Cancerous tumors of the extrahepatic bile duct are uncommon (less than 2% of all neoplasms).1–4 About 85% are cholangiocarcinomas, while the remaining 15% are miscellaneous tumors, including carcinoid tumors which represent 0.2%–0.34% of all bile duct neoplasms.1–7
The first case of carcinoid tumor of the bile duct was described by Davies in 1959, and up until 2009 only 60 cases had been published.1–4,6,8,9 We present a new case of bile duct carcinoma and discuss the symptoms, diagnosis, treatment and prognosis of this rare neoplasm.
The patient is a 14-year-old female with a self-palpated epigastric mass and abdominal distension. On examination, a mass in the right epigastrium and hypochondrium was detected. Results from blood tests (hemogram, hepatic biochemistry, coagulation, viral serology [hepatitis A, B C and D; EBV, CMV] and tumor markers [CEA, CA19-9 and αFP]) were normal.
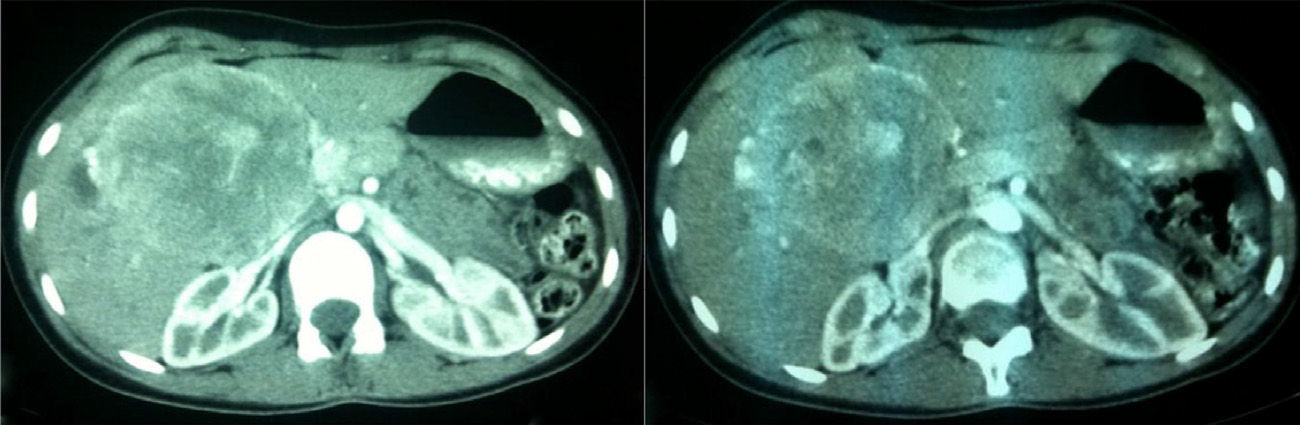
Ultrasound and abdominal CT showed a solid, isoechoic, homogeneous lesion in the hepatic hilum measuring 10cm in diameter (Fig. 1). The tumor was in contact with and displaced the hepatic hilum and compressed the common bile duct, producing mild dilatation of the right intrahepatic bile duct. There were another 2 hyperechoic lesions measuring 14 and 27mm in segment v.
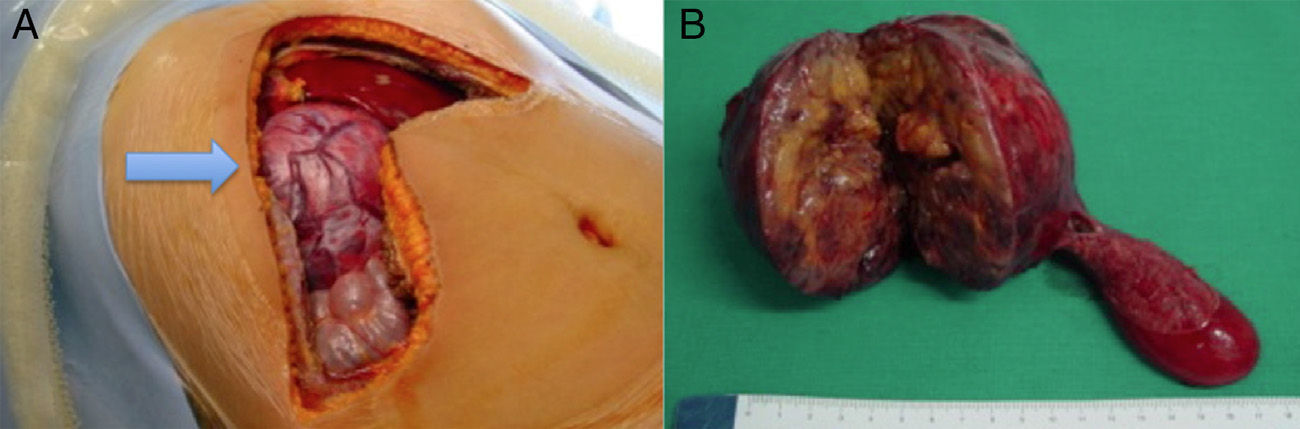
With the diagnosis of probable hepatoblastoma, surgery was performed, and a large mass was observed in the hilar region that infiltrated the right liver lobe. Intraoperative ultrasound detected several lesions in segments ivb, v, vi and viii. Intraoperative biopsy was reported to be either hepatoblastoma or neuroendocrine tumor. A right hepatectomy was performed with resection of subsegment ivb, portal lymph node dissection and total resection of the extrahepatic bile duct with hepaticojejunostomy (Fig. 2).
During the postoperative period, the patient presented a low-output biliary fistula (grade A) that resolved with conservative treatment, and she was discharged on the 10th day post-op. The definitive histology results were: differentiated neuroendocrine tumor of the bile duct (carcinoid) with a moderate mitotic rate, and presence of numerous vascular thrombi with no lymph node involvement. Immunohistochemistry was positive for chromogranin, synaptophysin and PGP5; negative for vimentin, alpha-fetoprotein, alpha-antitrypsin, CEA, beta-HCG, S-100 and neurofilaments; and (+/−) for EMA and PanCK. Postoperative determinations for 5 HIAA in urine as well as serum chromogranin A and serotonin were normal. One hundred months after the surgical procedure, the patient remains disease-free.
Carcinoid tumors arise from argentaffin cells (probably endodermal) that originate in the embryonic neural crest (Kulchistky cells) and migrate during embryonic development.1–6,10 Carcinoid tumors of the biliary system (gallbladder and biliary tree) represent only 0.2%–2% of these lesions.1,2,4–6,8,9 This extremely low frequency is due to the fact that the settling of these cells in the bile duct is exceptional. It has been postulated that chronic inflammatory processes of the bile duct could induce phenomena of metaplasia in these cells and cause carcinoid tumor of the bile duct.1,4,10
Carcinoid tumors of the bile duct are more frequent in women (ratio 2:1), and the mean age of presentation is 47 (range 10–79).1–3,5,7,8 There have only been 5 cases reported in adolescents and children.5,10 These tumors are located in: the common bile duct (55%), hilar region (30%), cystic duct (11%) and hepatic duct (3%).1,2,8 The most frequent symptom is jaundice (55%–70%), followed by abdominal pain.1,3,5,8,9 Although they may be active hormonally, it is exceptional for them to present symptoms derived from hormonal secretion, and serum 5 HIAA levels are usually normal.1,3,8–10 Carcinoid tumors of the bile duct have been described in association with von-Hippel Lindau and MEN I.2
Correct preoperative diagnosis of these tumors is very uncommon.4–6,8,10 Several diagnostic methods are used (ultrasound, abdominal CT, MR cholangiography and ERCP).8 Intraluminal polypoid lesions on cholangiography are suggestive of carcinoid tumor of the biliary duct.3
When a carcinoid tumor is found, there are 2 possible scenarios: it is usually (75%) an incidental finding during laparotomies performed for a misdiagnosis (choledocholithiasis, cholangitis)1,3,9; in the remaining cases, the intervention is done under the suspicion of cholangiocarcinoma.2,8 Carcinoid tumors of the bile duct have a series of typical clinical characteristics, including: female sex, 5th decade of life, limited local aggressivity, low rate of metastatic disease (30% of patients), and simple R0 resection.1,2,6 In our case, due to the patient's age and presence of a liver mass, we thought the lesion was a hepatoblastoma.
These carcinoid tumors are usually small and made up of small cells that present high rates of perineural and vascular invasion; they are also immunoreactive to chromogranin and negative for p53.2,5,7 The histologic differential diagnosis includes adenocarcinomas with isolated endocrine cells or small-cell carcinomas.2 The WHO has recently substituted the term carcinoid tumor of the bile duct for differentiated neuroendocrine tumor of the biliary duct.7
Surgical resection is the treatment of choice for these tumors and the only therapy that offers a possible cure.1,5,6,9 Complete tumor excision should be achieved with free margins.1,3 To do so, complete resection of the bile duct is usually done with portal lymph node dissection and reconstruction using hepaticojejunostomy.1,9,10 There are only 3 previously reported cases in which, due to direct invasion (hilar localization) or liver metastasis, a hepatectomy was performed during the same surgery as in our case (2 right hepatectomies and right trisectionectomy).6 There are 2 patients who were treated with liver transplantation.4
30% of patients present metastatic disease at diagnosis, which is located in the liver in 50% of cases.1,8 There is no correlation between tumor size and the presence of metastasis.2
In the literature, all the patients with R0 resection are alive and disease-free.1,5,6,10 Among those who present metastatic disease, 50% die during follow-up; their 5-year disease-free survival ranges between 40% and 80%, with a mean survival of 90 months.1,6,7,9 Postoperative treatment with chemotherapy (5-fluorouracil and streptozotocin) has not been able to demonstrate an increase in survival1,3 and, according to the NCCN, it is not indicated in completely resected cases.11
Please cite this article as: Ramia JM, Garrote D, Muffak K, Villegas T, Ferrón A. Tumor carcinoide de la vía biliar extrahepática en adolescente: larga supervivencia libre de enfermedad tras resección quirúrgica. Cir Esp. 2014;92:636–638.