónLa mayoría de los ancianos con antecedentes de ECV eran frágiles. Según la teoría fenotípica la fragilidad es un estado que precede a la dependencia total. El diagnóstico y la gestión de la fragilidad podrán ayudar a la prevención de eventos adversos que precipitan la institucionalización del anciano con ECV.
Article
Diríjase al área privada de socios de la web de la SEDENE, (https://sedene.com/revista-de-sedene/ ) y autentifíquese.