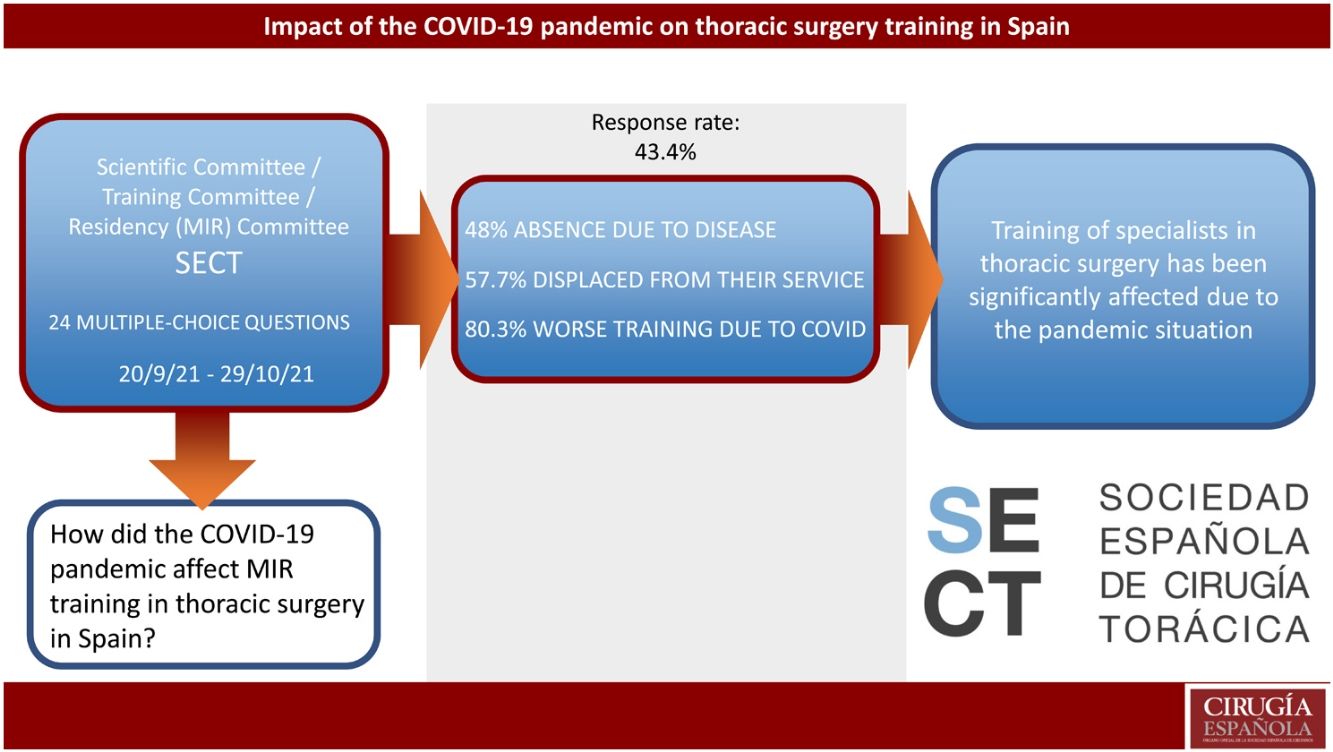
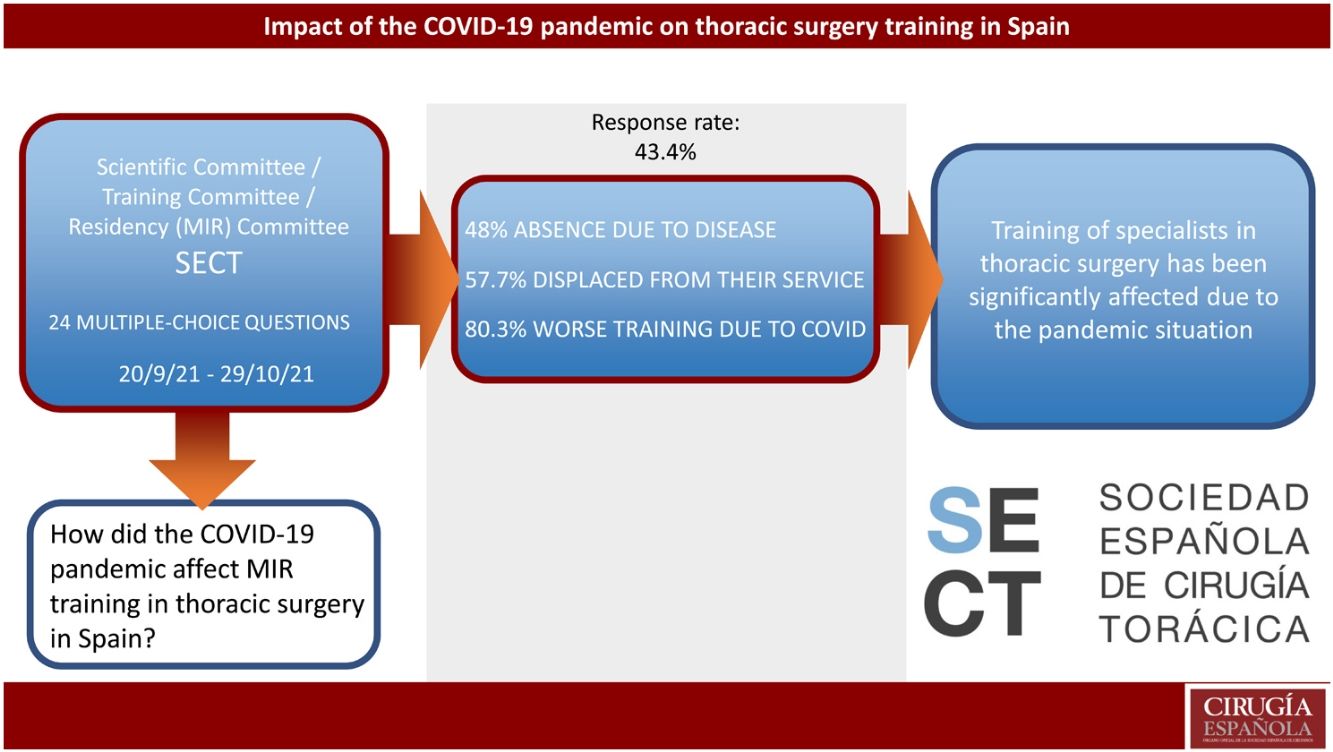
In the more than 2 years since its emergence, the SARS-CoV-2 pandemic has prompted important changes in healthcare systems and their organization. The aim of this study is to determine the implications in specialized thoracic surgery training as well as the repercussions on thoracic surgery residents. With this objective, the Spanish Society of Thoracic Surgery has conducted a survey among all its trainees and those who had finished their residency during the last 3 years. It consisted of 24 multiple-answer closed questions about the impact of the pandemic on their services, their training, and their personal experience. The response rate was 42% (52 out of a target population of 120). The effect of the pandemic on thoracic surgery services was high or extreme according to 78.8% of the participants. Academic activities were completely cancelled in 42.3% of the cases, and 57.7% of the respondents were required to treat hospitalized COVID patients (25% part-time, and 32.7% full-time). More than 80% of the survey participants believed that changes during the pandemic negatively affected their training, and 36.5% would prefer to extend their training period. In sum, we observe how the pandemic has had deep negative effects on specialized training in thoracic surgery in Spain.
Tras más de dos años desde su aparición, la pandemia por SARS-CoV-2 ha generado importantes cambios en la sanidad y su organización. El presente trabajo trata de dilucidar las implicaciones de estos en la formación especializada de la cirugía torácica y sus repercusiones en los profesionales en formación. Para ello, desde la Sociedad Española de Cirugía Torácica se distribuye una encuesta entre los residentes en activo y aquellos que han terminado su formación en los últimos 3 años. Esta consta de 24 preguntas cerradas de respuesta múltiple sobre el impacto de la pandemia en sus servicios, su formación y su vivencia. La tasa de respuesta de la encuesta fue del 42% (52 de una población objetivo de 120). El efecto de la pandemia en el funcionamiento de los servicios de cirugía torácica fue considerado alto o extremo según 78.8% de los participantes. Las actividades académicas fueron completamente suspendidas en 42.3% de los casos, mientras que el 57.7% de los participantes tuvieron que prestar atención asistencial a pacientes ingresados por COVID, de los cuales el 25% fue a tiempo parcial y 32,7% a tiempo completo. De los encuestados, el 80% consideró que los cambios sufridos durante la pandemia afectaron su formación como residente y 36.5% opinó que debería ofrecerse una prolongación del periodo de formación para quienes se hayan visto afectados. Así pues, observamos cómo la pandemia ha afectado profundamente de forma negativa la formación especializada en cirugía torácica en España.
The pandemic caused by SARS-CoV-2 has caused very important changes and problems in all aspects of life, but perhaps the most affected area has been healthcare. In a matter of weeks, an entire system that was not prepared for such a situation had to be adapted to provide the best possible response to a global health emergency.1
Entire medical specialties had to be reorganized to correctly prioritize the pathology, while also attempting to minimize the impact of the extreme levels of hospital occupation by patients with respiratory infection (up to 105% in some hospitals, or 300% in intensive care units)2 as well as its effect on patients with other non-delayable pathologies.3,4
For each medical department, this reorganization meant redistributing staff to other departments (emergency care, intensive care, respiratory care, etc.).5 Obviously, this had professional effects on all staff members of these services. However, at such a demanding time, if there was one thing that was negatively affected by these changes, it was the training of undergraduates (who in fact had to leave hospitals) as well as postgraduate training for resident doctors (in Spain, known as médico interno residente, or MIR).
Training in thoracic surgery was no exception. To assess the impact of the pandemic on the training of thoracic surgery residents (MIR) in our country, the Spanish Society of Thoracic Surgery (Sociedad Española de Cirugía Torácica or SECT) created a survey for residents and young attendings. The objective of the survey was to determine this group’s perception of how their training had been affected since the onset of COVID measures.
MethodsThe survey was designed by the Scientific, Training and MIR committees of the SECT and implemented on the SurveyMonkey online platform. The inclusion criteria of the survey participants were that they were SECT members during their formative MIR stage, or that they had finished their residency in the 3 years prior to the survey. An initial invitation was sent via email on September 29, 2021 to a total of 120 people. The survey was kept open for approximately one month (09/20/21–10/29/21), during which time 2 reminders were sent by email (09/23/21; 10/06/21 ) and text messages were sent on 5 other occasions (09/25/21; 09/29/21; 10/05/21; 10/21/21; 10/22/21).
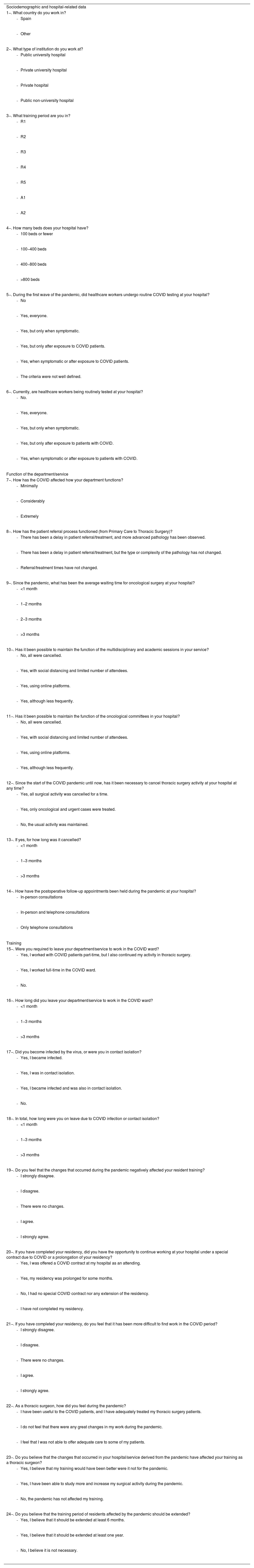
The survey consisted of 24 multiple-choice questions divided into 3 sections: demographic information, organization and operation of each department during the pandemic, and a last one on the perceived impact on academic training. The survey questions are listed in Table 1.
Administrative data.
| Sociodemographic and hospital-related data |
| 1−. What country do you work in? |
|
|
| 2−. What type of institution do you work at? |
|
|
|
|
| 3−. What training period are you in? |
|
|
|
|
|
|
|
| 4−. How many beds does your hospital have? |
|
|
|
|
| 5−. During the first wave of the pandemic, did healthcare workers undergo routine COVID testing at your hospital? |
|
|
|
|
|
|
| 6−. Currently, are healthcare workers being routinely tested at your hospital? |
|
|
|
|
|
| Function of the department/service |
| 7−. How has the COVID affected how your department functions? |
|
|
|
| 8−. How has the patient referral process functioned (from Primary Care to Thoracic Surgery)? |
|
|
|
| 9−. Since the pandemic, what has been the average waiting time for oncological surgery at your hospital? |
|
|
|
|
| 10−. Has it been possible to maintain the function of the multidisciplinary and academic sessions in your service? |
|
|
|
|
| 11−. Has it been possible to maintain the function of the oncological committees in your hospital? |
|
|
|
|
| 12−. Since the start of the COVID pandemic until now, has it been necessary to cancel thoracic surgery activity at your hospital at any time? |
|
|
|
| 13−. If yes, for how long was it cancelled? |
|
|
|
| 14−. How have the postoperative follow-up appointments been held during the pandemic at your hospital? |
|
|
|
| Training |
| 15−. Were you required to leave your department/service to work in the COVID ward? |
|
|
|
| 16−. How long did you leave your department/service to work in the COVID ward? |
|
|
|
| 17−. Did you become infected by the virus, or were you in contact isolation? |
|
|
|
|
| 18−. In total, how long were you on leave due to COVID infection or contact isolation? |
|
|
|
| 19−. Do you feel that the changes that occurred during the pandemic negatively affected your resident training? |
|
|
|
|
|
| 20−. If you have completed your residency, did you have the opportunity to continue working at your hospital under a special contract due to COVID or a prolongation of your residency? |
|
|
|
|
| 21−. If you have completed your residency, do you feel that it has been more difficult to find work in the COVID period? |
|
|
|
|
|
| 22−. As a thoracic surgeon, how did you feel during the pandemic? |
|
|
|
| 23−. Do you believe that the changes that occurred in your hospital/service derived from the pandemic have affected your training as a thoracic surgeon? |
|
|
|
| 24−. Do you believe that the training period of residents affected by the pandemic should be extended? |
|
|
|
After obtaining the data provided by the questionnaire respondents, a descriptive statistical analysis was performed with the platform offered by the SurveyMonkey online survey software. Results were given in absolute numbers and percentages.
ResultsThe survey was sent to a total of 120 SECT members who met the aforementioned inclusion criteria, 52 of whom responded, for a response rate (RR) of 43.3%.
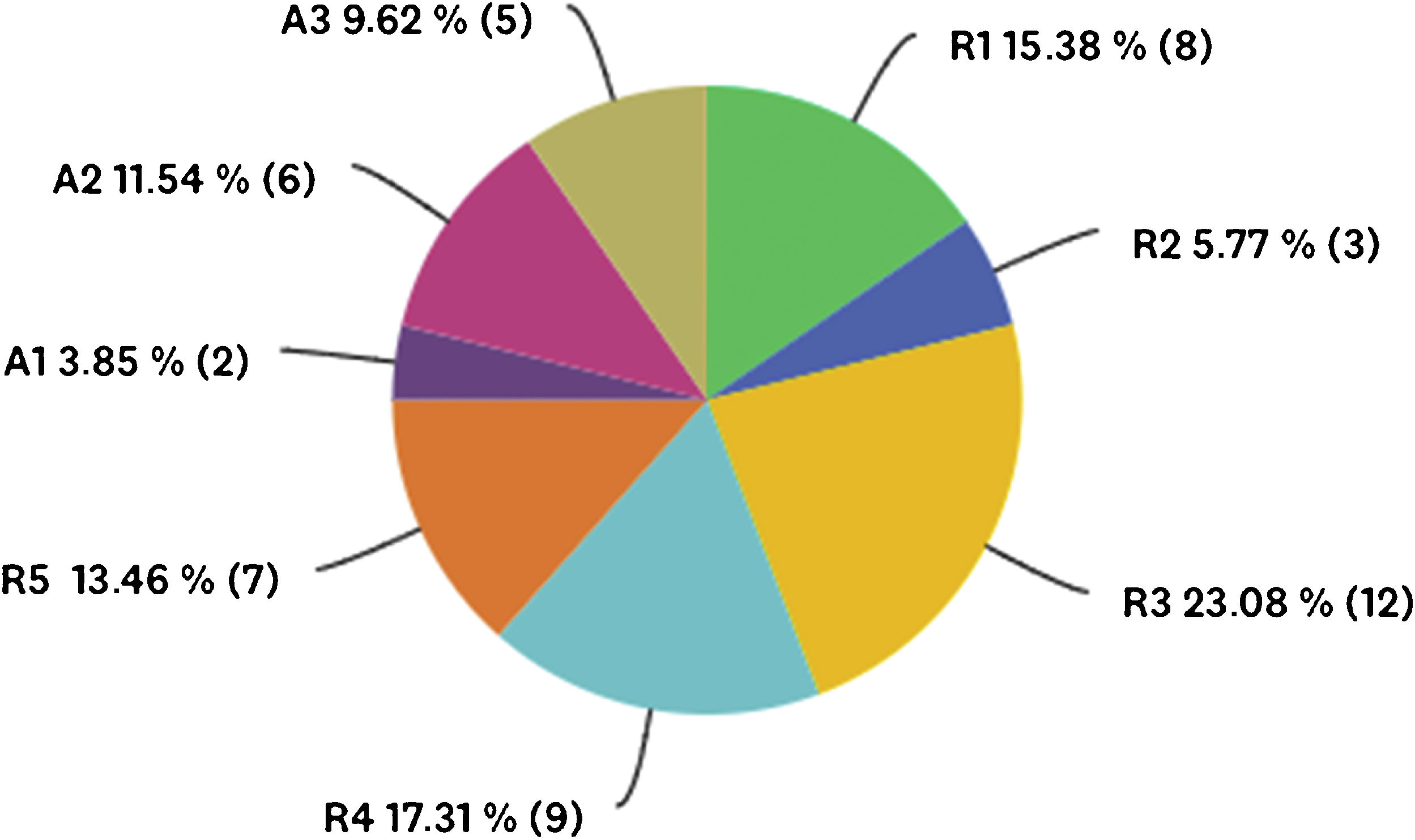
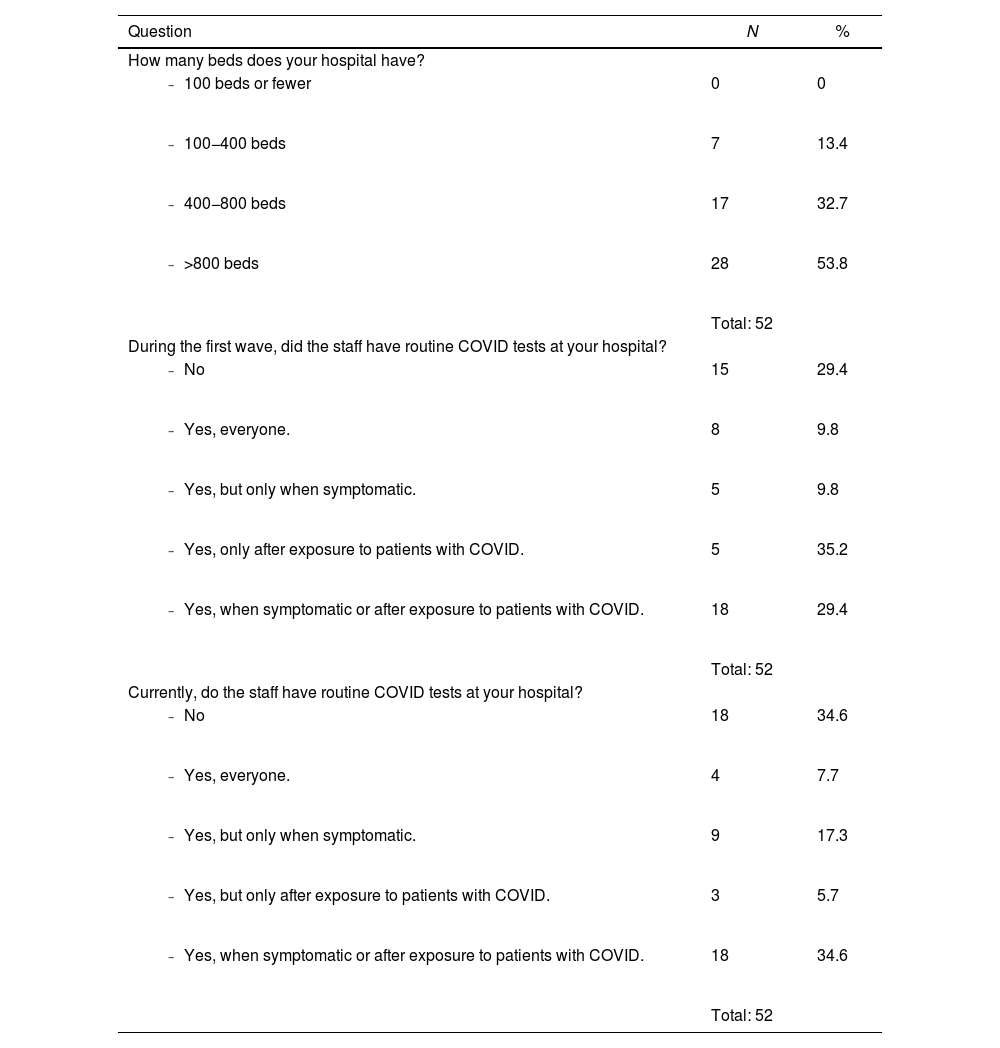
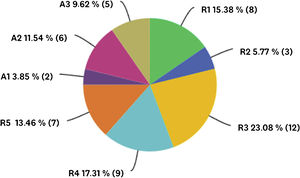
Sociodemographic and hospital-related data100% (52/52) of the respondents answered the sociodemographic questions. At the time of the survey, all of them worked in Spain and at university hospitals, most of which were large (more than 400 beds). The sample obtained was fairly uniform in terms of years of residency and attending experience (Fig. 1, Table 2).
Administrative data.
| Question | N | % |
|---|---|---|
| How many beds does your hospital have? | ||
| 0 | 0 |
| 7 | 13.4 |
| 17 | 32.7 |
| 28 | 53.8 |
| Total: 52 | ||
| During the first wave, did the staff have routine COVID tests at your hospital? | ||
| 15 | 29.4 |
| 8 | 9.8 |
| 5 | 9.8 |
| 5 | 35.2 |
| 18 | 29.4 |
| Total: 52 | ||
| Currently, do the staff have routine COVID tests at your hospital? | ||
| 18 | 34.6 |
| 4 | 7.7 |
| 9 | 17.3 |
| 3 | 5.7 |
| 18 | 34.6 |
| Total: 52 |
Question 7.How do you think the COVID pandemic has affected the operation of your department? (TR: 52/52; 100%)
Most of those surveyed considered that the operation of their department was “considerably” affected by the pandemic (n = 35; 67.3%), while 11.5% (n = 6) believed that the impact was “extreme”, and 21.1 % (n = 11) stated that their service has been “minimally” affected (Table 3).
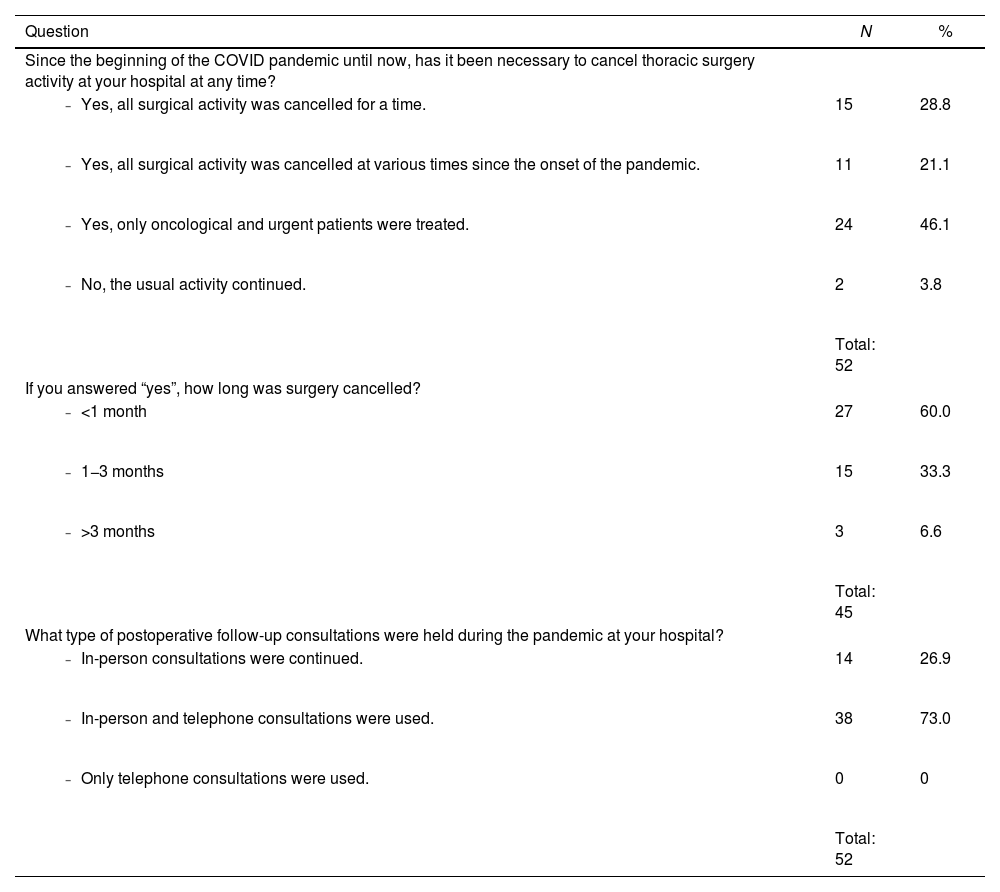
Surgical data.
| Question | N | % |
|---|---|---|
| Since the beginning of the COVID pandemic until now, has it been necessary to cancel thoracic surgery activity at your hospital at any time? | ||
| 15 | 28.8 |
| 11 | 21.1 |
| 24 | 46.1 |
| 2 | 3.8 |
| Total: 52 | ||
| If you answered “yes”, how long was surgery cancelled? | ||
| 27 | 60.0 |
| 15 | 33.3 |
| 3 | 6.6 |
| Total: 45 | ||
| What type of postoperative follow-up consultations were held during the pandemic at your hospital? | ||
| 14 | 26.9 |
| 38 | 73.0 |
| 0 | 0 |
| Total: 52 |
Question 8.How has the process for referring patients to thoracic surgery from primary care centers functioned? (TR: 52/52; 100%)
In total, 76.9% (n = 40) stated that the delay in care and referral of patients increased significantly, and more patients with advanced pathology were being seen in the consultation and emergency rooms. Another 7.7% (n = 4) responded that the referral time increased with no change in the degree of complexity of the pathology, and 15.4% (n = 8) observed no change.
Question 9.Since the pandemic, what has been the average waiting time for cancer surgery at your hospital? (TR: 52/52; 100%)
Waiting times of less than one month were reported in 23% of the cases (n = 12), between 1 and 2 months in 40.4% (n = 21), between 2 and 3 months in 32.7% (n = 17) and more than 3 months in 2 cases (3.8%). Other care factors can be found in Table 3.
Question 10.Has it been possible to keep the multidisciplinary and academic sessions going in your department? (TR: 52/52; 100%)
Frequently, all activities had been suspended (n = 22, 42.3%), while maintaining a certain degree of activity with social distancing and fewer attendees in many (n = 15, 28.8%), or using online platforms (n = 7, 13.4%), or reduced frequency (n = 8, 15.3%).
Question 11.Have the cancer committees continued functioning in your hospital? (TR: 52/52; 100%)
Most survey participants (n = 48, 92.3%) answered that these activities continued to be carried out at their hospitals while applying safety measures: social distancing and limited attendees (n = 24, 46.1%), online platforms (n = 23, 44.2%), or less frequent meetings (n = 1, 1.9%).
Data related to the academic training of residents during the pandemicQuestion 15.Did you have to leave your department to cover the COVID hospital ward? (TR: 52/52; 100%)
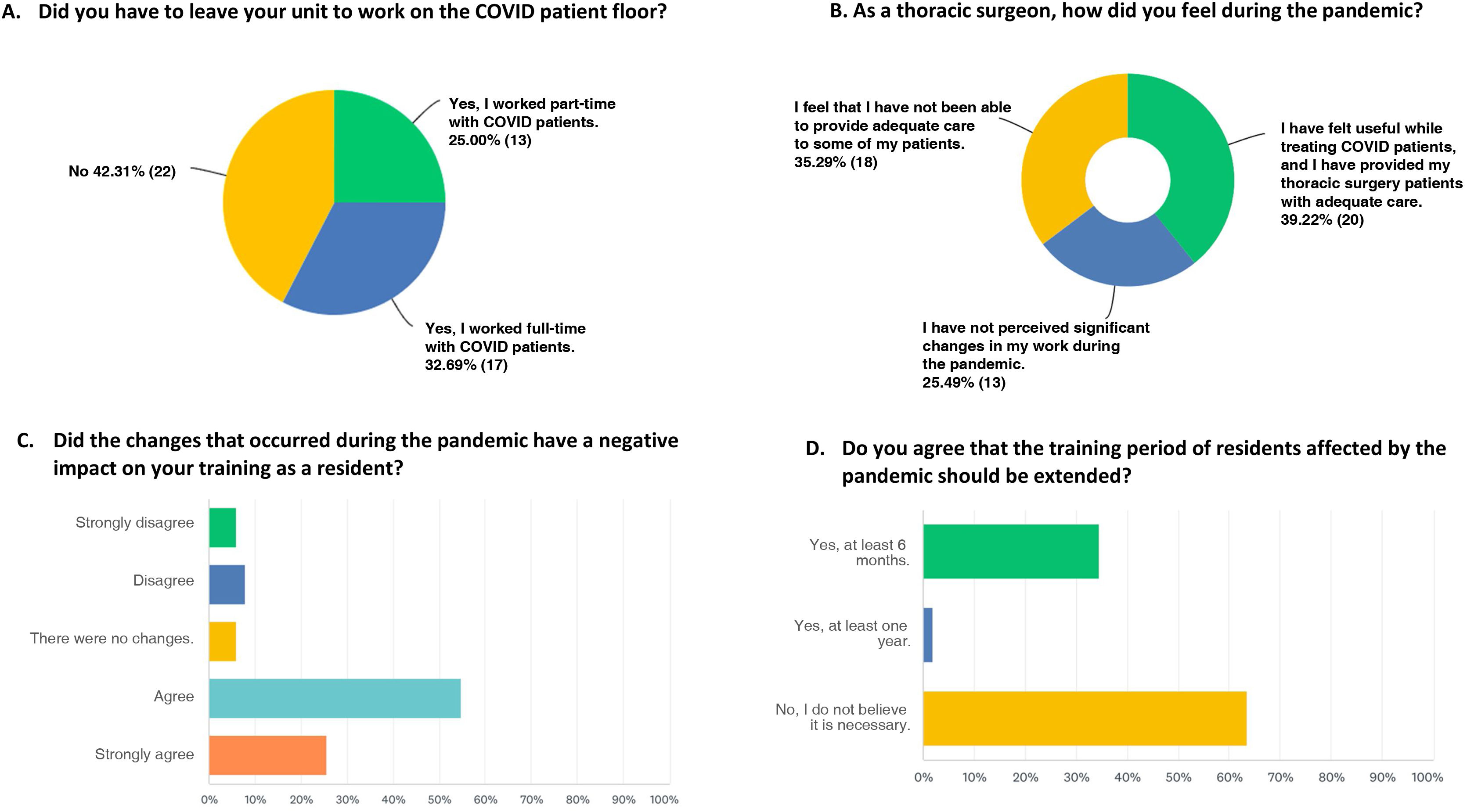
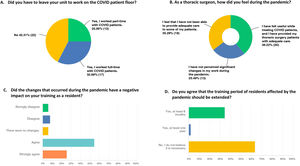
In total, 57.7% (n = 30) of the survey respondents had to temporarily leave their department to work with patients in the COVID-19 unit of their hospital, and more than half of these (n = 17) provided medical care to this group of patients on a full-time basis. In contrast, 22 respondents (42.3%) did not have to leave their service at any time during the pandemic (Fig. 2A).
Graphic representation of the responses to the following questions: A) Did you have to leave your unit to work on the COVID patient floor?; B) As a thoracic surgeon, how did you feel during the pandemic?; C) Did the changes that occurred during the pandemic have a negative impact on your training as a resident?; D) Do you agree that the training period of residents affected by the pandemic should be extended?
Question 16.How long were you out of your department to provide COVID assistance? (TR: 38/52; 73%)
Some 68.4% (n = 26) provided services outside their usual position for less than a month, 31.6% (n = 12) for one to 3 months and none for more than 3 months.
Question 17.Did you contract the virus or require contact isolation? (TR: 52/52; 100%)
Some 48% of those surveyed had been on sick leave; 23.0% (n = 12) had contracted COVID-19 infection at the time of the survey, while 25.0% (n = 13) had been in contact isolation. One participant had had one infection as well as a separate contact isolation (1.9%).
Question 18.In total, how long were you out due to COVID/contact isolation? (TR: 51/52; 98%)
Approximately half of those surveyed (49.02% n = 25) were forced to take a leave, either due to infection or due to contact with the virus. In 45.1% (n = 23), the leave was for less than a month, one respondent (1.9%) between one and 3 months, and another (1.9%), for more than 3 months.
Question 19.Do you feel that the changes that occurred during the pandemic have affected your training as a resident? (TR: 51/52; 98%).
The vast majority of respondents (n = 41, 80.3%) indicated that the pandemic has had a detrimental impact on their training as a resident, while the rest perceive that there have been no major changes (Fig. 2C).
Question 20. If you have finished your residency, did you have the opportunity to continue working at your hospital with a special contract due to COVID or extended residency? (TR: 46/52; 88.4%)
Out of the 11 respondents who had completed their resident training during the COVID period, only 2 received a job offer with a “COVID contract” at their hospital, while the remaining 9 did not receive a job offer or the option to extend their residency.
Question 21.If you have finished your residency, do you think it has been more difficult to get a job in the COVID era? (TR: 32/52; 61.5%)
Five of those surveyed (n = 5, 15.6%) believe that the pandemic has reduced the chances of finding a job after completing their residency. However, the majority of those who responded believe that there have been no changes (n = 27, 84.4%).
Question 22.How have you felt as a thoracic surgeon during the pandemic? (TR: 51/52;
More than one-third of those surveyed say they have not felt at ease with their work during the pandemic (18 respondents, 35.3%). In contrast, 25.5% (n = 13) reported not noticing changes in their work, while 20 participants (39.2%) are satisfied with their work performance during the pandemic (Fig. 2B).
Question 23.Do you believe that the changes in your hospital/department caused by the pandemic have affected your training as a thoracic surgeon? (TR: 51/52; 98%).
Most respondents (n = 41, 80.4%) believe that the pandemic has negatively affected their training as thoracic surgeons, while only 19.6% (n = 10) do not feel that their training would have been different under other circumstances.
Question 24.Do you think that the training time for residents affected by the pandemic should be extended? (TR: 52/52; 100%)
Nineteen (36.5%) survey participants believe that the training time should be extended. Among them, only one (1.9%) considers that the extension should be one year, while the rest indicate that 6 months would be sufficient. In contrast, 63.5% (n = 33) of the participants do not believe that any type of prolongation is necessary (Fig. 2D).
DiscussionThe outbreak of the SARS-CoV-2 pandemic in an unprepared world affected all daily activities. In healthcare, however, it generated the equivalent of a tsunami, with more than 758 million infected patients and more than 6.8 million deaths worldwide at the time of this writing,6 which saturated entire healthcare systems, forcing them to be restructured.7
The effect of the pandemic on thoracic surgery was very notable, especially given that the main volume of this specialty is the treatment of lung cancer, a pathology whose treatment cannot be delayed.8 Across Europe, there was a general decrease in surgical volume, as well as in multidisciplinary meetings and tumor committees for the treatment of lung cancer.9 In Spain, the effects were even greater in many cases, as our country was one of the most affected by the first wave of the virus.10 All this had an obvious impact on all members of thoracic surgery departments, although especially on specialists in training.
In Spain, the vast majority of thoracic surgeons in training feel that their residency education has been negatively affected by the pandemic situation (80.3%). This is an opinion common to all countries. In fact, the most common complaint among specialists in training around the world is the notably reduced volume of pathology (meaning that they have acquired less experience) as well as the inability to conduct training sessions. As a result, the training objectives of their residency have not been met.11 In fact, this effect has been especially notorious in surgical specialties from the moment that operating room activity was radically reduced.12
Added to the decrease in surgical volume is the fact that many residents also lost training time when they became infected or were isolated due to being in contact with an active case. In addition, many specialists in training were required to work in departments that were completely different from their trained specialty. In our series, more than half of those surveyed faced this situation, which is in line with the figures reported by the same surgical specialties in other countries (both European13 and Ibero-American).14 In total, certain studies have calculated a 75%–100% drop in involvement of residents in their service versus what they would have experienced without the pandemic.15
This entire situation has generated problems not only in the training itself, but also at the psychological level of these residents, causing burnout and concern for their well-being.1112 In fact, more than 35% of survey participants stated that they did not feel at ease due to what they considered to be deficient care that they were forced to offer their patients. In addition, they declared an added concern of feeling poorly trained and unprepared as surgeons, even wanting their training period to be extended. This possible extension has not occurred in our sample, and the recently finished residents have been launched into a job market that some consider more complex due to this defect in their training. In fact, this fear of incomplete training is something that has been seen consistently in studies published about the effect of the pandemic on residents of surgical specialties13,16 and is likewise shared by directors of residency programs.17
This study gives an overview of the repercussions brought about by the general restructuring of the Spanish healthcare system during the pandemic, based on data from an open survey of all thoracic surgery specialists in training and those who finished their residency during the pandemic. The study has limitations, such as the fact that it uses questions with closed answers, or the fact that the survey was conducted more than one year after the peak of the pandemic. This latter factor may provide greater perspective, but it may also generate a recall bias. Furthermore, this study has obtained a satisfactory sample of the target population (43.3% of the total), with a fairly consistent representation of the residents from different years and attendings, so we can conclude that the sample is representative.
ConclusionsThe COVID-19 pandemic devastated the entire healthcare structure worldwide and especially in our country, which was one of the most affected. And in all this reorganization brought on by necessity, one of the most overlooked yet affected facets of the healthcare system was the training of resident doctors. As a result, specialists have completed their residency with partially deficient training and would have likely benefited from an extension of their residency program.