Plasmacytomas represent 5% of all plasma cell neoplasms. Its most frequent presentation is as a solitary intraosseous mass (intramedullary plasmacytomas).1,2 Extramedullary plasmacytomas (EMP) are rare tumors usually located in the cervicofacial region. An extremely rare presentation of EMP is as a symptomatic abdominal or retroperitoneal mass causing abdominal pain or symptoms related to direct compression.1,3,4 In the case of an intramedullary plasmacytoma causing compressive symptoms, surgical resection is recommended; by extrapolation, resection should be considered in the presence of symptomatic EMP.4,5 Complete tumor excision is the treatment of choice for any retroperitoneal mass. In fragile patients, however, laparoscopic tumor reduction surgery could be a more efficient solution that increases quality of life, reduces risk and increases the efficacy of adjuvant therapy. We present a laparoscopic partial resection (80% of the tumor) of a symptomatic EMP.
An 81-year-old male consulted for three weeks of abdominal pain, reporting no previous abdominal trauma. The pain was located in the upper left quadrant, and non-steroidal anti-inflammatory drugs partially improved symptoms. His medical history included hypertension, atrial fibrillation, type II diabetes, stents in the arteries of both lower extremities for peripheral arterial disease, hypothyroidism, gastritis/duodenitis, pneumonia and appendectomy. His daily medication was: bisoprolol, pantoprazole, furosemide, levothyroxine and rivaroxaban.
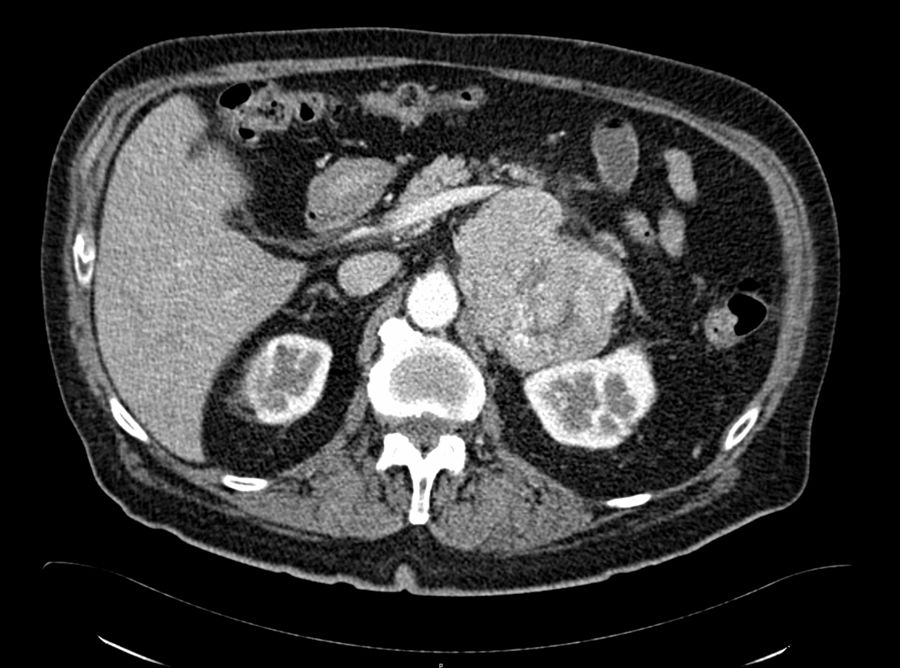
Ultrasound demonstrated a heterogeneous mass near the left kidney measuring 6.5×5.2cm and a left renal cyst. Lab work showed neutrophilia (81.2%), and the remaining parameters were normal, without elevated inflammatory markers or electrolyte imbalance. CT scan confirmed the existence of a retroperitoneal oval nodular lesion that seemed to originate in the left adrenal gland (Fig. 1). Magnetic resonance imaging showed a tumor measuring 9.7×7.5×10cm, located medially to the left kidney with slight displacement of the renal artery, splenic artery and vein, and possible invasion of the renal vein, as well as an 11mm cyst on the inferior side of the left kidney. Standard lab work was ordered to rule out a pheochromocytoma.6
The patient presented progressively greater pain, requiring the use of high-dose opioids. After careful preoperative evaluation, the patient was considered high risk (Charlson: 8, ASA: III). Given the incapacitating symptoms, we decided to perform laparoscopic partial tumor resection. The patient was placed in left lateral decubitus with the left arm raised above the head. Four trocars were used: left paraumbilical for the optics, auxiliary on the left axillary line (subcostal edge), and two working trocars (midline hypogastrium and midline epigastrium). Partial resection (80%) of the tumor was performed, including the adrenal gland and perirenal adipose tissue using a harmonic scalpel, with blood loss of 135cc. The specimen was extracted in a bag after expanding the umbilical trocar incision. In the postoperative period, a decrease in hemoglobin was observed, which required a transfusion (Clavien Dindo: II), and CT scan identified a 5-cm fluid collection located at the tumor excision site, without active bleeding. The hospital stay was 5 days.
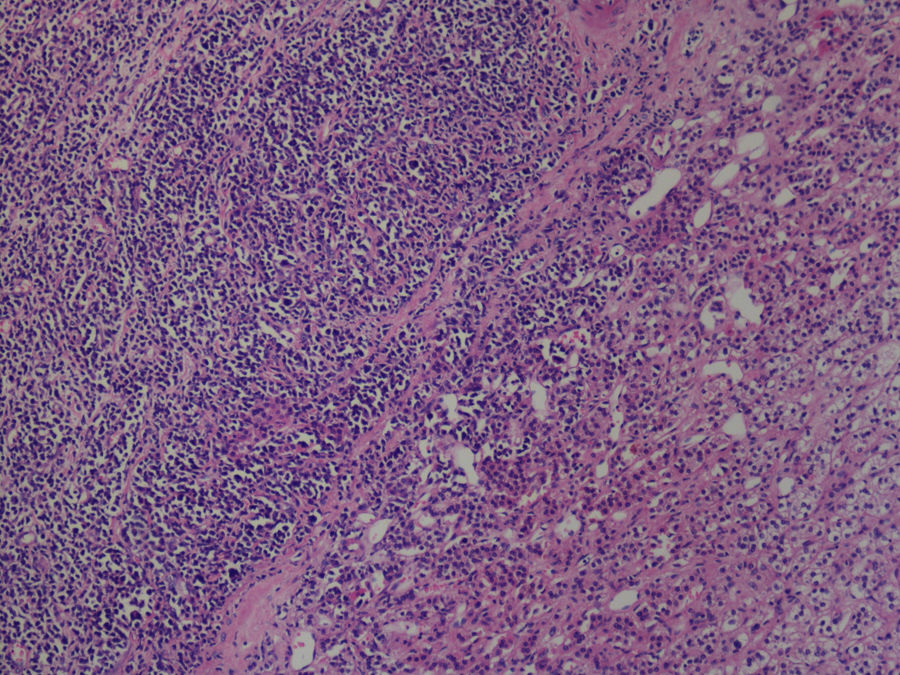
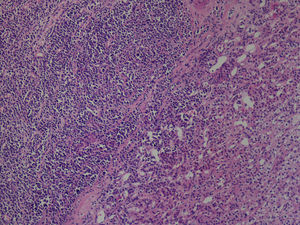
Histological examination showed a mass invading the adrenal gland and adipose tissue, comprised of blast-like monomorphic cells, with centrally located oval nuclei and basophilic cytoplasm (Fig. 2). The immunohistochemical study found that most cells were positive for CD38, CD138, and MUM1, while fewer cells were positive for cyclin D1+ and only a few for PAX5. CD30 was negative in all cells. IgG was positive, but without light chain immunohistochemical expression. The final diagnosis was plasmablastic plasmacytoma.
The patient did not present abdominal pain after partial resection. Abdominal CT scan performed one month after surgery showed a small residual tumor. PET/CT scan confirmed the residual disease. The patient tolerated radiotherapy well and has shown no progression in the following 14 months.
There is very limited evidence about the incidence and treatment of solitary abdominal and retroperitoneal plasmacytomas. A population analysis of the United States Surveillance, Epidemiology and End Results (SEER) database (1998–2007) included 540 cases of solitary EMP.7 Of all solitary plasmacytomas (1691 in total), radiation therapy was the most widely used treatment (48.8%).7 However, surgical treatment was more frequent in patients whose tumors were located in the abdomen and retroperitoneum (49.0%).7 A multivariate analysis showed that radiotherapy (risk 0.597) and surgical treatment (risk 0.764) were associated with increased survival.7 Five-year survival was greater in patients who underwent surgery (69.7%) compared to those who did not (54.7%).7
In 2004, the UK Myeloma Forum accepted the recommendation to surgically remove solitary extramedullary plasmacytoma not located in the head and neck area (grade B, level of evidence III), when possible.4 Partial resection is considered a palliative option. The feasibility and effectiveness of laparoscopic treatment of retroperitoneal or abdominal EMP has only been described in clinical cases or very short series, with no controlled studies providing information with valid scientific evidence.8,9
Our patient presented with a solitary retroperitoneal EMP in the region of the left adrenal gland and renal adipose tissue, causing severe pain that was poorly controlled with opiates. Complete excision with free margins, which would have been the technique of choice, would have required at the very least nephrectomy, splenectomy and adrenalectomy in a patient with comorbidities that contraindicate aggressive surgery (81 years, Charlson: 8). Possible therapeutic options included almost complete resection with a minimally invasive approach, or radiotherapy. While suboptimal, the surgery we performed provided histological confirmation, reduced the tumor burden to be treated with radiotherapy, and entailed low morbidity. Thus, we feel it may be a useful option for this specific type of patient.
Authorship/CollaboratorsData collection: Andrzej Gasz, Jan Danko, Maros Straka and Lazo Ilic.
Analysis and interpretation of the results: Andrzej Gasz, Jan Danko, Maros Straka, Lazo Ilic and José M. Ramia.
Article composition: Andrzej Gasz and José M. Ramia.
Critical review and approval of the final version: Andrzej Gasz and José M. Ramia.
Please cite this article as: Gasz A, Danko J, Straka M, Ilic L, Ramia JM. Resección parcial laparoscópica de plasmocitoma extramedular retroperitoneal. Cir Esp. 2020;98:299–301.