In the last decades there has been an increase in allergic disease throughout the world, particularly in children. Attempts have been made to identify the causes of this “allergy epidemic” in environmental changes and changes in population hygiene, lifestyle, socioeconomic level, and eating habits that would exert epigenetic effects.
Dietetic hypotheses have been mainly focussed in long-chain polyunsaturated fatty acids, vitamin D, antioxidants, Mediterranean diet, and fruits, vegetables and fish consumption. Although the data suggest a certain association between diet and the development of asthma/allergy, there is no evidence that diet has an impact upon the prevalence of such diseases after early infancy. If indeed there is such an impact, it is likely to be confined to the prenatal period and the first months of life – when it is still possible to modulate the development of the respiratory, digestive and immune systems. Thus, once the most appropriate preventive measures have been defined, these should be implemented during pregnancy and lactation.
The existing scientific evidence is unable to recommend any primary preventive measure in the general population or in different population subgroups. Special or restrictive diets in pregnant or nursing women are not indicated. Exclusive breastfeeding for six months is questioned, since solid foods should begin to be introduced at around four months of age. Once the atopic process has started, no nutritional strategies have been found to be effective as secondary or tertiary preventive measures. Longitudinal studies in cohorts of pregnant women or newborn infants could help clarify these issues.
The aetiology of asthma and atopic diseases is multifactorial, with complex interactions between genetic and environmental factors that give rise to the resulting phenotypical manifestation of the disease. In the last 50 years there has been an increase in allergic disease throughout the world, with an estimated prevalence of 40% in children,1 giving rise to what has been referred to as an “allergy epidemic”. Since it is not possible for relevant changes in the genetic profile of the population to have developed in such a short period of time, attempts have been made to identify the causes of this increase in environmental changes (infections, pollution, climate, pneumoallergen and food allergen exposure, etc.) and changes in population hygiene and eating habits, socioeconomic level and lifestyle, amongst other factors with epigenetic effects.2,3 Amongst these factors, special mention must be made of the dietetic changes associated with the transition from a traditional to a modern diet,4 in which foods are processed to allow for longer preservation, and salt, refined sugar and saturated fat consumption has increased. Besides, the modern western lifestyle is associated with sedentarism, obesity, fast food restaurants, and a decrease in the consumption of fruit and vegetables, milk (which moreover is consumed in ultra-pasteurised form), dietary fibre and foods rich in vitamins and antioxidants.5 The “dietetic hypothesis” has two major paradigms in the beneficial effects found amongst children who follow traditional eating habits, such as those living on farms6 or in families with an anthroposophic lifestyle.7
Attempts to apply the concept of asthma as a nosologic unit or entity have failed, because there are different disease phenotypes with different denominations. In preschool children it is particularly difficult to distinguish between an incipient allergic phenotype and wheezing due to some other cause; as a result, a European panel of pediatricians8 has recently recommended avoiding the diagnosis of asthma in this age group, since there is no evidence that its physiopathology is similar to that of asthma found in older children and in adults. In this context, the term “recurrent wheezing” is preferred.
Since it is presently not possible to modify the genetic factors, the development of a rational primary asthma and allergy prevention strategy must include identification of and action upon environmental factors – amongst which nutritional factors stand out. The prenatal period and the early stages of extrauterine life are crucial for establishing preventive strategies, since it is in this period of time when maturation of the immune system and of other body systems is completed. In this sense, different stimuli (nutrition, smoking, infections) can mark the newborn infant for life with an adequate Th1/Th2 cell balance, or with a predominance of Th2 activity characteristic of atopic individuals, which will favour the appearance of allergy. There is evidence in the newborn infant of a T-cell response to environmental antigens before any direct exposure to such antigens has occurred,9,10 starting from week 22 of gestation.11
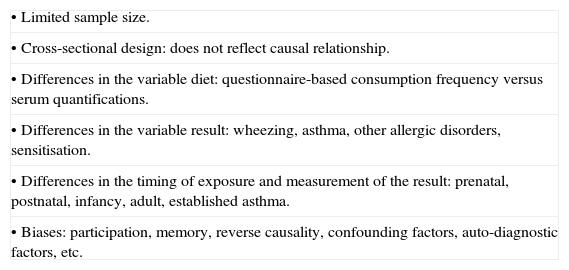
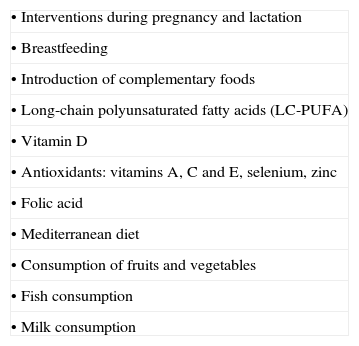
Prevention and treatment of asthma and allergy through dietetic interventionsIn general, the body of evidence drawn from observational studies seeking associations between diet and asthma/allergy is small due to the limitations of these studies (Table 1). The ideal situation would be to have randomised, double-blind, placebo-controlled prospective studies, taking into account confounding factors associated with asthma/allergy, such as an increased socioeconomic level, which can be associated to more healthy habits and increased collaboration in studies. It must also be mentioned that the different dietetic hypotheses (Table 2) would not be valid for all population subgroups. It is in the early stages of life (pre- and postnatal) when intervention opportunities arise, due to the immaturity of the respiratory, digestive and immune systems, and it is here when the study of the relationship between diet and asthma is most interesting, since it is still possible in this critical period to modulate the growth and development of the mentioned body systems – with repercussions for the entire subsequent lifetime of the individual.
Possible defects, biases and methodological differences of the epidemiological studies.
| • Limited sample size. |
| • Cross-sectional design: does not reflect causal relationship. |
| • Differences in the variable diet: questionnaire-based consumption frequency versus serum quantifications. |
| • Differences in the variable result: wheezing, asthma, other allergic disorders, sensitisation. |
| • Differences in the timing of exposure and measurement of the result: prenatal, postnatal, infancy, adult, established asthma. |
| • Biases: participation, memory, reverse causality, confounding factors, auto-diagnostic factors, etc. |
Dietetic hypotheses.
| • Interventions during pregnancy and lactation |
| • Breastfeeding |
| • Introduction of complementary foods |
| • Long-chain polyunsaturated fatty acids (LC-PUFA) |
| • Vitamin D |
| • Antioxidants: vitamins A, C and E, selenium, zinc |
| • Folic acid |
| • Mediterranean diet |
| • Consumption of fruits and vegetables |
| • Fish consumption |
| • Milk consumption |
Physiologically, pregnancy is characterised by Th2 cell polarisation or predominance that counters the Th1 responses that prove toxic for the placenta,12 thereby avoiding miscarriages as a result of immune rejection. After delivery, however, a shift towards Th1 responses is observed as a consequence of successive microbial stimuli that afford protection against germs, with a lessening of the Th2 reactivity responsible for allergic processes. A number of publications13–15 have related complications during gestation and delivery to a lesser risk of rhinitis and asthma. The situation could be the opposite, however, i.e., allergic women may have fewer gestational complications, fewer miscarriages and a larger number of pregnancies16,17 – atopy being more frequent in infants born to term or post-term than in premature infants.18
Different preventive interventions have been proposed to reduce the impact of asthma/allergy in infancy, such as maternal dietetic restriction during pregnancy and lactation, the encouragement of natural breastfeeding, the use of hypoallergenic formulas in children that cannot be breastfed, and a delay in the introduction of some foods.19–21 Double-blind, placebo-controlled studies have shown that the avoidance of food allergens during pregnancy does not lessen the risk of allergy22; in this sense, there is no evidence for recommending exclusion diets in pregnant women, as they are not seen to be effective and may pose a nutritional risk for the mother and foetus.23
Supplementing pregnant women with vitamins E24,25 and D,26,27 zinc,24 selenium and iron,28 fish29,30 and apples31 have been suggested as protective factors against the development of asthma or allergy in the offspring. On the other hand, a longitudinal study found no association between the consumption of vegetables, fish, eggs or dairy products in pregnant women and parameters of asthma in the offspring between 1 and 8 years of age.31
Gestational age and birth weightA cross-sectional study with ISAAC methodology conducted in 1138 German schoolchildren between 5 and 7 years of age recorded a directly proportional relationship between atopic sensitisation and gestational age, with similar findings between the IgE levels and body weight at birth.32 Obesity, with an important genetic burden, has been related to asthma, although it is not clear whether obesity is a mere triggering factor, a risk factor, a consequence, or whether it develops parallel to asthma.33
Immaturity increases the theoretical risk of allergic diseases in premature subjects, which paradoxically have a lesser incidence of allergic disorders.34 This tolerance could be explained by a combination between high concentrations of antigen on one hand and digestive and immune immaturity on the other.35 In contrast, prematurity increased risk of non-allergic pulmonary disease as a consequence of lung and immune immaturity – with great importance on the part of infections and exposure to tobacco smoke.
BreastfeedingA meta-analysis of prospective studies suggests that exclusive breastfeeding for at least four months is associated with a lesser rate of asthma in infancy, with a greater impact in children presenting antecedents of atopy.36 However, these data could simply reflect a protective effect of breastfeeding against respiratory infections, which are the main triggering causes of wheezing in preschool children. It has also been suggested that breastfeeding prevents allergic processes only in children without antecedents of allergy, but not in those with familial atopy.37 This could be explained through reverse causality: these would be children with mothers who are more aware of the protective effects of breastfeeding, and who thus prolong breastfeeding as far as possible. The use of partially hydrolysed infant formulas has only shown usefulness in preventing the development of allergies in children at high risk (those with at least one allergic first-degree relative) – the number needed to treat in order to prevent a case of cow's milk protein allergy being 25, and such benefit moreover does not increase with extensive hydrolysates or soya formulas.38
Introduction of solid foodsThe ingestion of high amount of food allergen during the first year of life can promote tolerance, whilst small and intermittent doses can induce sensitisation. This questions the appropriateness of recommending exclusive breastfeeding up to six months of age39 and the late introduction of solid foods.34 Indeed, such measures may even prove harmful.40,41 In a systematic review,21 Tarini et al. found that delays in introducing foods other than breast milk or formulas could exert a beneficial effect upon atopic dermatitis, but not on the rest of allergic disorders or upon sensitisation to both pneumoallergens and trophoallergens, which could develop via the topical route through eczematous lesions.42,43
Intestinal flora. Use of probiotics and prebioticsUntil recently, interventions designed to prevent asthma and allergy concentrated on reducing exposure to the allergen during pregnancy and lactation. Other measures, such as the use of probiotics and prebiotics, aimed to develop tolerance mechanisms through modification of the immune response of the foetus or nursing infant, whose intestine is sterile at the time of birth. Establishment of the intestinal microflora is crucial for modulating immune system maturation in the newborn infant44 – different studies have shown qualitative and quantitative differences depending on the type of delivery involved or the presence or absence of breastfeeding.45–47 The intestinal microbiota of allergic children is characterised by a predominance of Clostridium difficile,48 coliform strains and Staphylococcus aureus,49 whilst a greater presence of Lactobacillus is found in non-allergic49 and in anthroposophic infants.50 Different studies have reported different results regarding the effects of probiotics provided in the last weeks of pregnancy and in the first few months of life, as a protective measure against allergic processes, particularly atopic dermatitis.51–54 On the other hand, the provision of prebiotics during the first six months of life has been shown to afford protection against allergic symptoms and infections up to two years of age.55 However, a recent positioning document of the Nutrition Committee of the ESPGHAN does not support routine supplementing with prebiotics and probiotics in infant formulas, and underscores that the safety and efficacy data of one product are not extrapolatable to other products.56
Long-chain polyunsaturated fatty acids (LC-PUFA)Since LC-PUFAs cannot be synthesised by the body, they must be obtained from the diet. These fatty acids are incorporated to the cell membrane phospholipids, where they exert a number of functions, including modulation of the immune and inflammatory responses. There are two major groups of LC-PUFAs: omega-3, derived from α-linolenic acid (found in plants, soya oil and fish), and which act as the precursors of docosanoids (eicosapentaenoic (EPA) and docosahexaenoic (DHA) acids); and omega-6, derived from linoleic acid (found in corn, soya and sunflower oils and their margarines – the consumption of which has increased in the last few decades), which act as the precursors of eicosanoids (arachidonic acid and its derivatives, i.e., prostaglandins, thromboxanes and leukotrienes).
Some clinical studies have reported beneficial effects with fish oil supplementing in patients with asthma,57–59 whilst others have observed no such effects.60–62 In this context, a meta-analysis concluded that there is little evidence supporting supplementing or increasing the intake of omega-3 in the diet63 as a treatment for already-established asthma in children and adults. Since atopy is programmed in the first months of life, intervention with omega-3 once the allergic process has already become established may be too late to secure benefits. Early exposure to omega-3 may modify the Th1/Th2 profile – higher concentrations of docosanoids and IgA being observed in the milk of nursing women who received omega-3 supplements during pregnancy,64 together with higher serum levels of interferon-gamma (IFN-γ)65 in their offspring. In the CAMP study, fish oil or placebo supplementing was carried out in children at risk of developing asthma from six months of age. A resulting decrease was observed in the prevalence of wheezing, nocturnal cough or the use of bronchodilators at 18 months,66 with no influence upon sensitisation to foods or atopic dermatitis. This protective effect in turn disappeared over follow-up after three and five years.67
In an excellent review, Sala-Vila et al.68 detected numerous inconsistencies in the studies evaluating atopy risk in relation to the LC-PUFA in nursing infants’ serum samples and composition of breast milk from atopic mothers, concluding that it is not possible to establish a clear idea of the role and composition of LC-PUFAs in asthma and allergy based on the existing information. These discrepancies were influenced by the designs of the studies included in the meta-analysis. Overall, the data do not support the pre-existing idea that consumption and high levels of omega-6 and low levels of omega-3 are associated with atopy. On the other hand, emphasis is placed on the importance of the balance between both types of fatty acid, since despite individually some arachidonic acid derivatives may have inflammatory effects, their global action is of an anti-inflammatory nature.68
Vitamin DIt has been suggested that the increase in the prevalence of asthma in the western world is a consequence of vitamin D deficiency69 due to lesser exposure to sunlight. The immune modulating action of vitamin D is known,70 and the immune cells have activating receptors and enzymes for this vitamin.71 A series of cohorts involving newborn infants have reported an association between vitamin D deficiency before birth and in the first months of life and an increased risk of recurrent wheezing, asthma and allergic rhinitis26,27,72 in infancy. This could be attributed to an alteration in the response to viral infections73 – vitamin D having been shown to induce antimicrobial peptides, including cathelicidin, in vitro.74,75 In addition, there is a lesser incidence of influenza in schoolchildren who receive supplements of vitamin D376 – this effect being greater amongst asthmatics. Likewise, a protective association has been described between maternal vitamin D consumption during pregnancy and a lesser risk of developing wheezing in the first years of life,27 as well as asthma and allergic sensitisations in the future.26 Furthermore, in asthmatics, the provision of vitamin D could reduce the number and severity of the exacerbations,77–79 with suggested positive effects upon the corticosteroid action routes.80 Thus, vitamin D would exert primary preventive effects (avoiding the development of wheezing-asthma), secondary preventive effects (reducing disease severity in asthmatics), and also tertiary preventive effects (improving the response to corticosteroid treatment).
In contrast, other authors suggest that an excessive provision of Vitamin D could induce an exaggerated Th2 response, thereby favouring allergic sensitisations.81,82 In one study, vitamin D supplementing during the first year of life was associated to an increased risk of atopy, rhinitis and asthma at 31 years of age,83 although this study did not control for maternal vitamin D levels, possible confounding factors, or memory bias.
AntioxidantsAn association has been suggested between asthma and a diet poor in exogenous antioxidants84,85 such as vitamins A, C and E, and oligoelements such as zinc and selenium – which favour the production of IFN-γ and can attenuate the respiratory epithelial damage caused by free radicals. In 2010, a meta-analysis reported the intake of vitamins A, C and E to be significantly lower in patients with asthma, particularly amongst those with more serious disease.86 Previously, another meta-analysis failed to obtain evidence that antioxidant intake influences the risk of asthma.87 The existing evidence on the beneficial effects of antioxidants, vegetables and the Mediterranean diet is weak, but suggests protection against wheezing and asthma, particularly when applied to pregnant women,88 thanks to the optimisation of lung development89 and the palliation of oxidative damage in this critical period. The biological mechanisms by which these elements may influence childhood asthma could be independent of antioxidant activity, since they are not observed with all of the mentioned elements, and are also recorded with substances lacking antioxidant effects.4
Vitamin AVitamin A (retinol) exerts dual antioxidant action and protective anti-infection effects upon the respiratory tract.90 Children with high serum carotene levels have been found to be less likely to develop asthma91,92 – significant differences being observed in the concentrations of vitamin A between asthmatics and healthy controls.93 In addition, the consumption of vitamins A and C at levels below the recommended daily amounts is associated with a significantly higher prevalence of wheezing in the first years of life and asthma,86 and it has even been reported that the severity of asthma is inversely correlated to the blood levels of vitamin A.91 In contrast, it has not been possible to show that maternal supplementing with beta-carotenes is associated to a lesser risk of wheezing in the first years of life.31
Vitamin EVitamin E (α-tocopherol) is a first-order antioxidant in that it prevents the oxidation of LC-PUFAs and proteins. Moreover, it exerts immune actions by promoting Th1 responses and inhibiting Th2 differentiation.94,95 Maternal levels of vitamin E are a determinant factor for foetal growth, and for lung development and maturation.96 In this sense, there is a significant correlation between prenatal vitamin E intake and a reduction of wheezing in the first two years of life.25,97 Nutritional studies suggest a relationship between oxidative stress and bronchial inflammation; as a result, supplements of vitamin E in asthmatics could help lessen the symptoms98 and improve lung function.99,100
Vitamin CVitamin C (ascorbic acid) is a water-soluble antioxidant found in the airway epithelia and alveoli which is able to attenuate the oxidative damage caused by inhalatory agents, infections or cellular inflammation. In the context of the NHANES III study,92 measurements were made of the serum concentrations of vitamins in children between 6–17 years old. The bivariate analysis showed the diagnosis of asthma to be associated to lower levels of vitamin C, alpha- and beta-carotene, and beta-cryptoxanthin. However, after adjusting the results for possible confounding factors, only vitamin C and alpha-carotene continued to show statistical significance in the resulting logistic regression analysis. It has not been possible to show that an extra intake of vitamin C in pregnant women is able to reduce the risk of posterior wheezing in their offspring,25,97 although an inverse proportional relationship has been described between vitamin C intake and the risk of wheezing,101 bronchial hyperresponsiveness102,103 and FEV1 values.104,105 Despite these findings, two Cochrane reviews concluded that no generalised positive effect can be established, and that there is not enough evidence to support vitamin C supplementing in the treatment of established bronchial asthma.106,107
Folic acidFolic acid participates in nucleotide synthesis, cell division and differentiation, and in DNA methylation, and as such is a key element in foetal development. Some authors108 have described an inverse proportional relationship between folic acid concentrations and the presence of wheezing, atopy and IgE levels in 8083 subjects over two years of age. In contrast, other investigators have related folic acid to negative effects, with the observation of an increased frequency of respiratory and allergic disease in the offspring of women who received folate supplements during pregnancy109,110 – this possibly being linked to an increased risk of respiratory infections during the first months of life.
OligoelementsSeleniumThe role of selenium, acting as coenzyme of glutathione peroxidase, is subject to controversy, for although elevated selenium levels during pregnancy and in umbilical cord blood are associated to a decreased risk of early wheezing in the first two years of life,111 no such effects are seen at five years of age.112 Other studies in turn have reported an association between selenium levels and a decrease in the prevalence of asthma,113 fewer respiratory symptoms,114 and improved lung function.100
ZincZinc intervenes in the metabolism of superoxide dismutase (SOD) and vitamin E. Zinc levels in the hair of wheezing children have been found to be significantly lower than in the controls.115 Although there have been reports of its beneficial effects when supplied during pregnancy25 and in the first years of life,116 the evidence supporting such a recommendation is still weak.
MilkA number of studies have described that a frequent consumption of dairy products amongst pre-school children results in a lesser risk of asthma symptoms in these children.117,118 It is debatable whether this effect is linked to the LC-PUFA contents of milk, in which case it would only be valid for whole and scantly processed milk119 and butter,120 but not for skimmed milk products.
Despite the widespread belief that milk and its products increase airway mucus production; there is no convincing explanation for such an effect. In 2005, a review121 concluded that those individuals with this prior conviction reported perceived changes in mucus production after consuming milk, in contrast to those who did not share this belief. In a double-blind study, the “believers” detected the same increase in secretions both after consuming milk and after consuming a soya beverage with the same organoleptic properties – a situation that could be explained in terms of greater saliva production and thickening.122 It can be concluded that this belief has no scientific basis, and that there is no evidence in support of restricting or avoiding dairy products in asthmatic individuals.
Mediterranean diet. Fruit, vegetables, fish, and olive oilThe Mediterranean diet and frequent fruit consumption in children and pregnant women is associated with a lesser risk of wheezing, asthma and allergy.123–127 Willers et al.31 recorded beneficial effects of apple consumption (but not with total fruit intake) during pregnancy in relation to wheezing and asthma at five years of age. Specific studies addressing concrete foods therefore would be advisable (different fruit species belong to different botanical families with different biological properties). It has been suggested that the consumption of potentially allergenic foods during pregnancy increases the transplacental or transamniotic transmission risk of sensitisation128,129 to trophoallergens and pneumoallergens.130 In adults, the consumption of whole grain bread has been shown to exert a protective effect against asthma,131 although it cannot be ruled out that such consumption, in the same way as with fruit, might be a confounding factor associated to other healthy lifestyle factors.
The evidence on the effect of fish consumption during pregnancy in relation to allergy/asthma is inconclusive – some studies reporting a favourable effect,29,30,130 whilst others report no effect,31 or protective action against atopic dermatitis but not against the rest of allergic disorders.132 On the other hand, from week 30 of pregnancy, a Danish study comparing olive oil versus fish oil capsule supplementing found the offspring of the women in the latter group to have a lesser risk of asthma – although this same effect was observed in a third non-intervened control group.133
ConclusionsFollowing this review of the relationship between diet and asthma-atopy in the first years of life, we can conclude that the nutritional factors responsible for the increase in these diseases are not clear. The discrepancies observed by the different studies are largely attributable to methodological differences (Table 1).
Although the dietetic hypotheses are promising, and there are partial findings associating diet to the development of asthma or allergy, there is no evidence that any food or type of diet has an impact upon the prevalence of asthma after early infancy. If indeed there is such an impact, it is likely to be confined to the window of opportunity during the prenatal stage and the first months of life – a critical period when it is still possible to modulate the growth and development of the respiratory, digestive and immune systems, with repercussions for the rest of life. Thus, once the most appropriate preventive measures have been defined, these should be implemented early, during pregnancy and lactation. A possible explanation for the discrepancy between the hypothetical protective effect of certain substances and the absence of effect found in some studies involving supplements of these nutrients may be that such effects are only obtained in situations of deficiency.
Although the data suggest a certain association between diet and the development of asthma, the existing scientific evidence is unable to recommend any primary preventive measure in the general population or in specific population subgroups. Special or restrictive diets in pregnant or nursing women are not indicated. Exclusive breastfeeding for six months is questioned, since solid foods should begin to be introduced at around four months of age. Once the atopic process has started, no nutritional strategies have been found to be effective as secondary or tertiary preventive measures. Longitudinal studies involving dietetic interventions in cohorts of pregnant women or newborn infants could help clarify these issues.
Conflict of interestThe authors have no conflict of interest to declare.