Cystic fibrosis (CF) is a recessive autosomal disease caused by the mutation of a gene located in the long arm of chromosome 7, that causes the dysfunction of a protein known as cystic fibrosis transmembrane conductance regulator (CFTR). This protein participates in the transmembrane transport of chlorine in the epithelial cells of the airways, pancreas, liver, intestines, sweat glands and vas deferens, which results in the production of abnormally thick secretions. Symptomatic episodes of cholangitis or jaundice secondary to hepatolithiasis are very infrequent, and less than 14 cases have been reported in the literature. Given the progressive improvement in the prognosis of CF patients,1,2 a higher incidence of this pathology can be expected, which would be a challenge for surgeons due to the limited experience to date.
We present the case of a 31-year-old woman diagnosed with CF, in treatment for bronchiectasis colonized by Pseudomona aeurginosa (P. aeruginosa) and exocrine pancreatic insufficiency treated with pancreatic enzymes. She had undergone cholecystectomy 4 years earlier due to recurring episodes of biliary colic. She came to our consultation because of pain in the right hypochondrium. Magnetic resonance imaging detected choledocholithiasis with dilatation of the right posterior intrahepatic biliary radicles, which was treated by means of endoscopic retrograde cholangiopancreatography (ERCP). The procedure caused a perforation of the distal common bile duct that required urgent surgery for Kher tube placement in the proximal common bile duct, gastrostomy and jejunostomy for enteral feeding. The postoperative recovery was favorable.
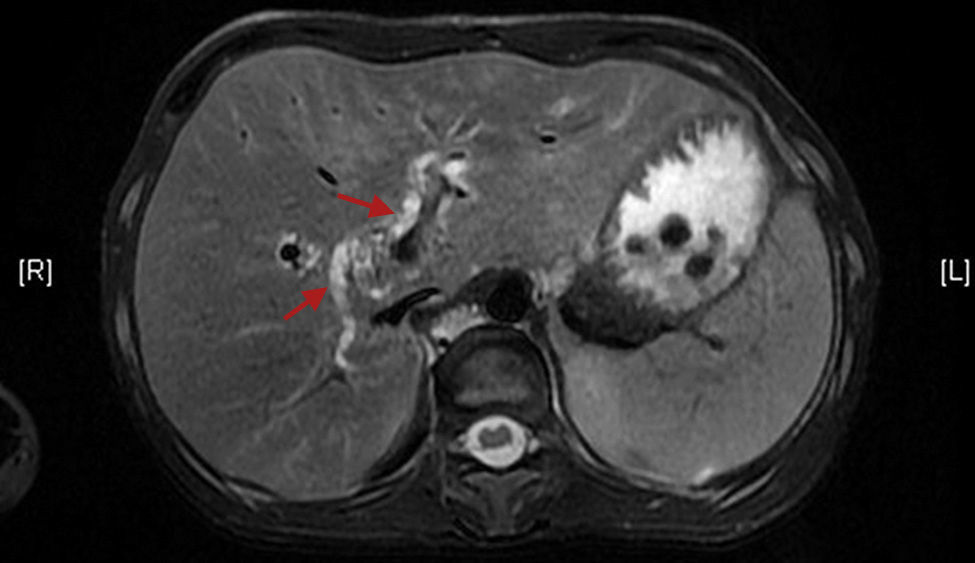
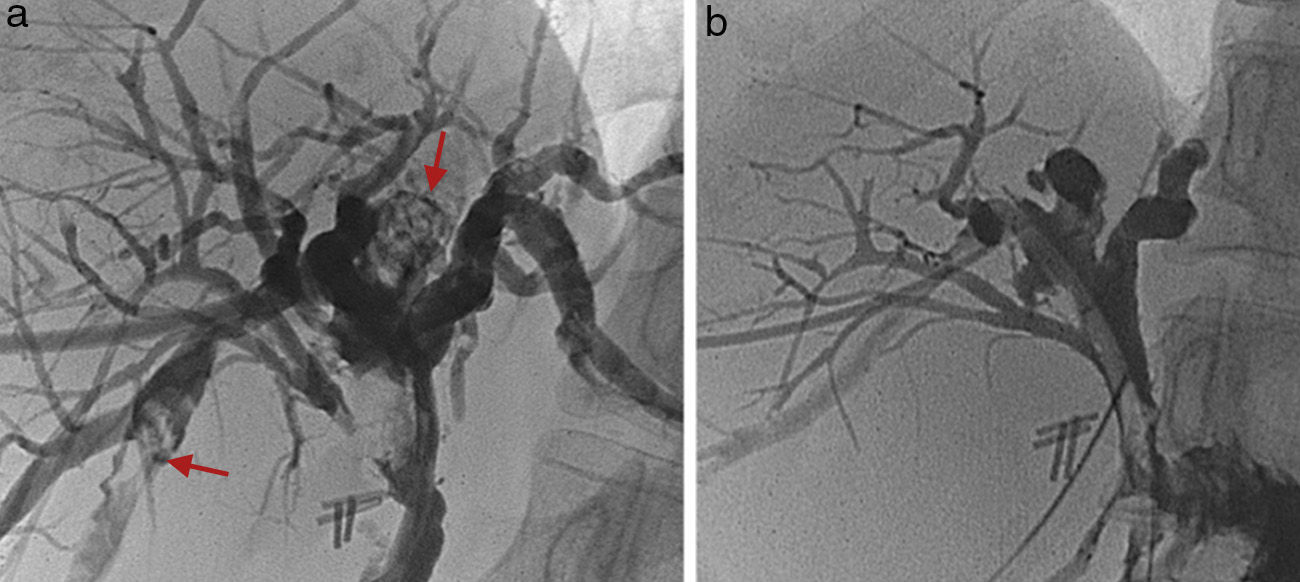
Approximately one month later, the patient experienced renewed episodes of pain in the right hypochondrium, accompanied by 38°C fever and jaundice, with total bilirubin levels of 3.3mg/dl. Ultrasound and magnetic resonance (Fig. 1) revealed bilateral dilatation of the intrahepatic bile duct with the presence of bilateral intrahepatic lithiasis. After the insertion of a transmural drain (Fig. 2a), the skin and mucous membrane jaundice and cholangitis improved. Elective surgery included a right subcostal incision with choledochotomy under direct vision with choledochoscopy and extraction of the calculi from the intrahepatic bile duct with a Fogarty® catheter. The intervention was completed with a high, extended Roux-en-Y hepatic-jejunostomy. Given the persistent etiopathogenic mechanisms that increase the incidence of bile stasis in CF patients, the blind end of the ascended loop was affixed to the abdominal wall (Hutson-Russell loop) in order to provide percutaneous access to the bile duct for any future recurrence. Postoperative percutaneous transhepatic cholangiography (PTC) showed evidence of the clearance of the bilateral hepatolithiasis, as well as mild extravasation of contrast at the hepaticojejunostomy, which evolved favorably with conservative treatment (Fig. 2b). One year after the intervention, the patient remains asymptomatic with no signs of recurrence.
In the human liver, CFTR is expressed in the membrane of the epithelial cells of the bile ducts and gallbladder, but not in hepatocytes. The loss of this protein function reduces the hydration and alkalization of bile secretions, causing periodical blockage of the bile ducts due to thick periodic acid-Schiff (PAS)-positive secretions. These secretions, together with their toxic action on the biliary epithelium, lead to chronic periductal inflammation and periductal fibrosis.1–4 In magnetic resonance imaging studies, evidence has been seen of cholangiopathy similar to primary sclerosing cholangitis in half of CF patients without liver involvement.5 The etiopathogenic mechanism in these patients is based on a vicious cycle of biliary stenosis, infection and lithogenesis. In CF, biliary stasis secondary to abnormally thick bile secretions and anatomical alterations in the intrahepatic bile ducts favor their overinfection, making an ideal environment for the development of intrahepatic lithiasis and recurring cholangitis, which can aggravate symptoms by increasing the chronic inflammatory reaction of the bile duct and, consequently, histological changes.6,7
The preferred initial approach to symptomatic hepatolithiasis is usually non-surgical therapy using ERCP or PTC because they are relatively innocuous techniques, even though there is high risk for recurrence. As for surgical treatment, hepatectomy is considered by many authors the treatment of choice in cases of hepatolithiasis,8 especially when the involvement is unilateral or limited. Hepatectomy eliminates both the calculi as well as any bile duct stenosis, with recurrence rates that are lower than those of other treatments. Given the similarities of this case with recurrent pyogenic cholangitis, we decided to use Roux-en-Y hepaticojejunostomy with a Hutson-Russell loop. It is a technique used with certain frequency for the treatment of this pathology and other stenosing diseases of the bile tract,9,10 and it avoids the risk of post-resection hepatic insufficiency while enabling the percutaneous treatment of any possible recurrences (which is an important aspect of this surgical technique in CF patients). Although this procedure has been successfully used in patients with stenosing diseases of the biliary tree, it is the first time that it has been described in the treatment of CF patients.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Mon Martín F, Martín Malagón AI, Arteaga González IJ, Díaz Luís H, Carrillo Pallares ÁL. Hepatolitiasis en fibrosis quística: una condición especial para el tratamiento quirúrgico. Cir Esp. 2014;92:634–635.