SARS-CoV-2 infection has been associated with multiple short- and long-term complications including depression, and cognitive impairment (CI). However, older adults with CI after COVID-19 have not been fully documented.
ObjectiveTo evaluate cognitive function in Mexican adults post-recovery from SARS-CoV-2 infection.
MethodsIn this prospective observational cohort study, we assess cognitive function (CF) by the Montreal Cognitive Assessment (MOCA) test with a cut-off less than 26 points, and functional status via telemedicine. Eligible patients with a history of moderate–severe COVID-19 aged ≥60 years, cognitively healthy (evaluated by Everyday Cognition Scale) and required admission to an intensive care unit (ICU) were included. Patients with history of dementia, stroke, and delirium during the cognitive evaluation were excluded. The association between CI and COVID-19 was assessed with a Cox regression model.
ResultsFrom the 634 patients admitted to the ICU, 415 survived, afterward 308 were excluded and 107 were analyzed. Mean age was 70 years, 58% were female, and 53% had severe COVID.
The mean MoCA score was 21±5 points, CI was present in 61 patients (57%). Infection severity (RR 1.87; 95% CI: 1.11–3.15, p<0.05), lower education (RR 0.92; 95% CI: 0.87–0.97, p<0.01), and activity daily living disability (RR 1.87; 95% CI: 1.07–3.26, p<0.05) were the main factors associated with CI (unadjusted model by age and sex). The delayed recall, orientation, and language (83.2, 77.6 and 72.9% respectively) domains were the most affected in patients with CI.
ConclusionsFifty-seven percent of patients analyzed developed CI six months post-ICU discharge due to SARS-CoV-2, and COVID severity was the main factor associated to its outcome.
La infección por el virus SARS-CoV-2 se ha asociado con múltiples complicaciones a corto y largo plazo, como depresión y deterioro cognitivo (DC). Sin embargo, los adultos mayores con DC posterior a la covid-19 no han sido completamente estudiados.
ObjetivoEvaluar la función cognitiva en adultos mexicanos recuperados de la infección por SARS-CoV-2.
MétodosEn este estudio de cohorte observacional prospectivo, evaluamos la función cognitiva mediante la prueba de Evaluación Cognitiva de Montreal (MoCa) con punto de corte menor a 26 puntos y una breve evaluación geriátrica a través de telemedicina. Se incluyó a pacientes elegibles con antecedentes de covid-19 moderado-grave con edad ≥60 años, cognitivamente sanos (evaluados por la escala Everyday Cognition) y que requirieron atención en la unidad de cuidados intensivos. Se excluyó a los pacientes con antecedentes de demencia, accidente cerebrovascular y delirium durante la evaluación cognitiva. La asociación entre función cognitiva y covid-19 se evaluó con un modelo de regresión de Cox.
ResultadosDe los 634 pacientes ingresados en la UCI, 415 sobrevivieron; posteriormente 308 fueron excluidos y 107 analizados. La edad media fue de 70 años, el 58% eran mujeres y el 53% cursó con covid grave. La puntuación MoCA media fue de 21±5 puntos, el DC estuvo presente en 61 pacientes. La gravedad de la infección (RR 1,87; IC95%: 1,11-3,15; p<0,05), menor nivel educativo (RR 0,92; IC95%: 0,87-0,97; p<0,01) y discapacidad en la actividad de la vida diaria (RR 1,87; IC95%: 1,07-3,26; p<0,05) fueron los principales factores asociados al DC (modelo no ajustado por edad y sexo). Los dominios de recuerdo tardío, orientación y lenguaje (83,2; 77,6 y 72,9%, respectivamente) fueron los más afectados en pacientes con DC.
ConclusiónEl 57% de los pacientes desarrollaron deterioro cognitivo 6 meses después del alta de la UCI por SARS-CoV-2, y la gravedad de la covid fue el principal factor asociado a este desenlace.
The COVID-19 pandemic has significantly impacted public health worldwide, including mental health. During the acute infection, the presence of delirium, depression, and anxiety appear to be the main risk factors predisposing patients to adverse cognitive outcomes. However, long COVID (fatigue, anxiety, and cognitive impairment) have been documented in young and middle-aged individuals as well, but not sufficiently.1
Current knowledge suggests that viral infections in general lead to chronic inflammation and abnormal immune responses, triggering long-term neuropsychiatric cognition syndromes.2 What cognitive domains and the extent of their involvement remain to be determined in the geriatric population. In a public health context, Mexico City was significantly affected by the COVID-19 pandemic, with a prevalence of 45% and a mortality rate of 29 per 1000 individuals in 2020. Due to the clinical characteristics of Mexican older adults i.e., high cardiovascular comorbidity, diabetes, obesity, etc., they are highly vulnerable to adverse cognitive outcomes.3 Further information on the effects of SARS-CoV-2 infection on cognitive function (CF) in the geriatric population should be fully investigated, given the high mortality rate of COVID-19 infection before the development of COVID-19 vaccines. Hence, a clear understanding of CF in older adults who recovered from SARS-CoV-2 infection is a priority. This study aimed to evaluate CF in older adults who recovered from SARS-CoV-2 infection in a tertiary care center.
2Material and methodsThe nature of the study was a single-center observational cohort, all patients were recruited in a tertiary care hospital in Mexico City. An electronic medical record was used to detect patients above the age of 60, cognitively healthy (per the Everyday Cognition Scale through an informant – primary caregiver or relative –),4 with a history of moderate–severe (by pulmonary involvement on computerized axial tomography) COVID-19, and that required admission to an intensive care unit (ICU) during hospitalization and were discharged between January 1 and August 31, 2021. At the time of cognitive evaluation (6 months after discharge), patients with uncontrolled comorbidities such as renal replacement therapy in chronic kidney disease, chemotherapy in oncological disease, systemic arterial hypertension (based on their control status in the last three months), type-2 diabetes (based on HbA1c in the las three months) and psychiatric disorders, (previous diagnosis of dementia, major depressive disorder uncontrolled, and anxiety symptoms), a history of stroke within the previous 6 months, and terminally ill patients were excluded.
To obtain this information related to the exclusion criteria, it was based on the interview with the patient via telemedicine, as well as the review of their electronic clinical record.
Patients with delirium diagnosed with the Confusion Assessment Method (CAM) during the cognitive evaluation were also excluded.5 The Local Ethics Committee reviewed and approved the study and written informed consent was obtained from all participants.
2.1Clinical and cognitive assessmentCOVID-19 was diagnosed according to the guidelines proposed by the World Health Organization.6 The severity disease was defined by the grade of pulmonary involvement in computerized axial tomography (CT) imaging criteria as suggested by the European Society of Radiology (ESR)/European Society of Thoracic Imaging (ESTI).7 Considering the health contingency, determining whether patients fulfilled inclusion/exclusion criteria was conducted by telephone in all study patients invited to participate. Subsequently, a brief geriatric evaluation was performed using telemedicine (6 months after discharge), which consisted of video calls sessions through the zoo platform, using hospital computing equipment. These telemedicine sessions, clinical characteristics such as functional status according to the Activities of Daily Living (ADAL) scale, depressive symptoms per the Geriatric Depression Scale (GDS), and the establishment of current comorbidities were evaluated. At the same time as the brief geriatric assessment, a cognitive evaluation was performed by telemedicine using the Montreal Cognitive Assessment (MoCA) and its cognitive domains (visuospatial/executive, naming, memory, attention, language, abstraction, delayed recall, and orientation) 6 months after hospital discharge. To establish abnormality in the performance of the MoCA test, a score of less than 26 points was used as the cut-off point.8 Due to the lack of pre-infection cognitive information, the Everyday Cognition Scale (ECog) was used as a proxy (through a primary caregiver) to evaluate cognitive performance through activities of daily living 10 years prior to infection. These evaluations were applied by geriatricians trained by an expert neuropsychologist in cognitive impairment. The definition of cognitive impairment (dependent variable) was based on patient performance in the MoCA using normative data obtained from the Mexican older adult population. SARS-CoV-2 infection severity was considered the independent variable based on the presence or lack of CT imaging-compatible changes, and the need for ICU care.
2.2Statistical analysisA descriptive and multivariate analysis based on the characteristics of the variables was conducted. The Student's t-test was used for continuous variables, and categorical variables were analyzed with the χ2 or Fisher's exact test. Continuous variables, including age, education, body mass index, were not normally distributed, thus Mann–Whitney U tests were used. Evaluation of the cognitive domains of both the MoCA and the ECog, z-scores were used. Cognitive function was evaluated 6 months after hospital discharge with a Cox proportional hazard model, adjusted for age and sex (potential confounding effects) to identify an association between impaired CF and SARS-CoV-2 infection; 95% confidence intervals (95% CI) were obtained, and a p-value below or equal to 0.05 was considered significant. Statistical analyses were conducted with the SPSS statistical package, version 25 (IBM SPSS Statistics for iOS, Armonk, NY, USA).
3ResultsIn total, 634 older adults were studied, these patients were hospitalized due SARS-CoV-2 infection between January and August 2022. At time of cognitive evaluation (6 months after hospital discharge) 415 patients still survived; of them, 308 (74%) were excluded due fulfilling the exclusion criteria, at the end 107 patients were included in the final analysis. The mean age of participants was 70±7.3 years. Sixty-one patients showed cognitive impairment (MoCA abnormal). Most were females (58%), with an average education level of 9.8±5.3 years, and an ECog mean score of 52±16 points (all the patients were included in the final analysis).
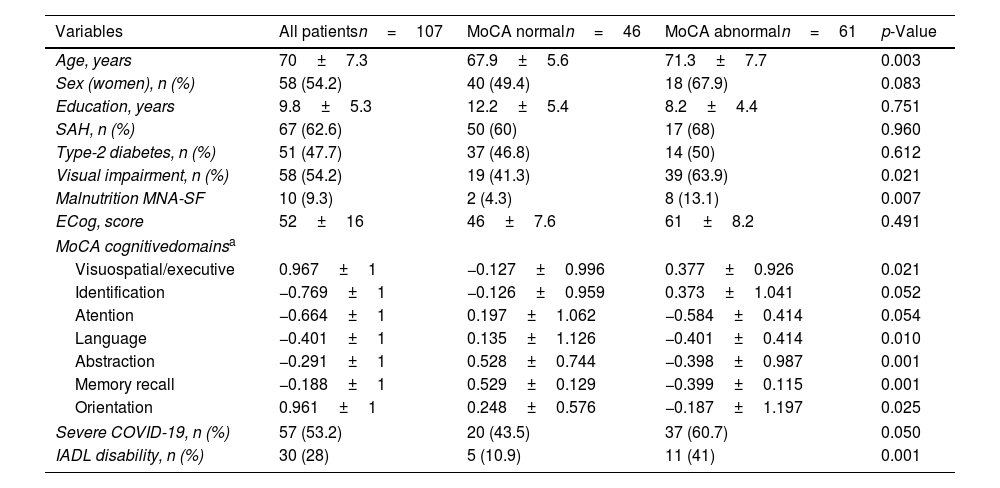
CT imaging revealed that 53% (57 patients) of the analyzed population had harbored severe infection, particularly in cases with subsequent CF impairment (37 patients) vs no CF impairment (20 patients) (p=0.05); 43.5% of patients with no CF impairment had developed a severe COVID-19 (Table 1).
Sociodemographic and clinical characteristics.
| Variables | All patientsn=107 | MoCA normaln=46 | MoCA abnormaln=61 | p-Value |
|---|---|---|---|---|
| Age, years | 70±7.3 | 67.9±5.6 | 71.3±7.7 | 0.003 |
| Sex (women), n (%) | 58 (54.2) | 40 (49.4) | 18 (67.9) | 0.083 |
| Education, years | 9.8±5.3 | 12.2±5.4 | 8.2±4.4 | 0.751 |
| SAH, n (%) | 67 (62.6) | 50 (60) | 17 (68) | 0.960 |
| Type-2 diabetes, n (%) | 51 (47.7) | 37 (46.8) | 14 (50) | 0.612 |
| Visual impairment, n (%) | 58 (54.2) | 19 (41.3) | 39 (63.9) | 0.021 |
| Malnutrition MNA-SF | 10 (9.3) | 2 (4.3) | 8 (13.1) | 0.007 |
| ECog, score | 52±16 | 46±7.6 | 61±8.2 | 0.491 |
| MoCA cognitivedomainsa | ||||
| Visuospatial/executive | 0.967±1 | −0.127±0.996 | 0.377±0.926 | 0.021 |
| Identification | −0.769±1 | −0.126±0.959 | 0.373±1.041 | 0.052 |
| Atention | −0.664±1 | 0.197±1.062 | −0.584±0.414 | 0.054 |
| Language | −0.401±1 | 0.135±1.126 | −0.401±0.414 | 0.010 |
| Abstraction | −0.291±1 | 0.528±0.744 | −0.398±0.987 | 0.001 |
| Memory recall | −0.188±1 | 0.529±0.129 | −0.399±0.115 | 0.001 |
| Orientation | 0.961±1 | 0.248±0.576 | −0.187±1.197 | 0.025 |
| Severe COVID-19, n (%) | 57 (53.2) | 20 (43.5) | 37 (60.7) | 0.050 |
| IADL disability, n (%) | 30 (28) | 5 (10.9) | 11 (41) | 0.001 |
Abbreviations: SAH, systemic arterial hypertension; ECog, Everyday Cognition Scale; GDS, Geriatric Depression Scale; MoCA, Montreal Cognitive Assessment; MNA-SF, Mini Nutritional Assessment-Short Form; IADLs, Instrumental Activities of Daily Living scale.
In the analyzed population, 61 patients (57%) had CF impairment per the MoCA test (mean score: 22.3±5.6). The average age of patients with impaired CF was greater than that of patients without CF compromise (67.9±5.6 vs 71.3±7.7 years; p<0.01). We specifically detected cognitive impairment in the visuospatial/executive (67.3 vs 32.7%, p<0.05), language (72.9 vs 27.1% p<0.05), abstraction (57 vs 43%, p<0.05), delayed recall (83.2 vs 16.8%, p<0.01), and orientation (77.6 vs 22.4%, p<0.05) domains. Also, disability in ADLs was significantly associated with altered CF (p<0.01). From the interview with the family member regarding the cognitive impairment prior to the severe COVID-19 infection, 56% reported that they were without alteration, while 43.9% commented that they had presented alteration in daily activities mediated by cognition (this population was included in the final analysis).
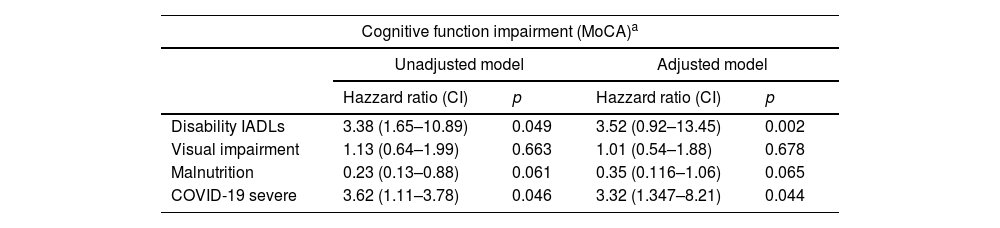
3.2Associated factorsThe ADL disability score (HR 3.38; 95% CI 1.65–10.89, p<0.05), and the severity of COVID-19 (HR 3.62; 95% CI 1.11–3.78, p<0.05) were the main factors associated with CF impairment at 6 months of hospital discharge in the unadjusted model. After adjustment (age, sex, and education) the severity of COVID-19 (HR 3.32; 95% CI 1.34–8.21, p<0.05) was the most significantly factor associated with CF impairment (Table 2).
Cox proportional-hazards model between cognitive function and risk factors.
| Cognitive function impairment (MoCA)a | ||||
|---|---|---|---|---|
| Unadjusted model | Adjusted model | |||
| Hazzard ratio (CI) | p | Hazzard ratio (CI) | p | |
| Disability IADLs | 3.38 (1.65–10.89) | 0.049 | 3.52 (0.92–13.45) | 0.002 |
| Visual impairment | 1.13 (0.64–1.99) | 0.663 | 1.01 (0.54–1.88) | 0.678 |
| Malnutrition | 0.23 (0.13–0.88) | 0.061 | 0.35 (0.116–1.06) | 0.065 |
| COVID-19 severe | 3.62 (1.11–3.78) | 0.046 | 3.32 (1.347–8.21) | 0.044 |
Abbreviations: MoCA, Montreal Cognitive Assessment; CI, confidence interval; IADLs, Instrumental Activities of Daily Living scale.
We established that COVID-19 patients presented cognitive impairment 6 months after recovery, suggesting that SARS-CoV-2 infection compromises cognitive function in the long-term, specifically in older patients who survived to moderate–severe COVID-19. The effect of SARS-CoV-2 infection on cognitive function has become increasingly evident, particularly in severely ill older adults; aside from their age and comorbidities.9 Among the cognitive domains most affected in this study was visuospatial and executive function, this ties in with findings in other studies where these domains have also been impaired in patients with severe COVID-19. Recently, a cross-sectional study evaluated the cognitive function of older adults 6 months after recovery from COVID-19 in Wuhan, China; they were also assessed via a telephone interview. This study also revealed that SARS-CoV-2 infection was associated with an increased risk of long-term cognitive impairment in severely ill patients.10 Another study showed that patients who survived SARS-CoV-2 infection had cognitive impairment at the medium-term, with the executive function domain being the most involved after hospital discharge.11
Several mechanisms that could account for the impact of COVID-19 on cognitive function are proposed, one of them is that the viral systemic inflammatory response may further accelerate the pathogenesis of an underlying neurodegenerative pathology, e.g., Alzheimer disease. It is proposed to link due to its inflammatory response, causing hyperphosphorylation of the tau protein and, on the other hand, the mechanism related to the oxidation of the ryanodine receptor/calcium release channels in the reticulum endo/sarcoplasmic brain cells.12
Other possibly involved mechanisms include hypoxemia and ischemia, particularly in the acute phase of the disease, oxygen deficiency plays a key role at the neuronal level since some brain regions such as the hippocampus are highly susceptible to hypoxic/ischemic injury.13 None of the mechanisms previously exposed has been shown by itself to elucidate the pathophysiology of cognitive impairment, suggesting a multifactorial role in this context.
There are important limitations in this study. The first is the lack of pre-COVID-19 cognitive assessment does not allow objective comparisons of pre-and post-infection cognitive status. Second, we did not include a group of patients with non-COVID-19 pneumonia. Third, the MOCA and CAM tool have not been validated for remote telemedicine use. However, the strengths of the study lie in its prospective design and its specific analysis of an older adult's Mexican population, in which we determined the impact of COVID-19 on cognitive function. Our results suggest that SARS-CoV-2 infection had a negative impact on cognitive function in recovered older adults. These patients must undergo long-term follow-up to further characterize their cognitive function, particularly in those previously affected by severe COVID-19.
5Conflict of interestThe authors declare no conflict of interest.
We are grateful for the support provided by Alberto Avila-Funes PhD and Gerontology service of the INCMNSZ, Belén Carolina Lara-Serrano, and Karla Marlen Martínez-Juárez.