Breast cancer (BC) is the most common cancer in the world. In 2020, 33 000 new cases were diagnosed in Spain.1
There is no doubt that major ambulatory surgery (MAS) provides important benefits, not only for patients but also for healthcare services. Early discharge has been shown to contribute to greater healthcare efficiency, without compromising the quality of care.2 Margolese et al.3 verified that MAS provides several advantages for the treatment of BC: greater satisfaction, psychological benefits for patients, reduced healthcare costs, etc, without compromising surgical outcomes in terms of morbidity or readmissions.
During the Covid pandemic, it was necessary to make changes to enable us to adequately treat our patients in a timely manner. Thus, we made changes in our daily practice and action protocols in order to transform hospitalization regimens into MAS programs. To maintain our activity and provide surgical treatments for our patients, a MAS program was launched, which included patients with drains.
The objective of this study is to analyze the results from the implementation of a MAS program in patients who underwent surgery for breast cancer and required either axillary or breast drains.
In 2020, 364 patients with BC were treated surgically, which were classified into Group 1 (before the pandemic) and Group 2 (during the pandemic). Table 1 shows the descriptive data of both groups.
Demographic and clinical characteristics of the study sample.
| In general (n = 364) | Group I (n = 93) | Group II (n = 271) | P | |
|---|---|---|---|---|
| Age, yrs | ||||
| Mean (SD) | 55.7 (14.1) | 56.3 (13.0) | 55.5 (14.5) | .6362a |
| 95% CI | 54.3 a 57.2 | 53.6 a 59.0 | 53.8 a 57.2 | |
| CC, n (%) | ||||
| Yes | 249 (68.4) | 55 (59.1) | 194 (71.6) | .0286b |
| No | 115 (31.6) | 38 (40.9) | 77 (28.1) | |
| Malignancy, n (%) | ||||
| Yes | 300 (82.4) | 71 (66.3) | 229 (84.5) | .0833b |
| No | 64 (17.6) | 22 (23.7) | 42 (15.5) | |
| Surgical procedure, n (%)* | ||||
| Lumpectomy | 84 (23.2) | 21 (22.8) | 63 (23.3) | |
| Lumpectomy + SLNB | 149 (41.2) | 29 (31.5) | 120 (44.4) | |
| Lumpectomy + AL | 2 (0.6) | 1 (1.1) | 1 (0.4) | |
| Simple mastectomy | 12 (3.3) | 6 (6.5) | 6 (2.2) | |
| Mastectomy + SLNB | 53 (14.6) | 14 (15.2) | 39 (14.4) | .2002c |
| Mastectomy + LA | 24 (6.6) | 7 (7.6) | 17 (6.3) | |
| SSM/NSM | 22 (6.1) | 10 (10.9) | 12 (4.4) | |
| SLNB | 5 (1.4) | 1 (1.1) | 4 (1.5) | |
| AL | 4 (1.1) | 1 (1.1) | 3 (1.1) | |
| Oncoplastic lumpectomy | 7 (1.9) | 2 (2.2) | 5 (1.9) | |
| MAS, n (%) | ||||
| Yes | 270 (74.2) | 30 (32.3) | 240 (88.6) | <.0001b |
| No | 94 (25.8) | 63 (67.7) | 31 (11.4) | |
| Received NA | 125 (34.34) | 31(33.3) | 94(34.6) | |
| Malignant in MAS, n (%) | 226 | 20 (28.2) | 206 (90) | .00 |
| Benign in MAS, n (%) | 44 | 10 (45) | 34 (81) | .04 |
| BCS in MAS, n | 211 | 30 | 181 | .02 |
| Mastectomy in MAS, n | 59 | 0 | 59 | .00 |
| BCS in ordinary, n | 39 | 25 | 14 | |
| Mastectomy in ordinary, n | 75 | 58 | 17 | .00 |
SD: standard deviation; CI: confidence interval; MAS: major ambulatory surgery; BCS: breast-conserving surgery; SLNB: sentinel lymph node biopsy; AL: axillary lymphadenectomy; SSM/NSM: skin-sparing/nipple-sparing mastectomy.
Group I: subjects who underwent surgery from January 1 to March 15, 2020.
Group II: subjects who underwent surgery March 16 to December al 31, 2020.
The percentage of patients with malignant pathology who underwent surgery without hospital admission was significantly higher in group 2. We did not increase the number of mastectomies, but we did reduce reconstructive procedures.
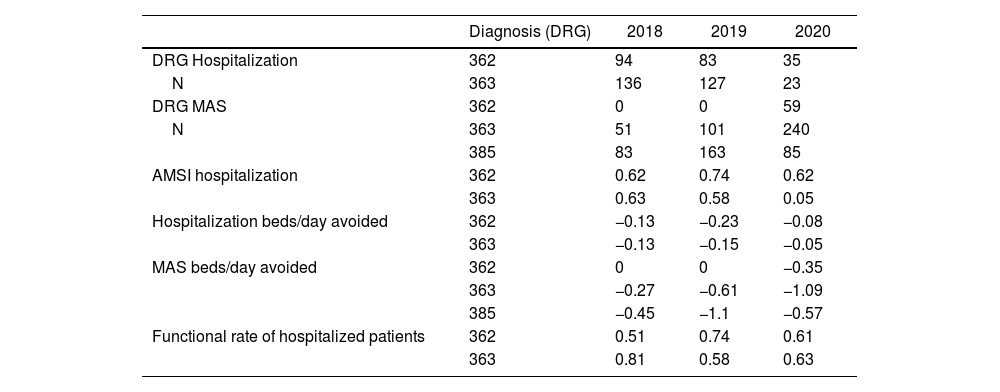
In terms of care quality indices, a descriptive comparison was conducted for the years 2018, 2019 and 2020 (Table 2). The number of inpatient surgeries in 2020 decreased considerably, while the number of outpatient surgical procedures increased. In 2020, the inpatient beds avoided for mastectomy and lumpectomy, including selective biopsy of the sentinel lymph node, were −0.35 beds/day and −1.09 beds/day, respectively, which represents cost savings and greater efficiency.
Quality indicators of the groups related with the most common hospital and ambulatory diagnoses in breast pathology from 2018, 2019 and 2020 at our hospital.
| Diagnosis (DRG) | 2018 | 2019 | 2020 | |
|---|---|---|---|---|
| DRG Hospitalization | 362 | 94 | 83 | 35 |
| N | 363 | 136 | 127 | 23 |
| DRG MAS | 362 | 0 | 0 | 59 |
| N | 363 | 51 | 101 | 240 |
| 385 | 83 | 163 | 85 | |
| AMSI hospitalization | 362 | 0.62 | 0.74 | 0.62 |
| 363 | 0.63 | 0.58 | 0.05 | |
| Hospitalization beds/day avoided | 362 | −0.13 | −0.23 | −0.08 |
| 363 | −0.13 | −0.15 | −0.05 | |
| MAS beds/day avoided | 362 | 0 | 0 | −0.35 |
| 363 | −0.27 | −0.61 | −1.09 | |
| 385 | −0.45 | −1.1 | −0.57 | |
| Functional rate of hospitalized patients | 362 | 0.51 | 0.74 | 0.61 |
| 363 | 0.81 | 0.58 | 0.63 |
DRG: diagnosis-related group; AMSI: adjusted mean stay index; 363: non-mastectomy breast procedures; 362: mastectomy procedures; 385: other diseases of the skin, subcutaneous tissue and breast; n = number of patients.
Regarding safety, 2 patients experienced bronchospasm during surgery: one (0.4%) in the MAS protocol group and 1 (1.1%) in the hospitalized group. The incidence rates of postoperative adverse events were 1.1% (3/271) and 4.3% (4/93) in group 2 and group 1, respectively (mean difference: 3.2%; 95% confidence interval: −6.5% to 0.0%; P = .0553).
In 2020 and 2021, the situation caused by the COVID-19 pandemic forced us to implement changes in our habitual healthcare practices, and MAS has since become a widely used protocol.
Outpatient surgery in BC has proven to be a feasible and safe strategy for more than 2 decades.4 In recent years, MAS has become increasingly popular and is now considered standard care for oncoplastic breast surgery in benign pathologies.5 However, certain surgical procedures, such as mastectomy, lymphadenectomy, and breast reconstruction (which often require drains to prevent seroma formation), have not been conventionally included in outpatient surgical protocols.
According to the results of the current study, the rates of inpatient BC procedures were high in 2018 and 2019. In fact, the number of outpatient mastectomies was 0 in both 2018 and 2019, versus 59 in 2020 (March 16 to December 31, 2020).
Before March 2020, patients were admitted to surgical units for 24 h when they required drains or were elderly. Nevertheless, when these patients were included in the MAS program, they were discharged on the same day of surgery. This strategy translated into lower use of beds, both in mastectomy-type surgery (−0.35 beds per day) and in breast-conserving surgery that were associated with AL (−1.57 beds per day), with no increase in the number of postoperative complications.
Since no satisfaction surveys were carried out, we subjectively observed that patients (especially elderly patients) welcomed this program, probably because it did not modify their routine and they felt supported by their family.
Regarding safety, the results of the current study show that the MAS protocol is a safe strategy for patients with BC. Although there was a trend toward a lower rate of adverse events in the MAS protocol compared to inpatient programs, the difference was not statistically significant (difference of means: 3.2%; 95% confidence interval: −6.5% to 0,0%; P = .0553).
During the pandemic, MAS for breast surgery, including patients with drains, has been a safe and effective alternative used to maintain surgical treatment.
Some limitations of this study must be considered. The first, which in our opinion is the most important, is the fact that this is a single-center study, so it only reflects the reality of a specific public healthcare area. The second limitation is the lack of surveys to objectively assess the opinions of patients.
FinancingThis research has not received aid from public sector agencies, sector commercial or non-profit entities.
Conflict of interestsThe authors declare that they have no conflict of interest.
Ethical considerationsAll patients offered consent for data collection. The information of the patients included in our work has been treated anonymously and confidentially. The database generated by our unit is only accessible by members of the research team, being protected from uses not permitted by people outside the research.
The treatment, communication and transfer of personal data of all participants complies with the provisions of Organic Law 3/2018 of December 5 on the Protection of Personal Data and guarantee of digital rights and following the bioethics rules of the World Medical Association's Helsinki declaration on ethical principles for medical research.