Clinical pharmacists are specialty trained practitioners who provide direct patient care and comprehensive medication management. While the practice model is most well established in the United States, there are clinical pharmacists throughout the world who are improving the care of patients of all ages and in all areas of acute and ambulatory care. This paper reviews the training standards, expected competencies, and contributions of clinical pharmacists.
Clinical pharmacists are licensed practitioners with advanced education and training who practice in all types of patient care settings with a focus on comprehensive medication management. These specialized pharmacists are focused on achieving optimal use of medications, emphasizing dosing, monitoring, identification of adverse effects, and economic efficiency to achieve optimal patient outcomes. Clinical pharmacists are gaining significant attention worldwide as important members of the patient care team for ambulatory and acute care patients. This paper will describe the actual and potential scope of practice of clinical pharmacists throughout the world.
DEFINITION OF CLINICAL PHARMACYThe American College of Clinical Pharmacy is the organization with a primary focus on clinical pharmacist development, advancement, and positioning among other providers, the public, and professional societies. There are over 16,000 members, but many other practitioners practice clinical pharmacy. The definition of clinical pharmacy is a health science discipline where pharmacists provide patient care that optimizes medication therapy and promotes health, wellness, and disease prevention1. Clinical pharmacists practice in all health care settings and utilize in-depth knowledge of medications and disease states to manage medication therapy as part of a multiprofessional team. Clinical pharmacists are responsible and accountable for medication therapy and patient outcomes. They are a primary source of scientifically valid information on the safe, appropriate, and cost-effective use of medications.
While pharmacists may participate in the management of specific medications or individual disease states (e.g. diabetes, hypertension) in collaboration with the care team, the goal for clinical pharmacists is a broader approach or comprehensive medication management (CMM). The definition of CMM is the standard of care that ensures each patient's medications (prescription, non-prescription, supplements, or herbals) are individually assessed to determine if appropriate for the patient, effective for the condition, safe for use with concurrent comorbidities and therapies, and that the patient is able to take them. An individualized care plan defines the goals, monitoring, and intended outcome. The patient is an active participant in the development of a CMM plan, along with other members of the care team. Key elements of CMM will be described in the Standards of Practice Section. The impact of CMM provided by clinical pharmacists in ambulatory settings is under investigation with a goal to determine effective processes and to measure overall patient outcomes. The disease-state specific medication therapy management programs have shown a reduction in frequency of some medication-related problems, including nonadherence, and have lowered some healthcare costs2.
CLINICAL TEAMS DEFINEDThe American College of Physicians has described the clinical care team in the United States as the health professionals-physicians, advanced practice registered nurses, other registered nurses, physician assistants, clinical pharmacists, and other health care professionals-with the training and skills needed to provide high-quality, coordinated care specific to the patient's clinical needs and circumstances3. Support for team-based practice is also provided by the American College of Obstetricians and Gynecologists, the Society of Critical Care Medicine, and other organizations4. While the composition of teams may vary, the responsibility and authority for specific aspects of care are optimally assigned to the person most appropriate for the task. Optimal team effectiveness relies on a culture of trust, shared goals, effective communication and mutual respect. The best interests of the patient should be the driving force for team activities. All team members need not be in a single location and as such the broad group of health professionals certainly includes general practice pharmacists in hospitals, clinics, and retail settings.
While just a single example, patients benefit from team-based care through improved control of BP, and a higher proportion of patients achieved controlled BP when a pharmacist was part of the team5.
The composition of dynamic clinical teams is reflected in the multi-professional nature of large professional organizations such as the Society of Critical Care Medicine, the Society of Hospital Medicine, the American Society of Parenteral and Enteral Nutrition, and the Neurocritical Care Society. Most of these organizations include clinical pharmacists in governance roles, including the presidency.
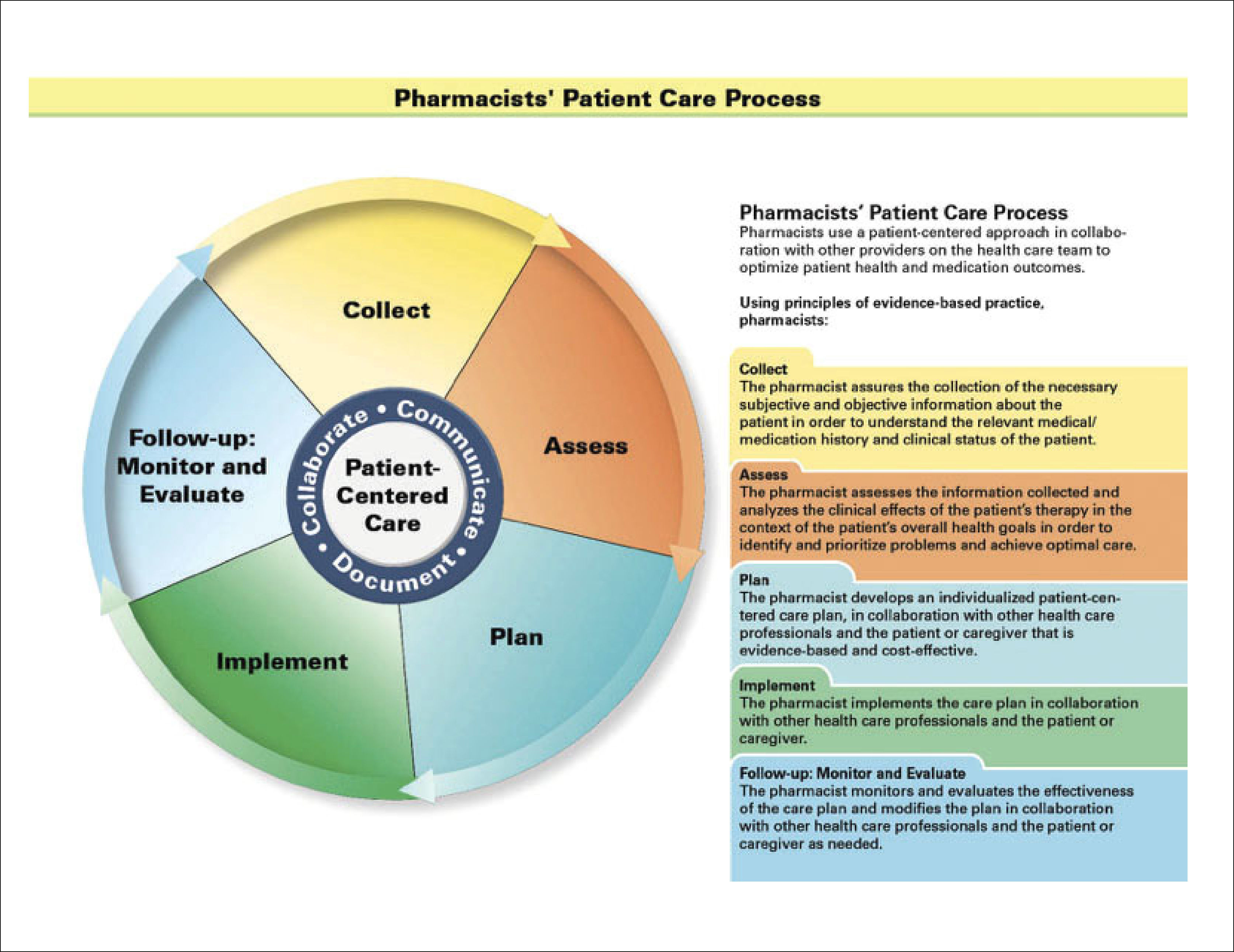
PHARMACIST PROCESS OF CAREPharmacists in the United States are expected to practice in a uniform manner according to the Pharmacist Process of Care published in 2015. This process includes multiple steps in the medication therapy sequence. The steps are illustrated in Figure 1, and include collection of pertinent patient care data, assessment of data relative to patient goals, development of a patient-centered plan, implementation of the care plan for therapy and monitoring, and reassessment and revision of the plan- all in collaboration with the care team6. However, it is realistic to assume that practitioners who were trained many decades ago, and who remain in practice are likely to have a different approach to direct patient care than the younger pharmacists who have been trained this way. However, the POC allows training and job descriptions to be focused on a consistent endpoint and defines the minimal expected activity for all pharmacists in all settings. In medicine, the POC is much more standardized and serves as the model for pharmacy.
The Pharmacist Process of Care
Ref6.
Clinical pharmacists are pharmacy the practitioners who specialize in direct patient care. While they are expected to follow the steps described in the Pharmacist POC, the Standards of Practice (SOP) guide the clinical pharmacist to comprehensively assess medication related needs, and frequently, to manage complex and specialized regimens.7 The documentation requirements are more detailed, and when applicable must be compatible with billing requirements. The clinical pharmacist may practice more independently in some settings, especially as defined by organizational privileges. Clinical pharmacists who have achieved the proper credentials and certification now must obtain hospital privileges like physicians and advanced practice providers. They are required to maintain a valid license, but have additional maintenance of certification requirements. The clinical pharmacist SOP also includes educational activities, scholarly pursuits, and quality improvement.
TRAINING CLINICAL PHARMACISTSPharmacy training varies throughout the world. In the United States (US), a pharmacist is eligible for licensure after 6 years of education and attainment of a Doctor of Pharmacy degree. While not required, many of these graduates already have a Bachelor of Science in another field. Pharmacists who are interested in direct patient care roles can seek additional training in postgraduate year-one (PGY-1) residency programs in acute care or ambulatory care settings. These are broad-based accredited experiences in clinical care, drug information, administration, teaching methods, and project/research over 12 months8. Those interested in specialization can complete a second post-graduate year (PGY-2) residency in areas as diverse as any medical specialty (ambulatory care, critical care, infectious disease, internal medicine, oncology, and many others)9. Additional research fellowship training may follow, especially for those interested in an academic or research role.
Pharmacists who are eligible for licensure in the United States have completed formal training, and many universities are partnering with pharmacy schools outside North America to create clinical pharmacy training opportunities for international students. The training programs in Chile have evolved to include additional clinical experiential training experiences10.
Clinical pharmacists may practice under a formal collaborative practice agreement with physicians in their practice area or as granted by the hospital11. As an example, a pharmacist may modify the dose, frequency, or route of administration of medications covered by a collaborative practice agreement. They may also initiate serum concentration monitoring or order other applicable laboratory tests to monitor the effects of the therapy. Quality assessment has demonstrated the value of these programs,12 Hospitals may require individuals to provide periodic quality assessments or proof of a minimum volume of activity. The laws for pharmacist activities are governed by individual states and local hospital regulation.
BOARD CERTIFICATIONFollowing didactic and experiential training, many clinical pharmacists seek Board of Pharmacy Specialties (BPS) certification13. There are more than 21,000 pharmacists worldwide who are BPS board certified in eight pharmacy specialties: ambulatory care, critical care, nuclear, nutrition support, oncology, pediatric, pharmacotherapy, and psychiatric pharmacy. Future specialty certifications may include infectious disease and cardiology among others. Board certified pharmacists must pass a rigorous examination and then maintain accreditation through continuing education or additional testing every 7 years. Board certification is a typical requirement to achieve privileges for independent or collaborative practice. Aspects of privileging are similar to those used for other medical providers.
CURRENT ROLES/BENEFITS OF CLINICAL PHARMACISTSClinical pharmacists in the US have established roles in many healthcare teams. Most are part of a multiprofessional team for acute care or ambulatory care populations, but some have a private practice upon referral from a broad population of physicians. There are numerous examples of the impact made by clinical pharmacists, and this paper will highlight some recent publications14.
Since medication management is the primary focus, most measurements reflect optimal use of medications and avoidance of adverse events. The broad use of antihypertensive medications may lead to adverse outcomes if doses are not properly titrated. The benefit of clinical pharmacist education, monitoring and intervention was demonstrated in a prospective, randomized study of 800 heart failure or hypertension patients treated at the clinics of a large public hospital15. The patients with clinical pharmacist interventions had a 34% lower risk of any adverse drug event (ADE) or medication error (ME) (risk ratio 0.66, 95% confidence interval [CI], 0.50-0.88) including a significantly lower risk of ADE, preventable ADE, potential ADE, and medication errors compared with control patients treated at the same clinics. Patients with complicated cardiovascular histories had the greatest number of medications and events. Pharmacist interaction, education, and regular communication with the rest of the team improved medication adherence, patient satisfaction, and reduced healthcare utilization and direct costs of care. A systematic review of 12 randomized trials of clinical pharmacist impact on heart failure patients showed similar benefits with a reduced rate of all-cause hospitalization (Odds ratio [OR] 0.71, 95%CI (0.54-0.94) and heart failure hospitalization rate OR 0.69, 95%CI (0.51-0.94)16. Other reviews have described additional benefits of clinical pharmacist monitoring and interventions on a variety of treatment endpoints (blood pressure, lipid profile, weight, and glycemic control)17. The American College of Cardiology has endorsed a strategy of team-based care, including clinical pharmacists18.
Clinical pharmacists on medical inpatient acute care teams have been shown to reduce preventable adverse drug events by 78%19. A clinical pharmacist who rounded with a critical care team more effectively identified and prevented more adverse drug events than pharmacists involved in order entry and verification, and avoided the potential expenditure of over $210,000 in 4.5 months.20 A review of 36 studies describing the impact of clinical pharmacists on hospital inpatients suggests that the addition of a clinical pharmacist to the acute care team resulted in improved care, with no evidence of harm.21 Interacting with the team on rounds, interviewing patients, reconciling medications from outpatient to inpatient, patient discharge education, and follow-up all resulted in improved outcomes. Highest risk patients such as the very elderly, and the very young have been shown to benefit from the presence of and contributions of clinical pharmacists.22,23
INTERNATIONALClinical pharmacists have increased in number throughout the world, and patients have benefited. A survey in 2005 described critical care clinical pharmacist roles in 24 countries outside North America24. The majority 74.4% indicated that they attended medical rounds, almost all (90%) prospectively reviewed drug therapy and intervened to prevent drug interactions, ADE, and to optimize dosing and frequency of administration. Pharmacists in Australia have described medication therapy interventions for hospitalized inpatients and demonstrated their ability to reduce length of stay and over $4 million dollars of annualized hospital cost savings in 8 hospitals25. Over 25% of the interventions were major or life-saving.
Pharmacists in the Netherlands have significantly reduced prescribing errors and related patient harm by their presence on the ward compared with the baseline central pharmacy services26. Pediatric pharmacists in China demonstrated a significant reduction in adverse drug reactions, length of stay, and drug costs compared with a control group of similar patients without a rounding pharmacist27. While these illustrate only a few examples, there are pharmacists providing patient focused interventions throughout the world, including Chile. Clinical pharmacy is growing in popularity, and the University of Chile offers a training program for pharmacists to become Specialists in Clinical Pharmacy and Pharmaceutical Care that is more patient and health-team focused and different from the academically focused Master in Pharmaceutical Science or Doctorate in Pharmacology.
PHARMACIST COMPETENCYStatements have been developed to define the basic competencies of pharmacists in a number of individual countries and also by the International Pharmaceutical Federation28. In Chile, the results of the Pan American Conference on Pharmaceutical Education proposal for basic education and pharmacist competencies include statements that apply to clinical pharmacists- specifically to document patient information and manage pharmacotherapy and follow-up29. Clinical pharmacist or advanced and specialist practice competencies have also been described and summarized30. While the United States has not compiled a single list of competencies for practitioners, a statement describes a general framework and there are training criteria for hospital pharmacists completing residency training that form the foundation for the knowledge and skills expected of a specialist practitioner31,32. In the United Kingdom, the National Health Service has competency statements for pharmacists and also for specialized practitioners33. This advanced to consultant level framework (ACLF) defines level of advanced practice (foundation, excellence, and mastery/consultant) and the competencies required to practice at each level.34 Critical car e pharmacists have developed a peer evaluation process and career advancement program that has resulted in the credentialing of a growing number of practitioners35. Candidates submit a vida voce and practice portfolio to provide evidence of their practice model based on the ACLF competencies. Supporting references, interviews, case-based discussions and peer reviews were included in this rigorous process that serves as a model for other specialty practices.
Health systems in many other countries have similarly developed pharmacist competency statements.
WHAT I DO AS A CLINICAL PHARMACISTAs a critical care pharmacy specialist, it is difficult to describe a typical day, but in general, I am occupied with the elements of the pharmacist process of care throughout my day. I consider myself to be responsible for all aspects of medication management. Each day, I evaluate and assess new patients, and update the progress of prior patients, identify medication related problems and potential problems, develop a problem list and plan of care for optimal dosing based on renal and hepatic function, potential drug interactions, and serum concentrations. I join multiprofessional rounds with the critical care team and ensure implementation of the medication plan by coaching medical residents in proper order entry or by entering orders myself under a collaborative practice agreement and document in the electronic medical record (EMR). A large contribution to medication management is to identify therapies that are no longer needed, thus reducing cost and risk of adverse events and maintaining antimicrobial stewardship programs in conjunction with our infectious disease physicians and pharmacist. I also monitor for achievement of quality measures such as ensuring proper venous thromboembolism prevention, appropriate use of stress gastritis prevention medications, addition of aspirin for troponin elevations related to coronary ischemia, and also by discussing need for central lines and urinary catheters. I educate the team on medication related issues and applicable literature on rounds and in didactic discussions. I am always available for emergency response and resuscitations and to answer mediation-related questions.
For each new patient, a member of the pharmacy team will compile a medication history from electronic records, from the family, the patient, community physicians or pharmacies and document that in the EMR. I will then reconcile that list to determine medication-related causes of admission such as nonadherence or overdose and provide advice on which medications to order to avoid withdrawal reactions or other adverse events. While I have a more limited role in verifying medication orders within the EMR and almost no role in actual drug product dispensing, I serve as a liaison with the technicians and pharmacists who are specialists in parenteral products and distribution systems to ensure that medications are present when needed. Nurses have the enormous task of administering medications, and I facilitate that process by assisting with intravenous compatibility information and education on unfamiliar therapies.
Other aspects of my role include developing quality assessment tools and evaluating data. The EMR is made more efficient by proper design of ordering systems that are efficient and facilitate achievement of quality measures and selection of preferred therapies. I have significant input into these ordering systems in the area of medication therapy and monitoring. I also report adverse drug events. Many adverse events or incidents are related to system-level problems and I regularly advise on potential process improvements in intravenous pumps programming, medication safety systems or other processes.
I direct a critical care pharmacist PGY-2 residency program and monitor the progress of the resident and interactions with other preceptors in our health-system. I participate in multiprofessional journal club discussions, case conferences and quality review meetings. Like other professionals I seek to maintain a role in scholarly contributions to the literature and to maintain competency and be current with the burgeoning literature. As a Board Certified Critical Care Pharmacist, I have a requirement for continuing education and maintenance of certification, and as a licensed pharmacist I must also maintain continuing education.
FUTUREWhile the clinical pharmacy programs are in various stages of development globally the need for specialists with a broad focus on medications and their optimal use is universal. The American College of Clinical Pharmacists has supported these training programs and provided education to individuals and groups. Their publications are used for preparation and maintenance of board certification by pharmacists worldwide. This outreach is expected to continue, as more partners are engaged and more pharmacists and their multiprofessional teams recognize the opportunities for clinical pharmacists to improve patient care.
The author declares no conflicts of interest in relation to this article.